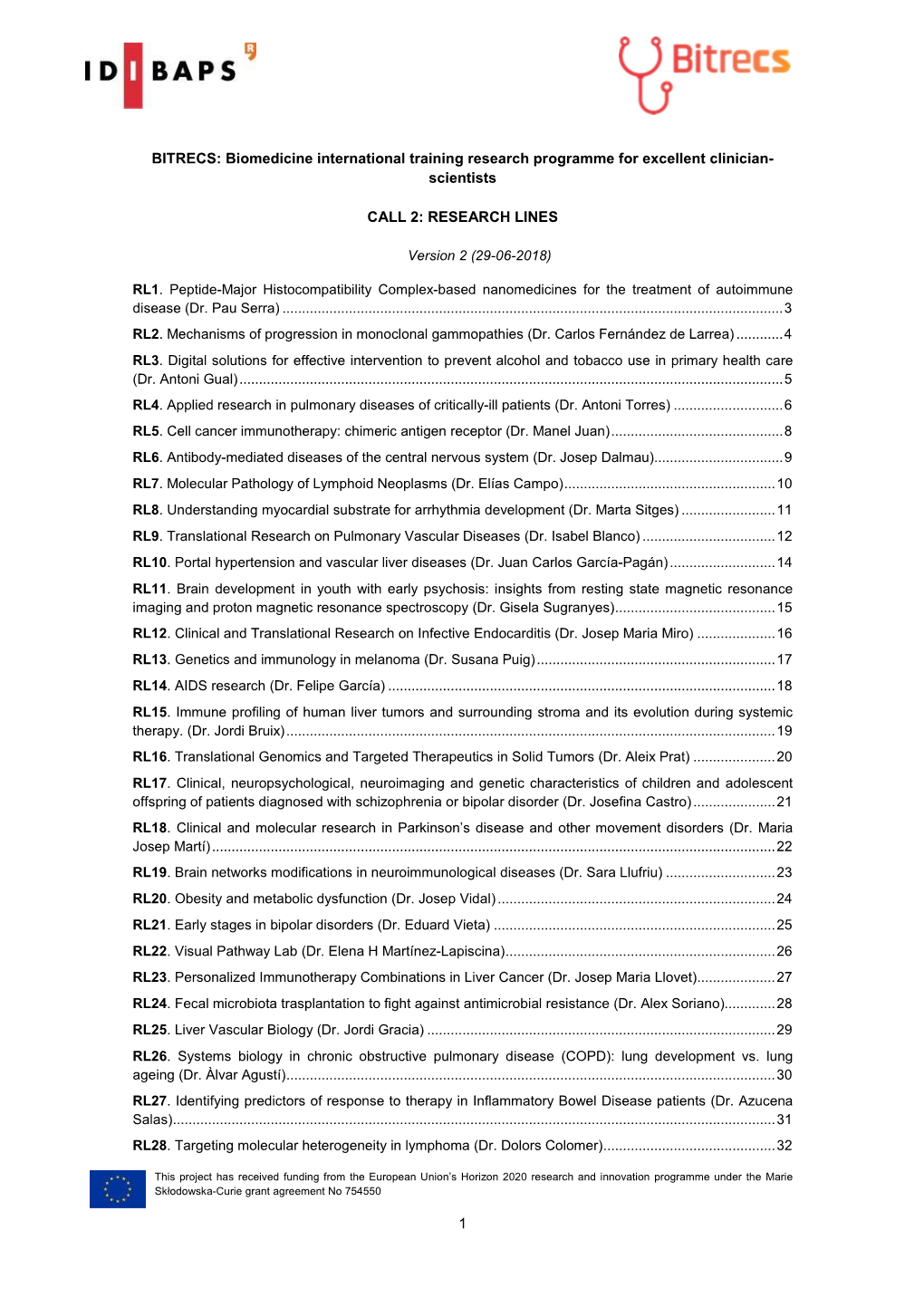
General Document Call 2 Canvi21
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Development of Virtual Screening and in Silico Biomarker Identification Model for Pharmaceutical Agents
DEVELOPMENT OF VIRTUAL SCREENING AND IN SILICO BIOMARKER IDENTIFICATION MODEL FOR PHARMACEUTICAL AGENTS ZHANG JINGXIAN NATIONAL UNIVERSITY OF SINGAPORE 2012 Development of Virtual Screening and In Silico Biomarker Identification Model for Pharmaceutical Agents ZHANG JINGXIAN (B.Sc. & M.Sc., Xiamen University) A THESIS SUBMITTED FOR THE DEGREE OF DOCTOR OF PHILOSOPHY DEPARTMENT OF PHARMACY NATIONAL UNIVERSITY OF SINGAPORE 2012 Declaration Declaration I hereby declare that this thesis is my original work and it has been written by me in its entirety. I have duly acknowledged all the sources of information which have been used in the thesis This thesis has also not been submitted for any degree in any university previously. Zhang Jingxian Acknowledgements Acknowledgements First and foremost, I would like to express my sincere and deep gratitude to my supervisor, Professor Chen Yu Zong, who gives me with the excellent guidance and invaluable advices and suggestions throughout my PhD study in National University of Singapore. Prof. Chen gives me a lot help and encouragement in my research as well as job-hunting in the final year. His inspiration, enthusiasm and commitment to science research greatly encourage me to become research scientist. I would like to appreciate him and give me best wishes to him and his loving family. I am grateful to our BIDD group members for their insight suggestions and collaborations in my research work: Dr. Liu Xianghui, Dr. Ma Xiaohua, Dr. Jia Jia, Dr. Zhu Feng, Dr. Liu Xin, Dr. Shi Zhe, Mr. Han Bucong, Ms Wei Xiaona, Mr. Guo Yangfang, Mr. Tao Lin, Mr. Zhang Chen, Ms Qin Chu and other members. -

2012 Single Cell Analysis Workshop
2012 Single Cell Analysis Workshop Where: Hyatt Regency, Bethesda MD When: April 17-18, 2012 Co-chairs: Dr. Gary Nolan (Stanford University) and Dr. Nancy Allbritton (University of North Carolina) The NIH Common Fund held a Single Cell Analysis meeting on April 17-18, 2012 in Bethesda, MD. The objective was to provide a forum to bring together a multidisciplinary group of investigators and federal staff to discuss the latest technological advances and transformative discoveries in the area of single cell analysis. The focus was on approaches that further our understanding of cell heterogeneity or variation, including identifying unique cell types and cell “states”. The goal was to share knowledge and accelerate the dissemination of technological advances within the relevant research community. The format incorporated short talks, poster presentations, and panel discussions providing the group with opportunities to review recent progress and consider the major challenges facing the field over the next decade. There were over 90 registered participants from academia as well as the public and private sectors with 20 attendees presenting posters during two day meeting. Four presentation/discussion sessions were held. A general description and summary of each follows. Session 1—Profiling Individual Cell State: Genomics Roger Lasken, Craig Venter Institute Barbara Wold, California Institute of Technology Robert Singer, Albert Einstein College of Medicine Paul Soloway, Cornell University Junhyong Kim, University of Pennsylvania Presenters discussed sequencing whole genomes at the level of a single cell or single nuclei; measuring and visualizing RNA expression and localization including technical challenges associated with multiplexed analyses; advances in single cell epigenomic analysis; and bioinformatics and computational questions using genomic/transcriptomic data from single cell experiments. -

Funding Opportunities for Research Announcements
Newsletter funding opportunities for research Announcements Alcohol, Drugs or Abuse &/or Smoking Men’s & Women’s Health Bioimaging and Radiation Research Miscellaneous Bioinformatics Musculoskeletal Biomedical Technology Nanomedicine/Nanotechnology Cancer & Blood Neurosciences Complementary & Alternative Medicine Nursing; Practice & Outcomes Research (CAM) Nutrition Cytomics Oral Cavity/Dentistry Diabetes, Endocrine & Metabolism Patient Oriented Research Digestive & Liver Pediatrics Education & Curriculum Development Pharmacy & Pharmacology Research Emergency Medicine Prizes & Awards Equipment Psychobehavioral Research/Mental Health Eyes, Ears, Nose, Throat Public Health Family Medicine Regenerative Medicine/Transplantation Genomics Skin Geriatrics/Aging Structural Biology & Proteomics Heart & Vascular Diseases Therapies & Therapeutics Immunology Training & Fellowships Infectious Disease/Biopreparedness Kidney & Urinary System NOTICES Lung and Sleep Click on a topic be taken to the page where that topic is bookmarked in the main body of the document and you can read each funding opportunity listed under that topic. Home will get you back to this page where you can select another topic. Current and archived newsletters can also be accessed on-line. Go to http://www.unmc.edu/vcr/fundingopportunities.htm 1 Volume 6, Issue 7 March 05, 2010 NOTICES Notice of Availability of Administrative Supplements for R25 Science Education Grants New NOT-DA-10-007 National Institutes of Health Blueprint for Neuroscience Research multiple institutes The National Institutes of Health Blueprint for Neuroscience Research announces an administrative supplement program of $600,000 in Fiscal Years 2010 and 2011 to provide funds to Blueprint Institute-supported research education projects (see Eligibility section below). The purpose of this program is to create and broadly disseminate materials/programs to inform students and teachers in kindergarten- 12th grade about the field of neuroscience. -

41 Nanoneuroscience and Nanoneurosurgery
Nanoneuroscience and 41 Nanoneurosurgery A Key Component of President Obama’s Brain Mapping Initiative Babak Kateb,* Vicky Yamamoto, Peter J. Basser, Michael Roy, Lucien M. Levy, Jian Tajbakhsh, Gary K. Steinberg, Allyson C. Rosen, Keith L. Black, Charlie Teo, Kuldip Sidhu, Mitchel S. Berger, and Warren S. Grundfest CONTENTS Introduction .................................................................................................................................... 547 Problem to Be Addressed ...............................................................................................................549 The National Alliance for NanoBioElectonics (NANBE) in Brain Mapping ........................... 550 National Network for Human Brain and Specimen Banks (NNHBSB) ................................... 550 National Data Repository and Analysis for Neuroscience (NDRAN) ...................................... 551 Purpose ........................................................................................................................................... 552 Significance of the Proposed Approach and Its Impact on the Field of Brain Mapping ............... 553 Programs and Methods .................................................................................................................. 553 Conclusion ..................................................................................................................................... 554 References ..................................................................................................................................... -

New Technology for the Human Cytome Project
Journal of Biological Regulators and Homeostatic Agents New technology for the human cytome project A. TÁRNOK Pediatric Cardiology, Heart Center Leipzig GmbH, University Hospital Leipzig, Leipzig, Germany ABSTRACT: Cytomes or cell systems are composed of various kinds of single-cells and constitute the elementary building units of organs and organisms. Their individualised (cytomic) analysis overcomes the problem of averaged results from cell and tissue homogenates where molecular changes in low frequency cell populations may be hidden and wrongly interpreted. Analysis of the cytome is of pivotal importance in basic research for the understanding of cells and their interrelations in complex environments like tissues and in predictive medicine where it is a prerequisite for individualised preventive therapy. Analysis of molecular phenotypes requires instrumentation that on the one hand provides high-throughput measurement of individual cells and is on the other hand highly multiplexed, enabling the simultaneous acquisition of many parameters on the single cell level. Upcoming technology suitable to this task, such as slide based cytometry is available or under development. The realisation of cytomic technology is important for the realisation of the human cytome project. (J Biol Regul Homeost Agents 2004; 18: ) KEY WORDS: Cytomics, Bioinformatics, Multilevel biocomplexity profiling, Slide based cytometry, Imaging, Human cytome project Received: Revised: Accepted: INTRODUCTION Slide based cytometry Cytomes, i.e. cell systems are composed -

Research Report 2009 Max Planck Institute for Molecular Genetics, Berlin Imprint | Research Report 2009
Research Report 2009 Max Planck Institute for Molecular Genetics, Berlin Imprint | Research Report 2009 Published by the Max Planck Institute for Molecular Genetics (MPIMG), Berlin, Germany, December 2009 Editorial Board: B.G. Herrmann, H. Lehrach, H.-H. Ropers, M. Vingron Conception & coordination: Patricia Marquardt Photography: Katrin Ullrich, MPIMG; David Ausserhofer Scientific Illustrations: MPIMG Production: Thomas Didier, Meta Data Contact: Max Planck Institute for Molecular Genetics Ihnestr. 63 – 73 14195 Berlin Germany Phone: +49 (0)30 8413-0 Fax: +49 (0)30 8413-1207 Email: [email protected] For further information about the MPIMG, please visit http://www.molgen.mpg.de MPI for Molecular Genetics Research Report 2009 Research Report 2009 1 Max Planck Institute for Molecular Genetics Berlin, December 2009 The Max Planck Institute for Molecular Genetics 2 MPI for Molecular Genetics Research Report 2009 Table of contents Organisational structure . 6 The Max Planck Institute for Molecular Genetics . 7 Mission . 7 Development of the Institute. 7 Research Concept . 8 Department of Developmental Genetics (Bernhard Herrmann) . 9 Transmission ratio distortion (H. Bauer) . 13 Regulatory Networks of Mesoderm Formation & Somitogenesis (B. Herrmann) . 17 Signal Transduction in Embryogenesis and Tumour Progression (M. Morkel) . 22 Organogenesis (H. Schrewe) . 26 General information about the whole Department . 29 Department of Vertebrate Genomics (Hans Lehrach) . 33 Molecular Embryology and Aging (J. Adjaye) . 40 Neuropsychiatric Genetics (L. Bertram) . 46 Automation (A. Dahl, W. Nietfeld, H. Seitz) . 49 Nucleic Acid-based Technologies (J. Glökler) . 55 Bioinformatics (R. Herwig) . 60 Comparative and Functional Genomics (H. Himmelbauer) . .65 Genetic Variation, Haplotypes & Genetics of Complex Diseases (M. Hoehe) . 69 3 in vitro Ligand Screening (Z. -

A Human Cytome Project
A Human Cytome Project Peter Van Osta MAIA SCIENTIFIC European Microscopy Congress Antwerp, Belgium Friday 27August 2004 A Human Cytome Project • Definitions • Introduction and rationale • Research concepts • Proposal of a strategy • Round table discussion • Conclusion A Human Cytome Project • Definitions • Introduction and rationale • Research concepts • Proposal of a strategy • Round table discussion • Conclusion Cytome - Cytomics • Cytomes can be defined as cellular systems and subsystems and functional components of the body. • Cytomics is the study of the heterogeneity of cytomes or more precisely the study of molecular single cell phenotypes resulting from genotype and exposure in combination with exhaustive bioinformatics knowledge extraction. • The word Cytomics was first used in 2001 by: Davies E, Stankovic B, Azama K, Shibata K, Abe S. “Novel components of the plant cytoskeleton: A beginning to plant "cytomics" Plant Science, Invited Review, Plant Science (160)2 (2001) pp. 185-196. A Human Cytome Project • Definitions • Introduction and rationale • Research concepts • Proposal of a strategy • Round table discussion • Conclusion Why do we need a Human Cytome Project ? Human 30,000 genes Mouse 30,000 genes 3,2000 Mb or 3.2 billion base pairs 2,500 Mb C. elegans 19,000 genes Drosophila 13,601 genes 97 Mb 165 Mb Complexity and differentiation of organisms is not only explained from the relative complexity of their genomes From Genes to Proteins to Pathways From gene to 3D protein structure Metabolic pathways The complexity of interacting metabolic pathways is not only predicted from the gene or protein structure Environment - Cell – Genome A web of interactions Environment Cell From Gene to Protein Cytome Genome - Proteome Instead of concentrating on molecular targets within the relatively infinite network of highly redundant molecular pathways of cells, one can primarily focus on the end result, represented by molecular phenotypes of cells as a consequence of both genotype and environment. -

Clinical Flow Cytometry, a Hypothesis-Driven Discipline of Modern Cytomics
Reprinted with permission of Cytometry Part A, John Wiley and Sons, Inc. © 2004 Wiley-Liss, Inc. Cytometry Part A 58A:87–97 (2004) Clinical Flow Cytometry, a Hypothesis-Driven Discipline of Modern Cytomics George Janossy* HIV Immunology, Department of Immunology and Molecular Pathology, Royal Free and University College Medical School, London, United Kingdom Recently, two major books have been published that regulatory processes, and proteomics investigates the summarize the historical aspects and recent achievements abundance of proteins simultaneously with the changes of practical flow cytometry (1,2). Both emphasize the role associated with alterations of the functional state of the played by this newly developed technical discipline in the cell. Such a “pseudo-functional” approach aims to extend development of scientific (1) and diagnostic platforms the study of quantitative changes during differentiation, during late 20th-century medicine (2). Indeed, the gray proliferation, and signaling of different cell types (5). box called a flow cytometer is the result of a multidisci- Clearly, there is an enormous, newly generated influx of plinary collaboration between engineers, biophysicists, information here, but it is not certain that a mere analysis biochemists, histopathologists, molecular cytologists, he- of genes and protein structure, even in its extended for- matologists, immunologists, and quality controllers, with a mat that includes the interaction of various biomolecules, more recent contribution from physicians specializing in will provide all of the necessary information to understand the human immunodeficiency virus (HIV), oncologists, function and regulation at the level of living cells and and epidemiologists (Table 1). organisms. Hence, the concept of cytomics has been in- The foresight by the “fathers” has been astonishing (1). -

Omics and Integrated Omics for the Promotion of Food and Nutrition Science
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Journal of Traditional and Complementary Medicine Vol. 1, No. 1, pp. 25-30 Copyright © 2011 Committee on Chinese Medicine and Pharmacy, Taiwan This is an open access article under the CC BY-NC-ND license. :ŽƵƌŶĂůŽĨdƌĂĚŝƚŝŽŶĂůĂŶĚŽŵƉůĞŵĞŶƚĂƌLJDĞĚŝĐŝŶĞ Journal homepagĞŚƩƉ͗ͬͬǁǁǁ͘ũƚĐŵ͘Žƌg Omics and Integrated Omics for the Promotion of Food and Nutrition Science Hisanori Kato*, Shoko Takahashi and Kenji Saito Food for Life, Organization for Interdisciplinary Research Projects, The University of Tokyo Abstract Transcriptomics, proteomics, and metabolomics are three major platforms of comprehensive omics analysis in the science of food and complementary medicine. Other omics disciplines, including those of epigenetics and microRNA, are matters of increasing concern. The increased use of the omics approach in food science owes much to the recent advancement of technology and bioinformatic methodologies. Moreover, many researchers now put the combination of multiple omics analysis (integrated omics) into practice to exhaustively understand the functionality of food components. However, data analysis of integrated omics requires huge amount of work and high skill of data handling. A database of nutritional omics data was constructed by the authors, which should help food scientists to analyze their own omics data more effectively. In addition, a novel tool for the easy visualization of omics data was developed by the authors’ group. The tool enables one to overview the changes of multiple omics in the KEGG pathway. Research in traditional and complementary medicine will be further facilitated by promoting the integrated omics research of food functionality. Such integrated research will only be possible with the effective collaboration of scientists with different backgrounds. -

P5 Ehealth: an Agenda for the Health Technologies of the Future
Gabriella Pravettoni Stefano Triberti Editors P5 eHealth: An Agenda for the Health Technologies of the Future P5 eHealth: An Agenda for the Health Technologies of the Future Gabriella Pravettoni • Stefano Triberti Editors P5 eHealth: An Agenda for the Health Technologies of the Future Editors Gabriella Pravettoni Stefano Triberti Department of Oncology and Department of Oncology and Hemato-Oncology Hemato-Oncology University of Milan University of Milan Milan, Italy Milan, Italy Applied Research Division for Cognitive Applied Research Division for Cognitive and Psychological Science and Psychological Science European Institute of Oncology (IEO) European Institute of Oncology (IEO) IRCCS IRCCS Milan, Italy Milan, Italy ISBN 978-3-030-27993-6 ISBN 978-3-030-27994-3 (eBook) https://doi.org/10.1007/978-3-030-27994-3 © The Editor(s) (if applicable) and The Author(s) 2020. This book is an open access publication. Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. -

Textbook of Personalized Medicine
Textbook of Personalized Medicine Textbook of Personalized Medicine Second Edition Kewal K. Jain, MD, FRACS, FFPM Jain PharmaBiotech, Basel, Switzerland Kewal K. Jain Jain PharmaBiotech Basel , Switzerland ISBN 978-1-4939-2552-0 ISBN 978-1-4939-2553-7 (eBook) DOI 10.1007/978-1-4939-2553-7 Library of Congress Control Number: 2015934582 Springer New York Heidelberg Dordrecht London © Springer Science+Business Media New York 2014, 2015 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specifi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. Printed on acid-free -

HHS Public Access Author Manuscript
HHS Public Access Author manuscript Author Manuscript Author ManuscriptJ Proteome Author Manuscript Res. Author Author Manuscript manuscript; available in PMC 2015 July 27. Published in final edited form as: J Proteome Res. 2009 June ; 8(6): 2656–2666. doi:10.1021/pr8008385. Quantitative Serum Glycomics of Esophageal Adenocarcinoma, and Other Esophageal Disease Onsets Yehia Mechref1,*, Ahmed Hussein1, Slavka Bekesova1, Vitara Pungpapong2, Min Zhang2, Lacey E. Dobrolecki3, Robert J. Hickey3, Zane T. Hammoud3, and Milos V. Novotny1,3,* 1National Center for Glycomics and Glycoproteomics, Department of Chemistry, Indiana University, 800 E. Kirkwood Ave., Bloomington, IN 47405 2Department of Statistics, Purdue University, West Lafayette, IN 47907-2068 3Department of Medicine, Indiana University School of Medicine, Indianapolis, IN 46202 Abstract Aberrant glycosylation has been implicated in various types of cancers and changes in glycosylation may be associated with signaling pathways during malignant transformation. Glycomic profiling of blood serum, in which cancer cell proteins or their fragments with altered glycosylation patterns are shed, could reveal the altered glycosylation. We performed glycomic profiling of serum from patients with no known disease (N=18), patients with high grade dysplasia (HGD, N=11) and Barrett’s (N=5), and patients with esophageal adenocarcinoma (EAC, N=50) in an attempt to delineate distinct differences in glycosylation between these groups. The relative intensities of 98 features were significantly different among the disease onsets; 26 of these correspond to known glycan structures. The changes in the relative intensities of three of the known glycan structures predicted esophageal adenocarcinoma with 94% sensitivity and better *Corresponding authors: Yehia Mechref [email protected], Milos V.