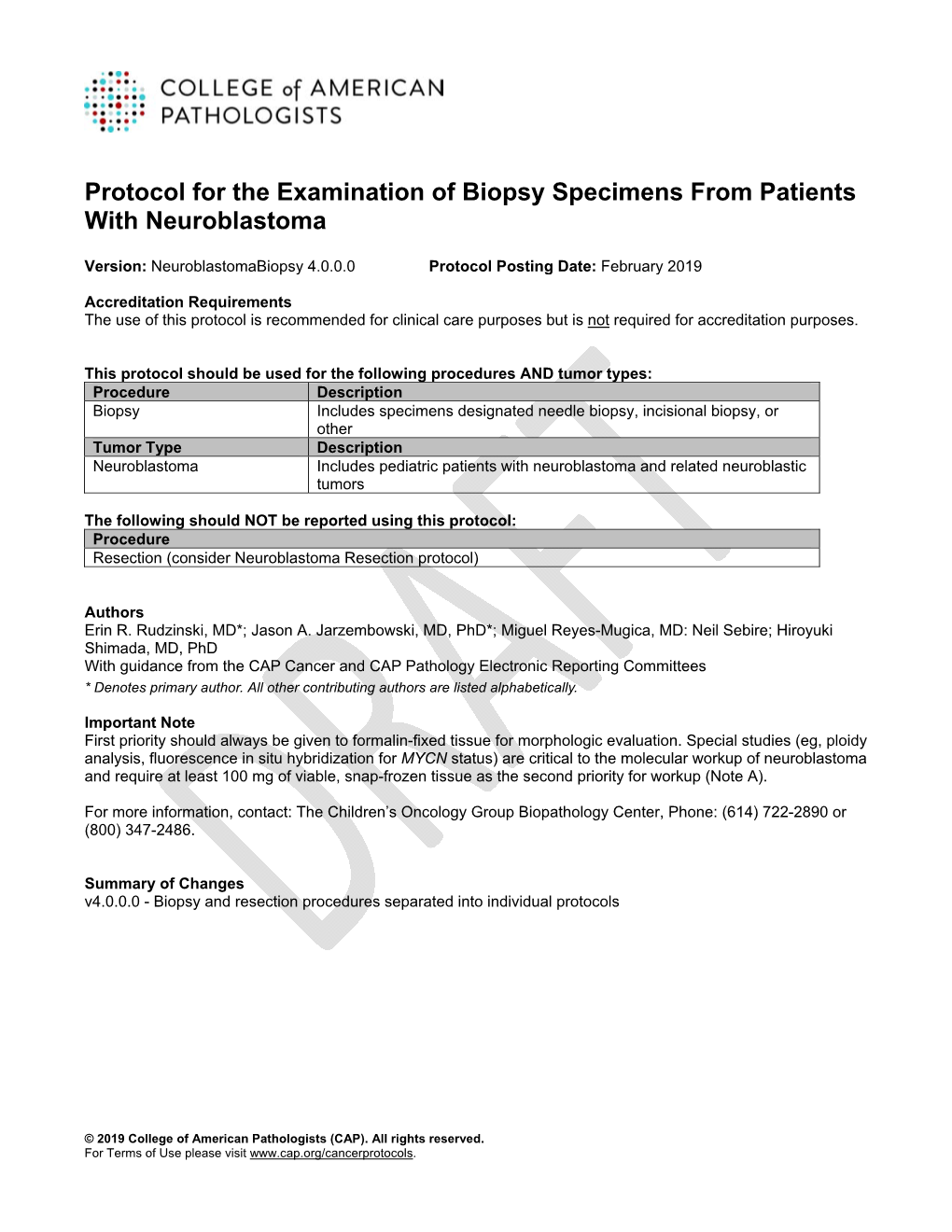
Protocol for the Examination of Biopsy Specimens from Patients with Neuroblastoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Strategy in Case with Co-Existence of Malignant Oligodendroglioma and Arteriovenous Malformation: a Case Report
Vol.2, No.8, 473-478 (2013) Case Reports in Clinical Medicine http://dx.doi.org/10.4236/crcm.2013.28125 Surgical strategy in case with co-existence of malignant oligodendroglioma and arteriovenous malformation: A case report Hirohito Yano1*, Noriyuki Nakayama1, Naoyuki Ohe1, Toshinori Takagi1, Jun Shinoda2, Toru Iwama1 1Department of Neurosurgery, Gifu University Graduate School of Medicine, Gifu, Japan; *Corresponding Author: [email protected] 2Chubu Medical Center for Prolonged Traumatic Brain Dysfunction, Department of Neurosurgery, Kizawa Memorial Hospital, Minokamo, Japan Received 26 September 2013; revised 20 October 2013; accepted 3 November 2013 Copyright © 2013 Hirohito Yano et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT with complaints of headache and vomiting. Her level of consciousness was normal and she had no neurologic A brain tumor associated with an arteriovenous deficits. Magnetic resonance images (MRI) on admission malformation (AVM) is very rare. A 42-year-old revealed a 7 cm in diameter mass lesion that showed low female presented with two separate lesions in signal intensity on the T1 weighted images (WI) and her right frontal lobe on MRI. An angiogram di- high signal intensity on the T2 WI in the right frontal agnosed one of the lesions as an AVM. The lobe. The lesion demonstrated heterogeneous enhance- second lesion appeared to be a tumor. Tumor ment by gadolinium-diethylenetriamine penta-acetic removal was difficult due to bleeding from the acid (Gd-DTPA) adjacent to the Rolandic vein (Figure nearby AVM, necessitating removal of the AVM 1(A)). -

Ganglioneuroma of the Sacrum
https://doi.org/10.14245/kjs.2017.14.3.106 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(3):106-108, 2017 www.e-kjs.org Ganglioneuroma of the Sacrum Donguk Lee1, Presacral ganglioneuromas are extremely rare benign tumors and fewer than 20 cases have been reported in the literature. Ganglioneuromas are difficult to be differentiated preoperatively Woo Jin Choe1, from tumors such as schwannomas, meningiomas, and neurofibromas with imaging modalities. 2 So Dug Lim The retroperitoneal approach for resection of presacral ganglioneuroma was performed for gross total resection of the tumor. Recurrence and malignant transformation of these tumors is rare. 1 Departments of Neurosurgery and Adjuvant chemotherapy or radiation therapy is not indicated because of their benign nature. 2Pathology, Konkuk University Medical Center, Konkuk University We report a case of a 47-year-old woman with a presacral ganglioneuroma. School of Medicine, Seoul, Korea Key Words: Ganglioneuroma, Presacral, Anterior retroperitoneal approach Corresponding Author: Woo Jin Choe Department of Neurosurgery, Konkuk University Medical Center, displacing the left sacral nerve roots, without 120-1 Neungdong-ro, Gwangjin-gu, INTRODUCTION Seoul 05030, Korea any evidence of bony invasion (Fig. 2). We performed surgery via anterior retrope- Tel: +82-2-2030-7625 Ganglioneuroma is an uncommon benign tu- ritoneal approach and meticulous adhesiolysis Fax: +82-2-2030-7359 mor of neural crest origin which is mainly loca- was necessary because of massive abdominal E-mail: [email protected] lized in the posterior mediastinum, retroperito- adhesion due to the previous gynecologic sur- 1,6) Received: August 16, 2017 neum, and adrenal gland . -

493.Full.Pdf
THE MERICAN JOURNAL OF CANCER A Continuation of The Journal of Cancer Research VOLUMEXXXVI I DECEMBER,1939 NUMBER4 GLIOMAS IN ANIMALS A REPORTOF Two ASTROCYTOMASIN THE COMMONFOWL ERWIN JUNGHERR, D.M.V., AND ABNER WOLF, M.D. (From the Department of Animal Diseases, Storrs Agricultural Experiment Station; the Department of Neuropathology, Columbia University; the Neurological Institute of New York) In one of the first modern studies of comparative tumor pathology, Bland- Sutton (4) stated that ‘‘ no tumors are peculiar to man.” While this view was supported in general by subsequent observations, the infreqhent reports of gliomas and other tumors of the central nervous system in animals other than man seemed to be significant. This low incidence, however, is probably more apparent than real. In a recent dissertation on the subject, Grun (20) points out that post-mortem examination of the brain in animals is performed com- paratively infrequently and that possible carriers of tumors of the central nerv- ous system are often disposed of by slaughter without adequate study. Enhanced interest in the study of brain tumors in man has been reflected in the increased number of reports of cerebral neoplasms in animals, espe- cially during the past decade, but many of these cases have been so inade- quately described that even an approximate classification is difficult. There is thus a definite need for wider information on the comparative pathology of tumors of the nervous system. The present communication aims to contribute to the subject by a brief critical review of the literature on gliomas in the lower animals, and by the reports of two additional cases in the common fowl. -

Case Report Synchronous Ganglioneuroma and Schwannoma Mistaken for Carotid Body Tumor
Hindawi Case Reports in Otolaryngology Volume 2017, Article ID 7973034, 2 pages https://doi.org/10.1155/2017/7973034 Case Report Synchronous Ganglioneuroma and Schwannoma Mistaken for Carotid Body Tumor Konstantinos Paraskevopoulos,1 Angeliki Cheva,2 Styliani Papaemmanuil,2 Konstantinos Vahtsevanos,1 and Konstantinos Antoniades1 1 Department of Oral and Maxillofacial Surgery, General Hospital G. Papanikolaou, 57010 Thessaloniki, Greece 2Department of Pathology, General Hospital G. Papanikolaou, 57010 Thessaloniki, Greece Correspondence should be addressed to Konstantinos Paraskevopoulos; [email protected] Received 29 May 2017; Accepted 2 August 2017; Published 24 September 2017 Academic Editor: M. Tayyar Kalcioglu Copyright © 2017 Konstantinos Paraskevopoulos et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Ganglioneuromas are a very rare benign neural tumor, commonly derived from the ganglia of the sympathetic system, and are composed of mature Schwann cells, ganglion cells, and nerve fibres. They may arise anywhere from the base of the skull to the pelvis along the paravertebral sympathetic plexus. We report a rare case of synchronous ganglioneuroma and schwannoma, mistaken for carotid body tumor. The coexistence of these two entities in head and neck region is very rare. 1. Introduction 4,4 × 2,3 × 2,7 cm between the left internal and external carotid artery. It was taken as a carotid body tumor or a para- Ganglioneuroma (GN) is a very rare entity, one per million ganglioma. Under general anesthesia, the mass was excised population [1]. It is differentiated, benign, neural tumor by oral and maxillofacial and vascular surgeons, without any that commonly derived from the ganglia of the sympa- problems during the operation. -

A Unique Combined Ganglioneuroma Schwannoma Tumor Mimicking Adrenal Malignancy
Open Access Case Report DOI: 10.7759/cureus.5500 A Unique Combined Ganglioneuroma Schwannoma Tumor Mimicking Adrenal Malignancy Katherine R. Porter 1 , Seema Shroff 2 , Tien-Anh Tran 2 , Vladimir Neychev 3 1. Miscellaneous, University of Central Florida College of Medicine, Orlando, USA 2. Pathology, AdventHealth, Orlando, USA 3. Surgery, University of Central Florida College of Medicine, Orlando, USA Corresponding author: Katherine R. Porter, [email protected] Abstract A 28-year-old woman with a past medical history significant for cervical cancer was diagnosed with a 2.5 cm adrenal tumor but was lost to follow-up. Two years later, she presented to the emergency room with worsening right upper abdominal and flank pain. The computed tomography (CT) and magnetic resonance imaging (MRI) of the abdomen and pelvis revealed that the right adrenal mass had nearly doubled in size (4.3 cm), was heterogeneous with calcifications, central necrosis and actively uptaking the intravenous (IV) contrast with a delayed washout. The biochemical workup was negative for hyperaldosteronism, hypercortisolism, and pheochromocytoma. She reported an unintentional body weight loss of 40 pounds. Adrenocortical carcinoma or a metastatic malignancy was high on the differential diagnoses list. She underwent a successful laparoscopic adrenalectomy, and final pathology revealed a benign extra-adrenal combined ganglioneurofibroma and schwannoma. These rare benign malignancies alone or in combination may closely mimic the clinical and imaging characteristics of adrenal malignancy and pose a diagnostic and therapeutic dilemma to surgeons as well as cause a significant distress to patients and their families. Thus, it is important to thoroughly document and report these cases in order to increase awareness and improve our understanding of the biology, natural history and management of these extremely rare tumors. -

Cervical Ganglioneuroma and Obstructive Hydrocephalus Following Surgery
logy & N ro eu u r e o N p h f y o s Journal of Neurology & l i a o l n o r Ionescu et al., J Neurol Neurophysiol 2017, 8:3 g u y o J Neurophysiology DOI: 10.4172/2155-9562.1000426 ISSN: 2155-9562 Case Report Open Access Cervical Ganglioneuroma and Obstructive Hydrocephalus Following Surgery - A Rare Association Ana-Maria Ionescu*, G Butoi, Sergiu Chirilă, Balan Corneliu and Hancu Anca Ovidius University of Constanta, Romania *Corresponding author: Ana-Maria Ionescu, Ovidius University of Constanta, Bvd 1 Mai 5-7, Constanta 900123, Romania, Tel: +40723381531; E-mail: [email protected] Received date: November 27, 2016; Accepted date: May 31, 2017; Published date: June 07, 2017 Copyright: © 2017 Ionescu AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Ganglioneuromas are rare tumors, known as neuroblastic or neurogenic tumors, which most often start in autonomic nerve cells, which may be found in any part of the body. We present a case of 53 years old, woman, with mild arterial hypertension, who has right sided hemiparesis, more on the leg, with gradual onset. Cerebral MRI was normal. After a few months, she developed motor deficit on the opposite leg, with the picture of triparesis and impairment of walking. MRI of the cervical spine was showing an extra medullary intradural mass C5-C6-C7 and she finally underwent extended cervical laminectomy from C-5 to C-7 level, and total ablation of the tumor. -

Tumor Heterogeneity in Glioblastomas: from Light Microscopy to Molecular Pathology
cancers Review Tumor Heterogeneity in Glioblastomas: From Light Microscopy to Molecular Pathology Aline P. Becker 1,* , Blake E. Sells 2 , S. Jaharul Haque 1 and Arnab Chakravarti 1 1 Comprehensive Cancer Center, Ohio State University, Columbus, OH 43210, USA; [email protected] (S.J.H.); [email protected] (A.C.) 2 Medical Scientist Training Program, Washington University in St. Louis, St. Louis, MO 63310, USA; [email protected] * Correspondence: [email protected] Simple Summary: Glioblastomas (GBMs) are the most frequent and aggressive malignant tumors arising in the human brain. One of the main reasons for GBM aggressiveness is its diverse cellular composition, comprised by differentiated tumor cells, tumor stem cells, cells from the blood vessels, and inflammatory cells, which simultaneously affect multiple cellular functions involved in cancer development. “Tumor Heterogeneity” usually encompasses both inter-tumor heterogeneity, differ- ences observed at population level; and intra-tumor heterogeneity, differences among cells within individual tumors, which directly affect outcomes and response to treatment. In this review, we briefly describe the evolution of GBM classification yielded from inter-tumor heterogeneity studies and discuss how the technological development allows for the characterization of intra-tumor hetero- geneity, beginning with differences based on histopathological features of GBM until the molecular alterations in DNA, RNA, and proteins observed at individual cells. Citation: Becker, A.P.; Sells, B.E.; Abstract: One of the main reasons for the aggressive behavior of glioblastoma (GBM) is its intrinsic Haque, S.J.; Chakravarti, A. Tumor intra-tumor heterogeneity, characterized by the presence of clonal and subclonal differentiated tumor Heterogeneity in Glioblastomas: cell populations, glioma stem cells, and components of the tumor microenvironment, which affect From Light Microscopy to Molecular multiple hallmark cellular functions in cancer. -

Mental and Seizure Manifestations in Relation to Brain Tumors a Statistical Study
166 EPlLEPSlA Mental and Seizure Manifestations in Relation to Brain Tumors A Statistical Study A. GUVENER, B. K. BAGCHI, K. A. KO01 AND H. D. CALHOUN The Electroencephalographic Laboratory, Neuropsychiatric Institute, University of Michigan Medical Center, Ann Arbor, Mich. (U.S.A.) INTRODUCTION It is well known that mental or behavioral changes and seizures occur in some phases of the development of many tumors. Many investigators in reporting large series (300 or over) have given the frequency of the clinical manifestations and their relation- ships to areas and types of tumors (2, 4, 5, 9, 10, 12-15, 17, 20, 22, 24, 27, 31). It is not always clear why some tumors produce the above mentioned manifestations and others of Lhe same type, same location and about the same size do not. We thought it might be of interest to make a statistical evaluation of the interrelationships between three variables, tumor location, tumor type, increased intracranial pressure in respect to mental and seizure manifestations. In the literature these relationships are not always clearly given. These might have some bearing on the mechanism of the clinical changes. MATERIAL AND METHODS Out of 901 brain tumor entries in the EEG Laboratory file with EEG and clinical data only 326 have been selected for this report. The excluded ones are the following: all 359 brain tumor entries before 1950, in addition to a total of 167 metastatic, brain stem and posterior fossa tumors, and 49 tumors with incomplete clinical and EEG information. Out of the accepted 326 cases gross and microscopic autopsy findings were available in 62. -

Cervical Dumbbell Ganglioneuroma Producing Spinal Cord Compression
Letter to Editor References A B 1. Bed TR, Kaur S, Kumar B. Red grain mycetoma of the scalp (Actinomadura pelletieri). A case report from India. Mycopathologia 1978;63:127-8. 2. Venugopal PV, Venugopal TV. Red grain mycetoma of the scalp due to Actinomadura pelletieri in Madurai. Indian J Pathol Microbiol 1990;33:384-6. 3. Mathur DR, Bharadwaj V, Vaishnav K, Ramdeo IN. Red grain mycetoma caused Actinomadura pelletieri in western Rajasthan. Report of two cases. Indian J Pathol Microbiol 1993;36:486-8 4. Fahal AH, el-Toum EA, el-Hassan AM, Mahgoub-ES, Gumma SA. A prelimi- nary study on the ultrastructure of Actinomadura pelletieri and its host tissue reaction. J Med Vet Mycol 1994;32:343-8. 5. Ndiaye B, Develoux M, Langlade MA, Kane A. Actinomycotic mycetoma. Aprospos of 27 cases in Dakar: medical treatment with cotrimoxazole. Ann Figure 2: Postoperative MRI of cervical spine: A. Transverse image Dermatol Venereol 1994;121:161-5. after intraspinal operation shows no tumour in spinal canal with remaining paraspinal mass; B.transverse image after extraspinal approache reveals complete tumor removal Accepted on 10-04-2005 Cervical dumbbell ganglioneuroma producing spinal cord compression Sir, A 39-year old man presented with complains of progressive weakness and numbness of all four limbs for six months. There was moderate spastic tetraparesis that was more marked on Figure 3: The pathologic finding of tumor tissue shows mature ganglion cells inside characteristic wave and loose stroma the left side, and hypoesthesia below the C5 dermatome. (HE, original magnification x 100). Magnetic resonance imaging (MRI) showed a large ex- tramedullary dumbbell mass at the C4-C5 level. -

Pediatric Spine and Spinal Cord Tumors: a Neglected Area?
Pediatric Spine and Spinal Cord Tumors: Disclosure A Neglected Area? • I have nothing to disclose • No relevant financial relations interfering with ECPNR 2020 my presentation Rome • Several cases shared by Thierry Huisman, MD and Aylin Tekes, MD Bruno P Soares, MD Associate Professor of Radiology Division Chief of Neuroradiology University of Vermont Medical Center Burlington, VT Outline Epidemiology • Epidemiology • Pediatric spinal cord neoplasms • Clinical presentation • 4-10% primary CNS tumors • Compartmental approach to diagnosis • 25% of all spinal tumors • Most prevalent between 1 and 5 years • Imaging findings • Differential diagnosis Epidemiology Approach to Diagnosis: Location • Intramedullary • Intramedullary Tumors • Glial: Astrocytoma, Ependymoma • Astrocytoma (pilocytic > diffuse): 60% • Neuroglial or Non-glial: Ganglioglioma, Hemangioblastoma • Ependymoma (assoc. with NF2): 15-30% • Intradural extramedullary • Ganglioglioma: up to 15% • Nerve sheath tumors • Meningioma • Paraganglioma • Mixopapillary ependymoma • Embryonal tumors •ATRT • Leptomeningeal metastasis Nonspecific Clinical Symptoms Clinical Presentation • Progressive motor weakness • Progressive scoliosis • Gait disturbance / falls • Paraspinal muscle spasmp • 25-30% presentp withh back pain!p • Up to 15% present with raised ICP Incorrect radiological work-up: Delay between onset of clinical symptoms and diagnosis Clinical Presentation: Back Pain MRI of Spinal Cord Tumors 1.. Cord expansion is a • Spinal pain (70%) major feature of T2-FSE • Dull and aching pain, localized to bone segments intramedullary adjacent to tumor neoplasms • Distension of thecal sac by enlarged cord • Root pain • Nerve root compression If absent or minimal, • Tract pain consider non-neoplastic • Vague, burning pain with paresthesias etiologies: MS, ADEM, • Infiltration of spinothalamic tracts sarcoidosis, ischemia... Astrocytoma ADEM Epstein F, Epstein N. Pediatric neurosurgery 1982: 529-540 MRI of Spinal Cord Tumors MRI of Spinal Cord Tumors 2. -

Cervical Spine Ganglioneuroma: a Case Report
Global Journal of Otolaryngology ISSN 2474-7556 Case Report Glob J Otolaryngol Volume 12 Issue 3 - December 2017 Copyright © All rights are reserved by Mehdi Chiniforoush DOI: 10.19080/GJO.2017.12.555837 Cervical Spine Ganglioneuroma: A Case Report Misagh Pourdonya1, Zhila Kazemi1 and Mehdi Chiniforoush2* 1Medical Student, Ardabil University of Medical Sciences, Iran 2Pathology Assistant Professor, Anatomical Sciences Department, Ardabil University of Medical Sciences, Iran Submission: December 13, 2017; Published: December 19, 2017 *Corresponding author: Mehdi Chiniforoush, Pathology Assistant Professor, Anatomical Sciences Department, Ardabil University of Medical Sciences, Iran, Tel: ; Email: Abstract Spinal and paraspinal tumors comprise a wide variety of histological types. About 1% of this neoplasm’s are Ganglioneuroma and a small proportion of them may invaginate through the intervertebral foramina causing cord compression. The recent case is about a 23 year old male referring to Fatemi Hospital of Ardabil University of medical sciences with the right extremities hemiparesis and after primary clinical examinations, taking MRI and CT scan; cervico-occipital tumor was diagnosed. Then, the patient was hospitalized at males’ neurosurgery ward. He was operated at the same hospital; the tumor was evacuated completely and for exact survey and further studies were sent to pathology. In macroscopic view, smooth tissue containing paramorphic irregular gray components diagnosed Ganglioneuroma at histopathology study/ microscopic view was observed. Keywords: Ganglioneuroma; Cervical Spine; Ardabil Introduction cases, intra-tumoral areas of malignant transformation, metastasis, Ganglioneuromas are rare, slow growing; benign tumors and the development of malignant peripheral tumors arising that generally arise from the ganglion cells of the sympathetic from ganglioneuromas have been described [6-10]. -

Care of Adults with Neurofibromatosis Type 1: a Clinical Practice Resource of the American College of Medical Genetics and Genomics (ACMG)
© American College of Medical Genetics and Genomics ACMG PRACTICE GUIDELINE Care of adults with neurofibromatosis type 1: a clinical practice resource of the American College of Medical Genetics and Genomics (ACMG) Douglas R. Stewart, MD1, Bruce R. Korf, MD, Ph.D2, Katherine L. Nathanson, MD3,4, David A. Stevenson, MD5 and Kaleb Yohay, MD6 Disclaimer: This practice resource is designed primarily as an educational resource for medical geneticists and other clinicians to help them provide quality medical services. Adherence to this practice resource is completely voluntary and does not necessarily assure a successful medical outcome. This practice resource should not be considered inclusive of all proper procedures and tests or exclusive of other procedures and tests that are reasonably directed to obtaining the same results. In determining the propriety of any specific procedure or test, the clinician should apply his or her own professional judgment to the specific clinical circumstances presented by the individual patient or specimen. Clinicians are encouraged to document the reasons for the use of a particular procedure or test, whether or not it is in conformance with this practice resource. Clinicians also are advised to take notice of the date this practice resource was adopted, and to consider other medical and scientific information that becomes available after that date. It also would be prudent to consider whether intellectual property interests may restrict the performance of certain tests and other procedures. Purpose: Neurofibromatosis type 1 (NF1) is an autosomal Results: Malignant peripheral nerve sheath tumor (MPNST), breast dominant disorder that is caused by a heterozygous loss-of- cancer, cutaneous neurofibromas, and significant psychiatric and function variant in the tumor suppressor gene NF1; it affects neurologic diagnoses are common problems in patients with NF1.