Secondary Metabolites Profiled in Cannabis Inflorescences, Leaves
Total Page:16
File Type:pdf, Size:1020Kb
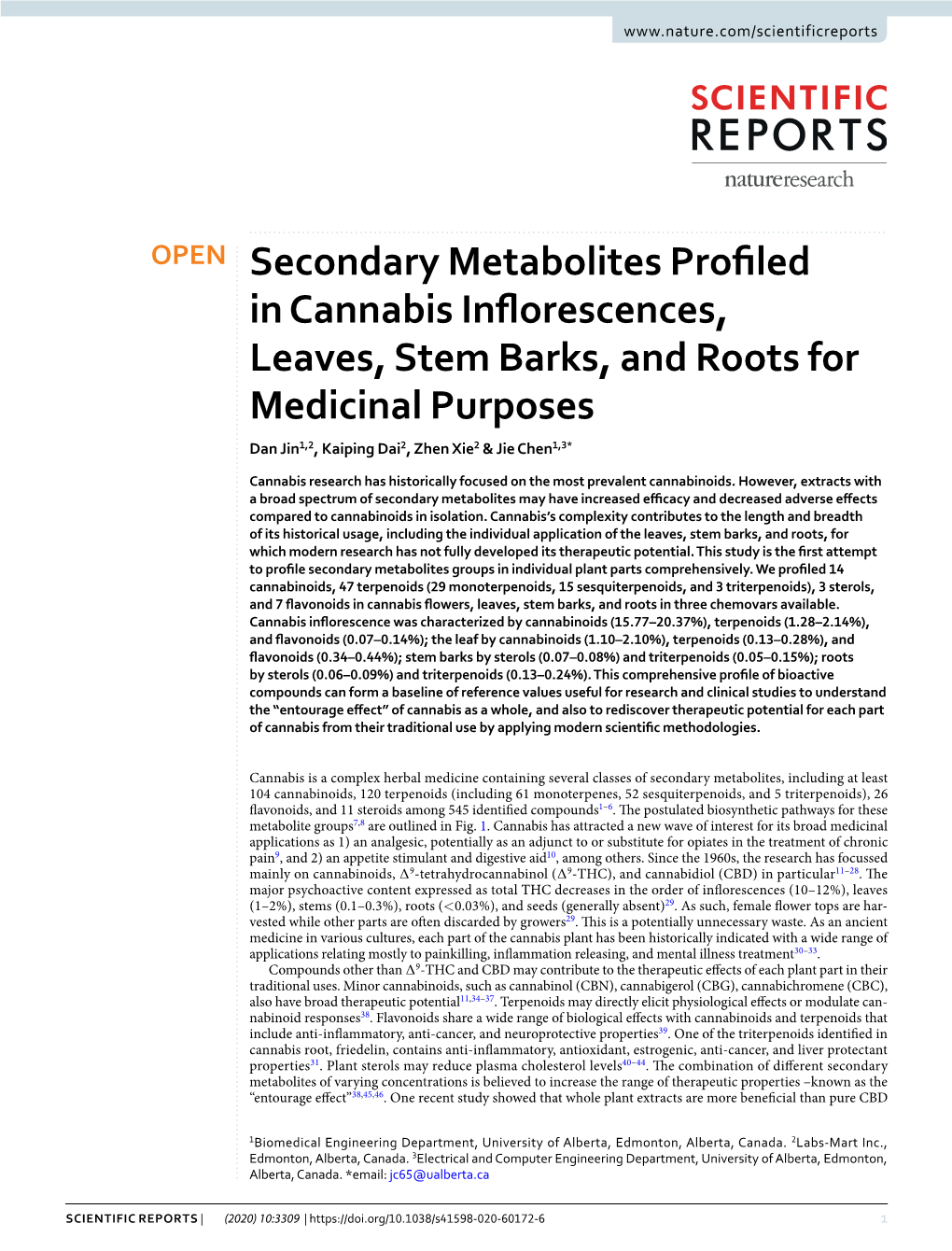
Load more
Recommended publications
-

Review Article Small Molecules from Nature Targeting G-Protein Coupled Cannabinoid Receptors: Potential Leads for Drug Discovery and Development
Hindawi Publishing Corporation Evidence-Based Complementary and Alternative Medicine Volume 2015, Article ID 238482, 26 pages http://dx.doi.org/10.1155/2015/238482 Review Article Small Molecules from Nature Targeting G-Protein Coupled Cannabinoid Receptors: Potential Leads for Drug Discovery and Development Charu Sharma,1 Bassem Sadek,2 Sameer N. Goyal,3 Satyesh Sinha,4 Mohammad Amjad Kamal,5,6 and Shreesh Ojha2 1 Department of Internal Medicine, College of Medicine and Health Sciences, United Arab Emirates University, P.O. Box 17666, Al Ain, Abu Dhabi, UAE 2Department of Pharmacology and Therapeutics, College of Medicine and Health Sciences, United Arab Emirates University, P.O. Box 17666, Al Ain, Abu Dhabi, UAE 3DepartmentofPharmacology,R.C.PatelInstituteofPharmaceuticalEducation&Research,Shirpur,Mahrastra425405,India 4Department of Internal Medicine, College of Medicine, Charles R. Drew University of Medicine and Science, Los Angeles, CA 90059, USA 5King Fahd Medical Research Center, King Abdulaziz University, Jeddah, Saudi Arabia 6Enzymoics, 7 Peterlee Place, Hebersham, NSW 2770, Australia Correspondence should be addressed to Shreesh Ojha; [email protected] Received 24 April 2015; Accepted 24 August 2015 Academic Editor: Ki-Wan Oh Copyright © 2015 Charu Sharma et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The cannabinoid molecules are derived from Cannabis sativa plant which acts on the cannabinoid receptors types 1 and 2 (CB1 and CB2) which have been explored as potential therapeutic targets for drug discovery and development. Currently, there are 9 numerous cannabinoid based synthetic drugs used in clinical practice like the popular ones such as nabilone, dronabinol, and Δ - tetrahydrocannabinol mediates its action through CB1/CB2 receptors. -

Efficacy of Cannabinoids in a Pre-Clinical Drug-Screening Platform for Alzheimer’S Disease
Molecular Neurobiology https://doi.org/10.1007/s12035-019-1637-8 Efficacy of Cannabinoids in a Pre-Clinical Drug-Screening Platform for Alzheimer’s Disease David Schubert1 & Devin Kepchia1 & Zhibin Liang1 & Richard Dargusch1 & Joshua Goldberg & Pamela Maher1 Received: 30 January 2019 /Accepted: 6 May 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Finding a therapy for Alzheimer’s disease (AD) is perhaps the greatest challenge for modern medicine. The chemical scaffolds of many drugs in the clinic today are based upon natural products from plants, yet Cannabis has not been extensively examined as a source of potential AD drug candidates. Here, we determine if a number of non-psychoactive cannabinoids are neuroprotective in a novel pre-clinical AD and neurodegeneration drug-screening platform that is based upon toxicities associated with the aging brain. This drug discovery paradigm has yielded several compounds in or approaching clinical trials for AD. Eleven cannabinoids were assayed for neuroprotection in assays that recapitulate proteotoxicity, loss of trophic support, oxidative stress, energy loss, and inflammation. These compounds were also assayed for their ability to remove intraneuronal amyloid and subjected to a structure-activity relationship analysis. Pairwise combinations were assayed for their ability to synergize to produce neuropro- tective effects that were greater than additive. Nine of the 11 cannabinoids have the ability to protect cells in four distinct phenotypic neurodegeneration screening assays, including those using neurons that lack CB1 and CB2 receptors. They are able to remove intraneuronal Aβ, reduce oxidative damage, and protect from the loss of energy or trophic support. -
Designing Microorganisms for Heterologous Biosynthesis of Cannabinoids Angelaˆ Carvalho1, Esben Halkjær Hansen1, Oliver Kayser2, Simon Carlsen1,∗ and Felix Stehle2
FEMS Yeast Research, 17, 2017, fox037 doi: 10.1093/femsyr/fox037 Advance Access Publication Date: 4 June 2017 Minireview MINIREVIEW Designing microorganisms for heterologous biosynthesis of cannabinoids Angelaˆ Carvalho1, Esben Halkjær Hansen1, Oliver Kayser2, Simon Carlsen1,∗ and Felix Stehle2 1Evolva Biotech A/S, Lersø Parkalle´ 42-44, 2100, Copenhagen, Denmark and 2Laboratory of Technical Biochemistry, Department of Biochemical and Chemical Engineering, TU Dortmund University, Emil-Figge-Str. 66, 44227 Dortmund, Germany ∗Corresponding author: Evolva Biotech A/S, Lersø Parkalle´ 42-44, 2100, Copenhagen, Denmark. Tel: +45-35-200-243; E-mail: [email protected] One sentence summary: In this review, the authors explore the use of synthetic biology as an alternative approach for the synthesis of pharmaceutical cannabinoids in a heterologous host organism. Editor: John Morrissey ABSTRACT During the last decade, the use of medical Cannabis has expanded globally and legislation is getting more liberal in many countries, facilitating the research on cannabinoids. The unique interaction of cannabinoids with the human endocannabinoid system makes these compounds an interesting target to be studied as therapeutic agents for the treatment of several medical conditions. However, currently there are important limitations in the study, production and use of cannabinoids as pharmaceutical drugs. Besides the main constituent tetrahydrocannabinolic acid, the structurally related compound cannabidiol is of high interest as drug candidate. From the more than 100 known cannabinoids reported, most can only be extracted in very low amounts and their pharmacological profile has not been determined. Today, cannabinoids are isolated from the strictly regulated Cannabis plant, and the supply of compounds with sufficient quality is a major problem. -

Cannabis Sativa: the Plant of the Thousand and One Molecules
REVIEW published: 04 February 2016 doi: 10.3389/fpls.2016.00019 Cannabis sativa: The Plant of the Thousand and One Molecules Christelle M. Andre*, Jean-Francois Hausman and Gea Guerriero Environmental Research and Innovation, Luxembourg Institute of Science and Technology, Esch-sur-Alzette, Luxembourg Cannabis sativa L. is an important herbaceous species originating from Central Asia, which has been used in folk medicine and as a source of textile fiber since the dawn of times. This fast-growing plant has recently seen a resurgence of interest because of its multi-purpose applications: it is indeed a treasure trove of phytochemicals and a rich source of both cellulosic and woody fibers. Equally highly interested in this plant are the pharmaceutical and construction sectors, since its metabolites show potent bioactivities on human health and its outer and inner stem tissues can be used to make bioplastics and concrete-like material, respectively. In this review, the rich spectrum of hemp phytochemicals is discussed by putting a special emphasis on molecules of industrial interest, including cannabinoids, terpenes and phenolic Edited by: compounds, and their biosynthetic routes. Cannabinoids represent the most studied Eugenio Benvenuto, group of compounds, mainly due to their wide range of pharmaceutical effects in ENEA, Italian National Agency for New humans, including psychotropic activities. The therapeutic and commercial interests of Technologies, Energy and Sustainable Economic Development, Italy some terpenes and phenolic compounds, and in particular stilbenoids and lignans, are Reviewed by: also highlighted in view of the most recent literature data. Biotechnological avenues to Biswapriya Biswavas Misra, enhance the production and bioactivity of hemp secondary metabolites are proposed University of Florida, USA Felix Stehle, by discussing the power of plant genetic engineering and tissue culture. -

Cannabidiol and Contributions of Major Hemp Phytocompounds to the “Entourage Effect”; Possible Mecha- Nisms
Nahler G, et al., J Altern Complement Integr Med 2019, 5: 066 DOI: 10.24966/ACIM-7562/100066 HSOA Journal of Alternative, Complementary & Integrative Medicine Review Article cannabinoid found in “drug-type” cannabis (marijuana, an obso- Cannabidiol and Contributions of lete and pejorative slang term for drug-type Cannabis), Cannabidi- ol (CBD) is the main cannabinoid in hemp (“fibre-type” Cannabis). Major Hemp Phytocompounds to The term “hemp” is therefore used for those Cannabis varieties that are low in THC (<0.2% by European law), “drug-type Cannabis” for the “Entourage Effect”; Possible those that are rich in THC, and “Cannabis” as overall term. Mechanisms Cannabis cultivars are often characterised by their THC/CBD ra- tio but a variety of terpenes have also been described as characteristic, 1 2 3 Gerhard Nahler *, Trevor M Jones and Ethan B Russo additional markers among a number of other phytocompounds that 1Clinical Investigation Support GmbH, Kaiserstrasse, Austria vary considerably between chemical varieties or “chemovars” [3,4]. 2King’s College London, London, UK The term “strain” is commonly misapplied to chemovars of Can- 3International Cannabis and Cannabinoids Institute, Prague, Czech nabis in common parlance, but is properly pertinent to bacteria and Republic viruses, but not plants [5-8]. In fact, neither CBD nor THC is formed enzymatically by the plant. Both substances are the decarboxylated form of Cannabidiolic Acid (CBDA) and delta-9-Tetrahydrocannab- Abstract inolic Acid (THCA) respectively, induced in nature by slowly aging Cannabidiol (CBD) is the primary cannabinoid in “fibre-type” can- (mainly by light), or in post-harvest processing e.g., by heating. -

5-HT3 Receptor Antagonists, 212 Acetaminophen, 211, 255
Cambridge University Press 978-1-107-02371-0 - Neuropathic Pain: Causes, Management, and Understanding Edited by Cory Toth MD and Dwight E. Moulin MD Index More information Index 5-HT3 receptor antagonists, 212 challenges in translational pain for spinal cord injury pain, 150–1 research, 44–7 neuropathic pain studies, 346 acetaminophen, 211, 255 chronic compression of the dorsal use in neuropathic pain treatment, acetylsalicylic acid, 127 root ganglion, 39 225 acupuncture, 106, 210, 349 chronic constriction nerve injury See also gabapentinoids and specific acute inflammatory demyelinating model, 38 drugs. polyneuropathy (AIDP), 135 combined drug therapies, 290–1 antidepressants, 127 acyclovir, 121 contribution of Nav1.3 channel, 70 adjuvant analgesics for cancer pain, adenosine-5’-triphosphate (ATP), contribution of Nav1.7 channel, 197–200 77–9 68–9 analgesics, 121 advanced glycosylation end products contribution of Nav1.8 channel, 69 for central post-stroke pain, 172 (AGEs), 103 contribution of Nav1.9 channel, 70 for fibromyalgia, 212 ajulemic acid (CT3), 255, 257 disease-related models, 39–41 for painful diabetic sensorimotor alcohol distal symmetrical polyneuropathy, polyneuropathy, 106–13 as a coping strategy, 3 41 for spinal cord injury pain, 150 alfentanil, 151 experimental autoimmune role in neuropathic pain treatment, allodynia, 52, 123, 151 encephalomyelitis (EAE) model, 217 alpha adrenergic receptors 160–3 See also tricyclic antidepressants; drug targeting, 346 interpreting results from animal SNRIs; SSRIs and specific drugs. -

SNP in Potentially Defunct Tetrahydrocannabinolic Acid Synthase Is a Marker for Cannabigerolic Acid Dominance in Cannabis Sativa L
G C A T T A C G G C A T genes Article SNP in Potentially Defunct Tetrahydrocannabinolic Acid Synthase Is a Marker for Cannabigerolic Acid Dominance in Cannabis sativa L. Andrea R. Garfinkel * , Matthew Otten and Seth Crawford Oregon CBD, Independence, OR 97351, USA; [email protected] (M.O.); [email protected] (S.C.) * Correspondence: [email protected] Abstract: The regulation of cannabinoid synthesis in Cannabis sativa is of increasing research interest as restrictions around the globe loosen to allow the plant’s legal cultivation. Of the major cannabi- noids, the regulation of cannabigerolic acid (CBGA) production is the least understood. The purpose of this study was to elucidate the inheritance of CBGA dominance in C. sativa and describe a marker related to this chemotype. We produced two crossing populations, one between a CBGA dominant cultivar and a tetrahydrocannabinolic acid (THCA) dominant cultivar, and one between a CBGA dominant cultivar and a cannabidiolic acid (CBDA) cultivar. Chemical and genotyping analyses confirmed that CBGA dominance is inherited as a single recessive gene, potentially governed by a non-functioning allelic variant of the THCA synthase. The “null” THCAS synthase contains a single nucleotide polymorphism (SNP) that may render the synthase unable to convert CBGA to THCA leading to the accumulation of CBGA. This SNP can be reliably used as a molecular marker for CBGA dominance in the selection and breeding of C. sativa. Citation: Garfinkel, A.R.; Otten, M.; Keywords: cannabinoids; cannabinoid synthesis; CBG; hemp Crawford, S. SNP in Potentially Defunct Tetrahydrocannabinolic Acid Synthase Is a Marker for Cannabigerolic Acid Dominance in 1. -

Chapter 1 What Is the Endocannabinoid System and Why Should You Care About It?
Chapter 1 What Is The Endocannabinoid System and Why Should You Care About It? By Chris D. Meletis, N.D. To keep your mind healthy, your joints strong, your mood calm, and your digestive system comfortable, your body was given an amazing tool. That tool is called the endocannabinoid system. Researchers discovered its existence only as recently as 1988, when they were investigating how cannabinoids found in the marijuana plant (Cannabis sativa) affect the body. The interesting thing about this system is that you don’t need marijuana to activate it. It’s a perfectly natural pathway that has served humankind and other mammals for millennia. Your body makes its own cannabinoids that work through this same system. These cannabinoids that your body makes are called endocannabinoids. There are also hemp-based cannabinoids (phytocannabinoids)—such as cannabidiol (CBD)—that work through the endocannabinoid system. These phytocannabinoids can even increase levels of your natural cannabinoids. CBD, unlike marijuana, works on the endocannabinoid system without making you high because it does not contain enough tetrahydrocannabinol (THC). That’s the component of marijuana responsible for its psychoactive effects. Even though your body makes endocannabinoids, many aspects of modern life can lead to an endocannabinoid deficiency (more on this later). That’s when hemp-based CBD oil can be especially effective. Your Body’s Locks and Keys Cells throughout your body have receptors. These receptors act like locks. They need certain substances that act like keys to open or close the receptor locks. Depending on the cell’s location in the body and receptor involved, this can open or close different doors to health or disease depending upon whether the substance acting like a receptor key is beneficial or harmful and whether it locks or unlocks the receptor. -

Analysis of Natural Product Regulation of Cannabinoid Receptors in the Treatment of Human Disease☆
Analysis of natural product regulation of cannabinoid receptors in the treatment of human disease☆ S. Badal a,⁎, K.N. Smith b, R. Rajnarayanan c a Department of Basic Medical Sciences, Faculty of Medical Sciences, University of the West Indies, Mona, Jamaica b Department of Genetics, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA c Jacobs School of Medicine and Biomedical Sciences, Department of Pharmacology and Toxicology, University at Buffalo, Buffalo, NY 14228, USA article info abstract Available online 3 June 2017 The organized, tightly regulated signaling relays engaged by the cannabinoid receptors (CBs) and their ligands, G proteins and other effectors, together constitute the endocannabinoid system (ECS). This system governs many Keywords: biological functions including cell proliferation, regulation of ion transport and neuronal messaging. This review Drug dependence/addiction will firstly examine the physiology of the ECS, briefly discussing some anomalies in the relay of the ECS signaling GTPases as these are consequently linked to maladies of global concern including neurological disorders, cardiovascular Gproteins disease and cancer. While endogenous ligands are crucial for dispatching messages through the ECS, there are G protein-coupled receptor also commonalities in binding affinities with copious exogenous ligands, both natural and synthetic. Therefore, Natural products this review provides a comparative analysis of both types of exogenous ligands with emphasis on natural prod- Neurodegenerative disorders ucts given their putative safer efficacy and the role of Δ9-tetrahydrocannabinol (Δ9-THC) in uncovering the ECS. Efficacy is congruent to both types of compounds but noteworthy is the effect of a combination therapy to achieve efficacy without unideal side-effects. -
Analyte Stability Issues During Sample Preparation: Recommendations for the Best Practices
Analyte Stability Issues during Sample Preparation: Recommendations for the Best Practices Aihua Liu, Ph.D. Director, R&D Dyad Labs 1 134th Annual Meeting & Exposition | September 8 – 24, 2020 Outline Background Recommendations for the Best Practices Examples: Case I and Case II Conclusion 2 134th Annual Meeting & Exposition | September 8 – 24, 2020 Background Ensuring analyte stability under various environmental conditions is critical for creation of an accurate and precise quantitative method. Known environmental conditions causing instability can be intentionally avoided during method development. It’s very important to comprehensively understand the compound stability before developing a quantitative method. 3 134th Annual Meeting & Exposition | September 8 – 24, 2020 Recommendations for the Best Practices Assess the stability of analytes under a variety of environmental conditions. Three main environmental conditions are pH, light exposure and temperature. The assessment should use extreme conditions. Apply appropriate pH, light and temperature conditions during sample preparation to prevent instability issue. 4 134th Annual Meeting & Exposition | September 8 – 24, 2020 Recommendations for the Best Practices 5% NH4OH Different pH Levels Water 5% FA 5 134th Annual Meeting & Exposition | September 8 – 24, 2020 Recommendations for the Best Practices Different Temperatures o Ice-Water RT 60 C 6 134th Annual Meeting & Exposition | September 8 – 24, 2020 Recommendations for the Best Practices Different Light Exposures 300 Watts Light -

Minireview the Pharmacological Case for Cannabigerol
1521-0103/376/2/204–212$35.00 https://doi.org/10.1124/jpet.120.000340 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 376:204–212, February 2021 Copyright ª 2021 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. Minireview The Pharmacological Case for Cannabigerol Rahul Nachnani, Wesley M. Raup-Konsavage, and Kent E. Vrana Department of Pharmacology, Penn State College of Medicine, Hershey, Pennsylvania Received September 15, 2020; accepted November 4, 2020 ABSTRACT Downloaded from Medical cannabis and individual cannabinoids, such as D9- antibacterial activity. There is growing interest in the commercial tetrahydrocannabinol (D9-THC) and cannabidiol (CBD), are re- use of this unregulated phytocannabinoid. This review focuses ceiving growing attention in both the media and the scientific on the unique pharmacology of CBG, our current knowledge literature. The Cannabis plant, however, produces over 100 of its possible therapeutic utility, and its potential toxicolog- different cannabinoids, and cannabigerol (CBG) serves as the ical hazards. precursor molecule for the most abundant phytocannabinoids. jpet.aspetjournals.org CBG exhibits affinity and activity characteristics between SIGNIFICANCE STATEMENT D9-THC and CBD at the cannabinoid receptors but appears Cannabigerol is currently being marketed as a dietary supple- to be unique in its interactions with a-2 adrenoceptors and ment and, as with cannabidiol (CBD) before, many claims are 5-hydroxytryptamine (5-HT1A). Studies indicate that CBG may being made about its benefits. Unlike CBD, however, little have therapeutic potential in treating neurologic disorders research has been performed on this unregulated molecule, (e.g., Huntington disease, Parkinson disease, and multiple and much of what is known warrants further investigation to sclerosis) and inflammatory bowel disease, as well as having identify potential areas of therapeutic uses and hazards. -
Study of the Effects of the Cannabinoids Anandamide and Cannabidiol on the Feeding Processes of Tetrahymena Pyriformis
Study of the Effects of the Cannabinoids Anandamide and Cannabidiol on the feeding processes of Tetrahymena pyriformis Charou Jaisswar Student ID: 32171241 December 2019 Masters by Research Project Thesis Supervised by Dr Jackie Parry and Dr Karen L. Wright Declaration This thesis is entirely my own work and has not been submitted in full or in part for the award of a higher degree at any other educational institution. No sections of this thesis have been published. Word count: 23,091 1 Table of Contents Abstract 4 Glossary 5 1. Introduction 8 1.1 The human endocannabinoid system 8 1.2 Cannabinoids 8 1.2.1. Phytocannabinoids 8 1.2.2. Endogenous cannabinoids (Endocannabinoids) 9 1.3 Biosynthetic and degradation enzymes 10 1.4 Endocannabinoid receptors and cannabinoid interactions 13 1.4.1. CB1 13 1.4.2. CB2 15 1.4.3. TRPV1 15 1.4.4. Other receptors 16 1.5. Single celled protists and cannabinoids 17 1.5.1. Introduction to protists 17 1.5.2. Presence of ECS components in ciliates 18 1.5.2.1. Endocannabinoids 18 1.5.2.2. Enzymes 18 1.5.2.3. Receptors 19 1.5.3. Effect of exogenous cannabinoids on protists 19 1.5.4. Ciliate feeding process 20 1.5.4.1. Ingestion 20 1.5.4.2. Digestion 22 1.6. Rationale and aims of this study 24 2. Materials and Methods 26 2.1. Organisms and maintenance 26 2.1.1. Preparation and maintenance of prey 26 2.1.2. Preparation and maintenance of Tetrahymena pyriformis 26 2.2.