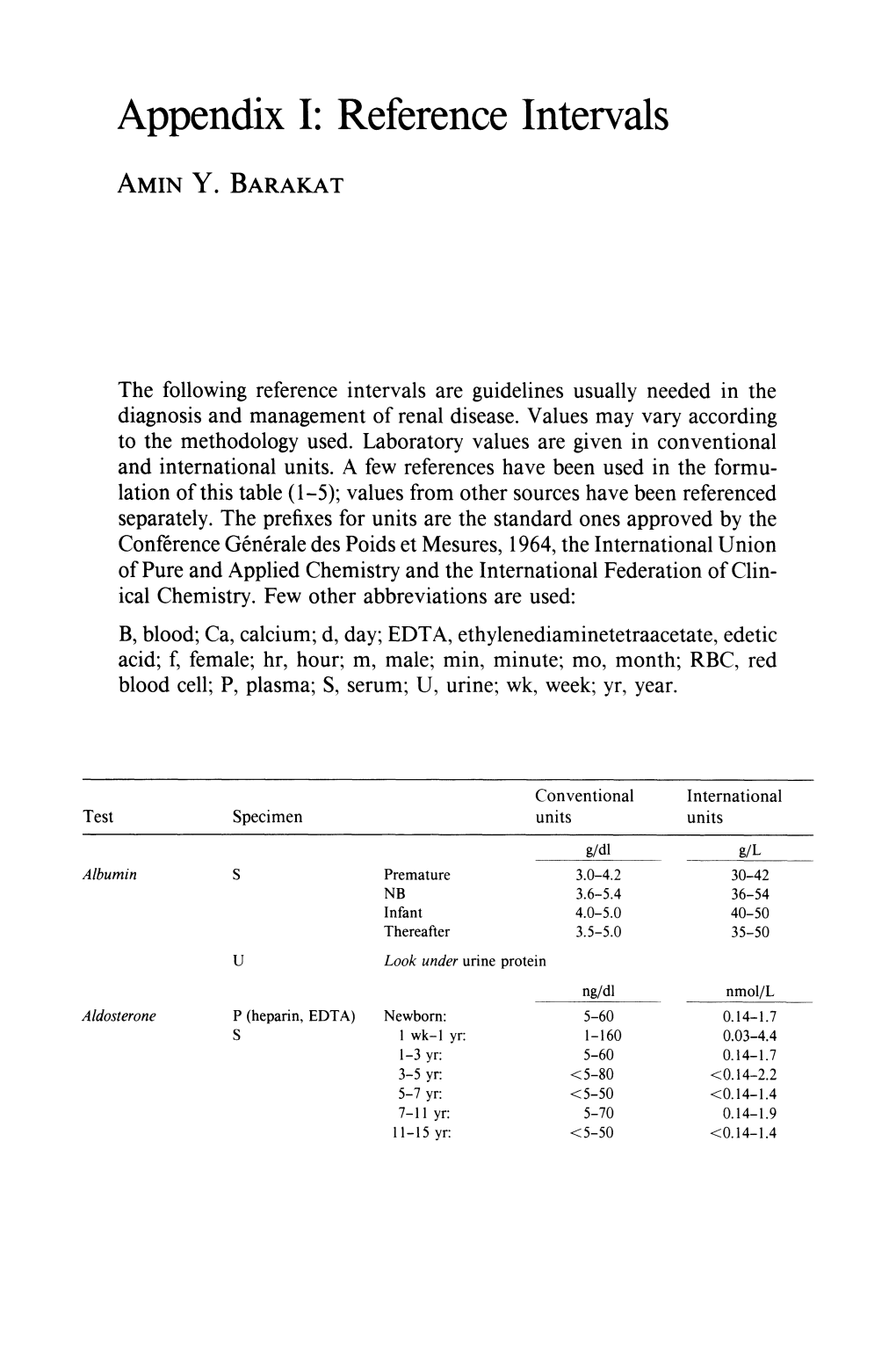
Appendix I: Reference Intervals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Leading Article the Molecular and Genetic Base of Congenital Transport
Gut 2000;46:585–587 585 Gut: first published as 10.1136/gut.46.5.585 on 1 May 2000. Downloaded from Leading article The molecular and genetic base of congenital transport defects In the past 10 years, several monogenetic abnormalities Given the size of SGLT1 mRNA (2.3 kb), the gene is large, have been identified in families with congenital intestinal with 15 exons, and the introns range between 3 and 2.2 kb. transport defects. Wright and colleagues12 described the A single base change was identified in the entire coding first, which concerns congenital glucose and galactose region of one child, a finding that was confirmed in the malabsorption. Subsequently, altered genes were identified other aZicted sister. This was a homozygous guanine to in partial or total loss of nutrient absorption, including adenine base change at position 92. The patient’s parents cystinuria, lysinuric protein intolerance, Menkes’ disease were heterozygotes for this mutation. In addition, it was (copper malabsorption), bile salt malabsorption, certain found that the 92 mutation was associated with inhibition forms of lipid malabsorption, and congenital chloride diar- of sugar transport by the protein. Since the first familial rhoea. Altered genes may also result in decreased secretion study, genomic DNA has been screened in 31 symptomatic (for chloride in cystic fibrosis) or increased absorption (for GGM patients in 27 kindred from diVerent parts of the sodium in Liddle’s syndrome or copper in Wilson’s world. In all 33 cases the mutation produced truncated or disease)—for general review see Scriver and colleagues,3 mutant proteins. -

Characteristics of Presentation and Metabolic Risk Factors in Relation to Extent of Involvement in Infants with Nephrolithiasis
DOI: 10.14744/ejmi.2019.87741 EJMI 2020;4(1):78–85 Research Article Characteristics of Presentation and Metabolic Risk Factors in Relation to Extent of Involvement in Infants with Nephrolithiasis Kenan Yilmaz,1 Mustafa Erman Dorterler2 1Department of Pediatric Nephrolog, Sanliurfa Training and Research Hospital, Sanliurfa, Turkey 2Department of Pediatric Surgery, Harran University Faculty of Medicine, Sanliurfa, Turkey Abstract Objectives: To evaluate the characteristics of presentation and metabolic risk factors in relation to the extent of in- volvement in infants with nephrolithiasis. Methods: A total of 111 infants (age range 0.3–11.8 months, 58.6% were girls) diagnosed with nephrolithiasis in the first year of life were included in this retrospective study. Data on age at diagnosis, gender, family history of nephrolithiasis, parental consanguinity, symptoms on admission, urinary abnormalities, surgery, size of renal calculi, and metabolic risk factors (hypercalciuria, hyperuricosuria, hyperoxaluria, hypocitraturia, cystinuria, hypercalcemia) were recorded for each patient and compared with the number of kidneys affected (bilateral vs. unilateral), the number of kidney stones (multiple vs. single), and the kidney stone size (microlithiasis vs. larger stones). Results: Overall, 58.6% of the infants were girls. Irritability was the most common symptom on admission (34.2%). Microlithiasis (62.2%), bilateral kidney involvement (61.3%), multiple kidney stones (73.9%), and metabolic risk fac- tors (45.0%, hypercalciuria in 31.5%) were commonly noted. Bilateral nephrolithiasis was associated with significantly higher rates of hypercalciuria than unilateral nephrolithiasis (39.7% vs. 18.6%, respectively; p=0.022). The presence of multiple kidney stones was associated with a significantly higher rate of hyperuricosuria than the presence of a single kidney stone (20.7% vs. -

Thomas Addis (1881—1949): Mixing Patients, Rats, and Politics
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Kidney International, Vol. 37 (1990), pp. 833—840 HISTORICAL ARCHIVE CARL W. GOi-FSCHALK, EDITOR Thomas Addis (1881—1949): Mixing patients, rats, and politics STEVEN J. PEITZMAN Department of Medicine, Division of Nephrology and Hypertension, The Medical College of Pennsylvania, Philadelphia, Pennsylvania, USA In the early decades of the twentieth century, with the threatat the Laboratory of the Royal College of Physicians of Edin- of epidemic infectious diseases already in decline, attentionburgh, one of Great Britain's pioneering medical research shifted to the chronic maladies: hypertension, atherosclerosis,enterprises, also supported by the Carnegie Trusts. obesity, cancer, diabetes—and nephritis, or Bright's disease. Ray Lyman Wilbur (1875—1949), dean of the young Stanford New chemical methods devised by Otto Folin (1867—1934) atMedical School in 1911, "thought it would be a good thing to Harvard and Donald D. Van Slyke (1883—1971) at the Rock-bring in a young scientist from Scotland if the right one could be efeller Institute Hospital empowered the investigation of renalfound who had been trained in German as well as British and metabolic disorders. Folin's colorimetric system provideduniversities, and who was likely to develop in some promising rapid measurement of creatinine, urea, and uric acid, while Vanfield of research" [3]. So Wilbur sent a cable of invitation to Slyke's gasometric analyses allowed quantification of urea andEdinburgh, and the young Scotsman accepted the unlikely total carbon dioxide. Also in the first decades of the twentiethposition: in 1911 Stanford was still a relatively isolated and century, the reform of medical schools provided new opportu-little-known medical school in San Francisco (the school moved nities for academic medical careers. -

Acute Kidney Injury in Cancer Patients
Acute kidney injury in cancer patients Bruno Nogueira César¹ Marcelino de Souza Durão Júnior¹ ² 1. Disciplina de Nefrologia, Universidade Federal de São Paulo, São Paulo, SP, Brasil 2. Unidade de Transplante Renal Hospital Israelita Albert Einstein, São Paulo, SP, Brasil http://dx.doi.org/10.1590/1806-9282.66.S1.25 SUMMARY The increasing prevalence of neoplasias is associated with new clinical challenges, one of which is acute kidney injury (AKI). In addition to possibly constituting a clinical emergency, kidney failure significantly interferes with the choice and continuation of antineoplastic therapy, with prognostic implications in cancer patients. Some types of neoplasia are more susceptible to AKI, such as multiple myeloma and renal carcinoma. In cancer patients, AKI can be divided into pre-renal, renal (intrinsic), and post-renal. Conventional platinum-based chemotherapy and new targeted therapy agents against cancer are examples of drugs that cause an intrinsic renal lesion in this group of patients. This topic is of great importance to the daily practice of nephrologists and even constitutes a subspecialty in the field, the onco-nephrology. KEYWORDS: Acute Kidney Injury. Neoplasia. Malignant tumor. Chemotherapy. INTRODUCTION With the epidemiological transition of recent de- (CT), compromises the continuation of treatment, cades, cancer has become the object of several clini- and limits the participation of patients in studies cal studies that resulted in more options for the diag- with new drugs. nosis and treatment of the disease. Thus, there was an increase in the survival of patients, and handling EPIDEMIOLOGY complications of the disease and treatment adverse effects also became more common1. -

Simplified Quantitative Methods for Bacteriuria and Pyuria
J Clin Pathol: first published as 10.1136/jcp.16.1.32 on 1 January 1963. Downloaded from J. clin. Path. (1963), 16, 32 Simplified quantitative methods for bacteriuria and pyuria JAMES McGEACHIE AND ARTHUR C. KENNEDY From the University Departments of Bacteriology and Medicine, Royal Infirmary, Glasgow SYNOPSIS Although pyelonephritis is a common disease, it escapes clinical detection in an un- desirably high proportion of patients. The present unsatisfactory diagnostic position would be much improved by widespread screening of patients by simple yet reasonably accurate methods. Bacterial counts by the pour-plate technique and estimates of the white cell excretion per hour or day, while undoubtedly of diagnostic value, are probably unsuitable for use on a wide scale. In an attempt to find more convenient procedures a simplified stroke-plate method of bacterial counting and a simplified quantitative white cell count method were devised and applied to over 1,000 mid-stream urine samples from 398 patients. Good correlation was obtained between the simpler stroke-plate method of bacterial counting and the more time-consuming pour-plate method. The quantitative white cell procedure was a much more sensitive index of pyuria than wet-film micro- scopy, and comparison with the bacterial count results showed that it gave a useful indication of urinary infection. It is suggested that a quantitative bacterial count should replace non-quantitativecopyright. culture methods when urinary infection is suspected and that the quantitative white cell count should be performed as a routine part of the initial clinical and laboratory assessment of all patients, followed by a bacterial count if pyuria is revealed. -

High Urinary Calcium Excretion and Genetic Susceptibility to Hypertension and Kidney Stone Disease
High Urinary Calcium Excretion and Genetic Susceptibility to Hypertension and Kidney Stone Disease Andrew Mente,* R. John D’A. Honey,† John M. McLaughlin,* Shelley B. Bull,* and Alexander G. Logan* *Prosserman Centre for Health Research, Samuel Lunenfeld Research Institute, Mount Sinai Hospital, and Department of Public Health Sciences, and †St. Michael’s Hospital, Division of Urology, Department of Surgery, University of Toronto, Toronto, Ontario, Canada Increased urinary calcium excretion commonly is found in patients with hypertension and kidney stone disease (KSD). This study investigated the aggregation of hypertension and KSD in families of patients with KSD and hypercalciuria and explored whether obesity, excessive weight gain, and diabetes, commonly related conditions, also aggregate in these families. Consec- utive patients with KSD, aged 18 to 50 yr, were recruited from a population-based Kidney Stone Center, and a 24-h urine and their spouse were interviewed by telephone (333 ؍ sample was collected. The first-degree relatives of eligible patients (n to collect demographic and health information. Familial aggregation was assessed using generalized estimating equations. Multivariate-adjusted odds ratios (OR) revealed significant associations between hypercalciuria in patients and hypertension (OR 2.9; 95% confidence interval 1.4 to 6.2) and KSD (OR 1.9; 95% confidence interval 1.03 to 3.5) in first-degree relatives, specifically in siblings. No significant associations were found in parents or spouses or in patients with hyperuricosuria. Similarly, no aggregation with other conditions was observed. In an independent study of siblings of hypercalciuric patients with KSD, the adjusted mean fasting urinary calcium/creatinine ratio was significantly higher in the hypertensive siblings compared with normotensive siblings (0.60 ؎ 0.32 versus 0.46 ؎ 0.28 mmol/mmol; P < 0.05), and both sibling groups had significantly higher values than the unselected study participants (P < 0.001). -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Inherited Renal Tubulopathies—Challenges and Controversies
G C A T T A C G G C A T genes Review Inherited Renal Tubulopathies—Challenges and Controversies Daniela Iancu 1,* and Emma Ashton 2 1 UCL-Centre for Nephrology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF, UK 2 Rare & Inherited Disease Laboratory, London North Genomic Laboratory Hub, Great Ormond Street Hospital for Children National Health Service Foundation Trust, Levels 4-6 Barclay House 37, Queen Square, London WC1N 3BH, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-2381204172; Fax: +44-020-74726476 Received: 11 February 2020; Accepted: 29 February 2020; Published: 5 March 2020 Abstract: Electrolyte homeostasis is maintained by the kidney through a complex transport function mostly performed by specialized proteins distributed along the renal tubules. Pathogenic variants in the genes encoding these proteins impair this function and have consequences on the whole organism. Establishing a genetic diagnosis in patients with renal tubular dysfunction is a challenging task given the genetic and phenotypic heterogeneity, functional characteristics of the genes involved and the number of yet unknown causes. Part of these difficulties can be overcome by gathering large patient cohorts and applying high-throughput sequencing techniques combined with experimental work to prove functional impact. This approach has led to the identification of a number of genes but also generated controversies about proper interpretation of variants. In this article, we will highlight these challenges and controversies. Keywords: inherited tubulopathies; next generation sequencing; genetic heterogeneity; variant classification. 1. Introduction Mutations in genes that encode transporter proteins in the renal tubule alter kidney capacity to maintain homeostasis and cause diseases recognized under the generic name of inherited tubulopathies. -

Article Twenty-Four Hour Urine Testing and Prescriptions For
CJASN ePress. Published on November 11, 2019 as doi: 10.2215/CJN.03580319 Article Twenty-Four Hour Urine Testing and Prescriptions for Urinary Stone Disease–Related Medications in Veterans Shen Song,1 I-Chun Thomas,2 Calyani Ganesan,1 Ericka M. Sohlberg ,3 Glenn M. Chertow,1 Joseph C. Liao,2,3 Simon Conti,2,3 Christopher S. Elliott,3,4 Alan C. Pao,1,2,3 and John T. Leppert1,2,3 Abstract Background and objectives Current guidelines recommend 24-hour urine testing in the evaluation and treatment 1Division of of persons with high-risk urinary stone disease. However, how much clinicians use information from 24-hour Nephrology, urine testing to guide secondary prevention strategies is unknown. We sought to determine the degree to which Departments of clinicians initiate or continue stone disease–related medications in response to 24-hour urine testing. Medicine and 3Urology, Stanford Design, setting, participants, & measurements We examined a national cohort of 130,489 patients with incident University School of Medicine, Stanford, urinary stone disease in the Veterans Health Administration between 2007 and 2013 to determine whether California; 2Veterans prescription patterns for thiazide diuretics, alkali therapy, and allopurinol changed in response to 24-hour urine Affairs Palo Alto testing. Health Care System, Palo Alto, California; 4 fi and Division of Results Stone formers who completed 24-hour urine testing (n=17,303; 13%) were signi cantly more likely to be Urology, Santa Clara prescribed thiazide diuretics, alkali therapy, and allopurinol compared with those who did not complete a 24-hour Valley Medical Center, urine test (n=113,186; 87%). -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

Acute Kidney Injury and Chronic Kidney Disease: Classifications and Interventions for Children and Adults Teresa V
Acute Kidney Injury and Chronic Kidney Disease: Classifications and Interventions for Children and Adults Teresa V. Lewis, PharmD, BCPS Assistant Professor of Pharmacy Practice University of Oklahoma College of Pharmacy Adjunct Assistant Professor of Pediatrics University of Oklahoma College of Medicine 1 Disclosures • Teresa V. Lewis, Pharm.D., BCPS • Nothing to disclose Objectives 1. When given specific patient details, identify those with increased Identify which adult or pediatric patients are at risk for development of acute kidney injury (AKI) and recommend appropriate preventive interventions. 2. Design an evidence-based plan to manage AKI for a given patient. 3. Compare and contrast the RIFLE, pRIFLE, and Kidney Disease Improving Global Outcomes (KDIGO) classification systems for AKI. 4. List risk factors for development of chronic kidney disease (CKD). 5. Compare and contrast the Kidney Disease Outcomes Quality Initiative (KDOQI) staging of CKD with the Kidney Disease Improving Global Outcomes (KDIGO) CKD staging criteria. 6. Design an evidence-based plan to prevent progression of CKD for a given patient. 3 Kidney Development and Maturation • Nephrogenesis • Begins around 9 weeks of gestation • Complete by 36 weeks of gestation • Immature renal function at birth • Lower renal blood flow • Immature glomeruli • Immature renal tubule function • Kidney function will be similar to adult values by age 2 years 4 Presentation Outline • Diagnostic Workup • Acute Kidney Injury • Drug Induced Nephrotoxicity • Chronic Kidney Disease 5 DIAGNOSTIC WORK-UP Blood Urea Nitrogen (BUN) • Normal: 8-20 mg/dL • Amino-acids metabolized to ammonia and converted in liver to urea • Urea is filtered and reabsorbed in proximal tubule (dependent on water reabsorption) • Normal BUN:Serum creatinine (Scr) ratio is 10-15:1 • Elevated BUN:Scr ratio suggests true or effective volume depletion 7 Serum Creatinine (Scr) • Freely filtered • Actively secreted • Scr lags behind glomerular filtration rate (GFR) by 1-2 days due to: 1. -

Distribution of Glucose Transporters in Renal Diseases Leszek Szablewski
Szablewski Journal of Biomedical Science (2017) 24:64 DOI 10.1186/s12929-017-0371-7 REVIEW Open Access Distribution of glucose transporters in renal diseases Leszek Szablewski Abstract Kidneys play an important role in glucose homeostasis. Renal gluconeogenesis prevents hypoglycemia by releasing glucose into the blood stream. Glucose homeostasis is also due, in part, to reabsorption and excretion of hexose in the kidney. Lipid bilayer of plasma membrane is impermeable for glucose, which is hydrophilic and soluble in water. Therefore, transport of glucose across the plasma membrane depends on carrier proteins expressed in the plasma membrane. In humans, there are three families of glucose transporters: GLUT proteins, sodium-dependent glucose transporters (SGLTs) and SWEET. In kidney, only GLUTs and SGLTs protein are expressed. Mutations within genes that code these proteins lead to different renal disorders and diseases. However, diseases, not only renal, such as diabetes, may damage expression and function of renal glucose transporters. Keywords: Kidney, GLUT proteins, SGLT proteins, Diabetes, Familial renal glucosuria, Fanconi-Bickel syndrome, Renal cancers Background Because glucose is hydrophilic and soluble in water, lipid Maintenance of glucose homeostasis prevents pathological bilayer of plasma membrane is impermeable for it. There- consequences due to prolonged hyperglycemia or fore, transport of glucose into cells depends on carrier pro- hypoglycemia. Hyperglycemia leads to a high risk of vascu- teins that are present in the plasma membrane. In humans, lar complications, nephropathy, neuropathy and retinop- there are three families of glucose transporters: GLUT pro- athy. Hypoglycemia may damage the central nervous teins, encoded by SLC2 genes; sodium-dependent glucose system and lead to a higher risk of death.