Clinical Controversies in DOAC Reversal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: a Pharmacokinetics, Pharmacodynamics, and Safety Study
Adv Ther (2020) 37:3916–3928 https://doi.org/10.1007/s12325-020-01439-2 ORIGINAL RESEARCH Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: A Pharmacokinetics, Pharmacodynamics, and Safety Study Zining Wang . Xia Zhao . Pengkang He . Shuqing Chen . Jie Jiang . Akiko Harada . Steven Brooks . Yimin Cui Received: May 25, 2020 / Published online: July 20, 2020 Ó The Author(s) 2020 ABSTRACT b.i.d., oral). After a washout period, the 12 subjects again received dabigatran etexilate Introduction: Idarucizumab is a humanized (220 mg b.i.d., oral) and idarucizumab monoclonal antibody fragment that specifically (2.5 ? 2.5 g, intravenous) 2 h after the last binds to dabigatran with high affinity and administration of dabigatran etexilate. reverses its anticoagulant effect. This study Results: The geometric mean (gMean) values of investigated the pharmacokinetics (PK) and area under the plasma concentration–time pharmacodynamics (PD) of idarucizumab in curve (AUC0–?) and maximum concentration healthy Chinese subjects at steady state of (Cmax) were 44,200 nmol h/L and 30,900 nmol/ dabigatran and explored the effect of idaru- L, respectively. An amount of 35.3 lmol of cizumab on PK and PD of dabigatran. idarucizumab, corresponding to 33.8% of the Methods: Twelve subjects received dabigatran total dose, was excreted by urine over 72 h. The etexilate treatment alone (220 mg twice daily, area under the effect (AUECabove,2–12) in the presence and absence of idarucizumab was close to zero for all coagulation parameters, diluted Zining Wang and Xia Zhao contributed equally to this work. thrombin time (dTT), ecarin clotting time (ECT), activated partial thromboplastin time Digital Features To view digital features for this article (aPTT), and thrombin time (TT), which indi- go to https://doi.org/10.6084/m9.figshare.12613334. -

Reversal of Oral Anticoagulation in Patients with Acute Intracerebral Hemorrhage Joji B
Kuramatsu et al. Critical Care (2019) 23:206 https://doi.org/10.1186/s13054-019-2492-8 REVIEW Open Access Reversal of oral anticoagulation in patients with acute intracerebral hemorrhage Joji B. Kuramatsu* , Jochen A. Sembill and Hagen B. Huttner Abstract In light of an aging population with increased cardiovascular comorbidity, the use of oral anticoagulation (OAC) is steadily expanding. A variety of pharmacological alternatives to vitamin K antagonists (VKA) have emerged over recent years (direct oral anticoagulants, DOAC, i.e., dabigatran, rivaroxaban, apixaban, and edoxaban) which show a reduced risk for the occurrence of intracerebral hemorrhage (ICH). Yet, in the event of ICH under OAC (OAC-ICH), hematoma characteristics are similarly severe and clinical outcomes likewise substantially limited in both patients with VKA- and DOAC-ICH, which is why optimal acute hemostatic treatment in all OAC-ICH needs to be guaranteed. Currently, International Guidelines for the hemostatic management of patients with OAC-ICH are updated as several relevant large-sized observational studies and recent trials have established treatment approaches for both VKA- and DOAC-ICH. While the management of VKA-ICH is mainly based on the immediate reversal of elevated levels of international normalized ratio using prothrombin complex concentrates, hemostatic management of DOAC-associated ICH is challenging requiring specific antidotes, notably idarucizumab and andexanet alfa. This review will provide an overview of the latest studies and trials on hemostatic reversal agents and timing and summarizes the effects on hemorrhage progression and clinical outcomes in patients with OAC-ICH. Keywords: Intracerebral hemorrhage, Anticoagulation reversal, Tranexamic acid, Ciraparantag, Desmopressin Introduction importantly have a greater frequency of hematoma ex- Of all stroke sub-types, intracerebral hemorrhage (ICH) pansion (HE), all of which are significant outcome pre- constitutes roughly 15% and is associated with the worst dictors determining an even poorer prognosis [11–13]. -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD August 2016 CONTENTS General Toxicology 6 Metals 30 Management 14 Pesticides 31 Drugs 16 Chemical Warfare 33 Chemical Incidents & 24 Plants 34 Pollution Chemicals 25 Animals 34 CURRENT AWARENESS PAPERS OF THE MONTH Toxicity evaluation of α-pyrrolidinovalerophenone (α-PVP): results from intoxication cases within the STRIDA project Beck O, Franzén L, Bäckberg M, Signell P, Helander A. Clin Toxicol 2016; 54: 568-75. Context An increasing number of new psychoactive substances (NPS) of different chemical classes have become available through marketing and sale over the Internet. This report from the Swedish STRIDA project presents the prevalence, laboratory results, and clinical features in a series of intoxications involving the stimulant NPS -pyrrolidinovalerophenone (-PVP), a potent dopamine re-uptake inhibitor, over a 4-year period. Study design Observational case series of consecutive patients with admitted or suspected intake of NPS presenting to hospitals in Sweden from 2012 to 2015. Patients and methods In the STRIDA project, blood and urine samples are collected from intoxicated patients with admitted or suspected intake of NPS or unknown drugs presenting to hospitals over the country. Analysis of NPS is performed by mass spectrometry multicomponent methods. Clinical data are collected when caregivers consult the Swedish Poisons Information Centre Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 (PIC), and retrieved from medical records. -

Extended-Duration Betrixaban Versus Shorter-Duration Enoxaparin for Venous Thromboembolism Prophylaxis in Critically Ill Medical
Intensive Care Med (2019) 45:477–487 https://doi.org/10.1007/s00134-019-05565-6 ORIGINAL Extended-duration betrixaban versus shorter-duration enoxaparin for venous thromboembolism prophylaxis in critically ill medical patients: an APEX trial substudy Gerald Chi1* , C. Michael Gibson2, Arzu Kalayci1, Alexander T. Cohen3, Adrian F. Hernandez4, Russell D. Hull5, Farima Kahe1, Mehrian Jafarizade1, Sadaf Sharfaei1, Yuyin Liu6, Robert A. Harrington7 and Samuel Z. Goldhaber8 © 2019 Springer-Verlag GmbH Germany, part of Springer Nature Abstract Purpose: To assess the efcacy and safety of betrixaban for venous thromboembolism (VTE) prophylaxis among criti- cally ill patients. Methods: The APEX trial randomized 7513 acutely ill hospitalized patients to betrixaban for 35–42 days or enoxa- parin for 10 4 days. Among those, 703 critically ill patients admitted to the intensive care unit were included in the analysis, and± 547 patients who had no severe renal insufciency or P-glycoprotein inhibitor use were included in the full-dose stratum. The risk of VTE, bleeding, net clinical beneft (composite of VTE and major bleeding), and mortality was compared at 35–42 days and at 77 days. Results: At 35–42 days, extended betrixaban reduced the risk of VTE (4.27% vs 7.95%, P 0.042) without causing excess major bleeding (1.14% vs 3.13%, P 0.07). Both VTE (3.32% vs 8.33%, P 0.013) and= major bleeding (0.00% vs 3.26%, P 0.003) were decreased in the full-dose= stratum. Patients who received= betrixaban had more non-major bleeding= than enoxaparin (overall population: 2.56% vs 0.28%, P 0.011; full-dose stratum: 3.32% vs 0.36%, P 0.010). -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Standard-Dose Apixaban After Very Low-Dose Thrombolysis for Acute Intermediate-High Risk Acute Pulmonary Embolism
SAFE-LYSE | STUDY PROTOCOL Standard-dose Apixaban AFtEr Very Low-dose ThromboLYSis Title: for Acute Intermediate-high Risk Acute Pulmonary Embolism Short Title: SAFE-LYSE Protocol Version: Issue Date: 28/AUG/2019 Principal Victor Tapson1,2, Aaron Weinberg1,2 Investigators: Sub Investigators: Sam Torbati1, Susan Jackman1, Niree Hindoyan1, Joseph Meza1 1Cedars-Sinai Medical Center 8700 Beverly Blvd Los Angeles, CA 90048 Affiliations: 2Cedars-Sinai Medical GrouP 200 N. Robertson Blvd. Beverly Hills, CA 90211 Victor TaPson 8730 Alden Drive, W155 Primary Contact: Los Angeles, CA 90048 (919) 971-6441 Investigator-Initiated Bristol-Myers Squibb Company (BMS) Study Funded By: Version 8.0 | Date: 28Aug2019 1 SAFE-LYSE | STUDY PROTOCOL STUDY SYNOPSIS Funding Provided by BMS/Pfizer Alliance Standard-dose Apixaban AFtEr Very Low-dose ThromboLYSis for Protocol Title Acute Intermediate-high Risk Acute Pulmonary Embolism (SAFE-LYSE) Pulmonary embolism (PE) is a major cause of mortality in the United States, with an estimated 100,000 deaths annually and uP to 30% of Patients dying within the first month of diagnosis. Recent guidelines now risk-stratify intermediate-risk PE Patients to intermediate-low and intermediate-high risk categories, but consensus on treatment for those Patients are controversial, as compared to that of high or low-risk Patients. Because of an increased risk of major, non-major, and intracranial bleeding and an uncertain effect on survival and Post-thrombotic complications, thrombolysis is not routinely recommended in the guidelines for intermediate- risk Patients. However, studies have evaluated half-dose (50 mg dose) tissue Plasminogen activator (tPA) and this aPPears to be effective for treating PE with a reduced yet still significant risk of bleeding. -

Oral Anticoagulants
4/26/2018 Disclosure • Kelsey Gander, PharmD, BCACP Direct Oral Anticoagulants: – Declares no financial relationships pertinent to this session When to Use and How to Choose – Declares off-label use of medication will not be discussed during this presentation. Kelsey Gander, PharmD, BCACP Minnesota Academy of Physician Assistants Conference May 11th, 2018 Abbreviations Objectives • DOAC= direct oral anticoagulant 1) Compare and contrast the efficacy and safety • VTE= venous thromboembolism • DVT= deep vein thrombosis of direct oral anticoagulants (DOACs) to • PE= pulmonary embolism warfarin • A-fib, AF= atrial fibrillation 2) Identify which anticoagulant would be most • ESRD= end stage renal disease appropriate for a given patient • ACC= American College of Cardiology • AHA= American Heart Association 3) Recognize when it would not be appropriate • HRS= Heart Rhythm Society to use a DOAC • BID= twice daily Appropriate Abbreviations Patient Case JJ is a 66 y/o male who was hospitalized for pulmonary • NOAC embolism and initiated on anticoagulant therapy one week – Novel Oral Anticoagulant ago. – Chief complaint: – Non-Vitamin K Oral Anticoagulant • Presents to clinic today for INR check, post-hospital discharge follow- up • TSOAC – Past medical history: • Hypertension, hyperlipidemia, osteoarthritis, erectile dysfunction, – Target Specific Oral Anticoagulant BPH, type 2 diabetes, peripheral artery disease – Home medications • DOAC • Acetaminophen 650mg po every 6 hours PRN – Direct Oral Anticoagulant • Diazepam 5mg po at bedtime PRN anxiety -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -
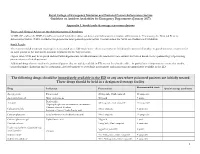
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

Laboratory Monitoring of Direct Oral Anticoagulants (Doacs)
biomedicines Review Laboratory Monitoring of Direct Oral Anticoagulants (DOACs) Claire Dunois HYPHEN BioMed, Sysmex Group, 95000 Neuville sur Oise, France; [email protected] Abstract: The introduction of direct oral anticoagulants (DOACs), such as dabigatran, rivaroxaban, apixaban, edoxaban, and betrixaban, provides safe and effective alternative to previous anticoagulant therapies. DOACs directly, selectively, and reversibly inhibit factors IIa or Xa. The coagulation effect follows the plasma concentration–time profile of the respective anticoagulant. The short half-life of a DOAC constrains the daily oral intake. Because DOACs have predictable pharmacokinetic and pharmacodynamic responses at a fixed dose, they do not require monitoring. However in specific clinical situations and for particular patient populations, testing may be helpful for patient management. The effect of DOACs on the screening coagulation assays such as prothrombin time (PT), activated partial thromboplastin time (APTT), and thrombin time (TT) is directly linked to reagent composition, and clotting time can be different from reagent to reagent, depending on the DOAC’s reagent sensitivity. Liquid chromatography–mass spectrometry (LC-MS/MS) is considered the gold standard method for DOAC measurement, but it is time consuming and requires expensive equipment. The general consensus for the assessment of a DOAC is clotting or chromogenic assays using specific standard calibrators and controls. This review provides a short summary of DOAC properties and an update on laboratory methods for measuring DOACs. Keywords: DOAC; monitoring; screening assays; quantitative assays Citation: Dunois, C. Laboratory Monitoring of Direct Oral Anticoagulants (DOACs). 1. Introduction Biomedicines 2021, 9, 445. https:// Direct oral anticoagulants (DOACs) constitute first-line therapy used for many throm- doi.org/10.3390/biomedicines9050445 boembolic indications, such as prevention and treatment of venous thromboembolism (VTE) and stroke prevention in atrial fibrillation (AF) [1,2]. -

Management of Bleeding with Non–Vitamin K Antagonist Oral Anticoagulants in the Era of Specific Reversal Agents
NEW DRUGS AND DEVICES Management of Bleeding With Non–Vitamin K Antagonist Oral Anticoagulants in the Era of Specific Reversal Agents ABSTRACT: Vitamin K antagonists are commonly used by clinicians Downloaded from to provide anticoagulation to patients who have or are at risk of having thrombotic events. In addition to familiarity with the dosing and monitoring Christian T. Ruff, MD, of vitamin K antagonists, clinicians are accustomed to using vitamin K if MPH Robert P. Giugliano, MD, there is a need to reverse the anticoagulant effect of vitamin K antagonists. SM There are now 4 new non–vitamin K antagonist oral anticoagulants (NOACs) Elliott M. Antman, MD http://circ.ahajournals.org/ that are attractive alternatives to vitamin K antagonists. Despite similar or lower rates of serious bleeding with NOACs in comparison with warfarin, there is a pressing need for strategies to manage bleeding when it does occur with NOACs and to reverse the pharmacological effect of these agents if needed. Important steps in minimizing bleeding risks with NOACs include dose adjustment of the agents in the setting of renal dysfunction and avoidance of the concomitant use of other antithrombotic agents if by MEREDITH HURT on September 28, 2016 feasible. Laboratory measurement of the anticoagulant effect of NOACs is best accomplished with specialized assays, although some of the more widely available coagulation tests can provide information that is potentially useful to clinicians. Nonspecific hemostatic agents such as prothrombin complex concentrates and recombinant factor VIIa can be used to reverse the effect of NOACs. More specific reversing agents include the approved humanized monoclonal antibody fragment idarucizumab for reversing the effects of dabigatran, the investigational factor Xa decoy andexanet alfa, and the synthetic small molecule ciraparantag. -

Transition of Anticoagulants 2019
Transition of Anticoagulants 2019 Van Hellerslia, PharmD, BCPS, CACP, Brand Generic Clinical Assistant Professor of Pharmacy Practice, Angiomax bivalirudin Temple University School of Pharmacy, Philadelphia, PA Arixtra fondaparinux Bevyxxa betrixaban Pallav Mehta, MD, Assistant Professor of Medicine, Coumadin warfarin Division of Hematology/Oncology, Eliquis apixaban MD Anderson Cancer Center at Cooper, Camden, NJ Fragmin dalteparin Lovenox enoxaparin Reviewer: Kelly Rudd, PharmD, BCPS, CACP, Pradaxa dabigatran Clinical Specialist, Anticoagulation, Bassett Medical Center, Savaysa edoxaban Cooperstown, NY Xarelto rivaroxaban From To Action Apixaban Argatroban/ Wait 12 hours after last dose of apixaban to initiate parenteral anticoagulant. In cases of Bivalirudin/ high bleeding risk, consider omitting initial bolus when transitioning to heparin infusion. Enoxaparin/ Dalteparin/ Fondaparinux/ Heparin Apixaban Warfarin When going from apixaban to warfarin, consider the use of parenteral anticoagulation as a bridge (eg, start heparin infusion or therapeutic enoxaparin AND warfarin 12 hours after last dose of apixaban and discontinue parenteral anticoagulant when INR is therapeutic). Apixaban affects INR so that initial INR measurements during the transition may not be useful for determining the appropriate dose of warfarin. Apixaban Betrixaban, Wait 12 hours from last dose of apixaban to initiate betrixaban, dabigatran, edoxaban, or Dabigatran, rivaroxaban. Edoxaban, or Rivaroxaban Argatroban Apixaban, Start apixaban, betrixaban, dabigatran,