Documentation Dissection
Total Page:16
File Type:pdf, Size:1020Kb
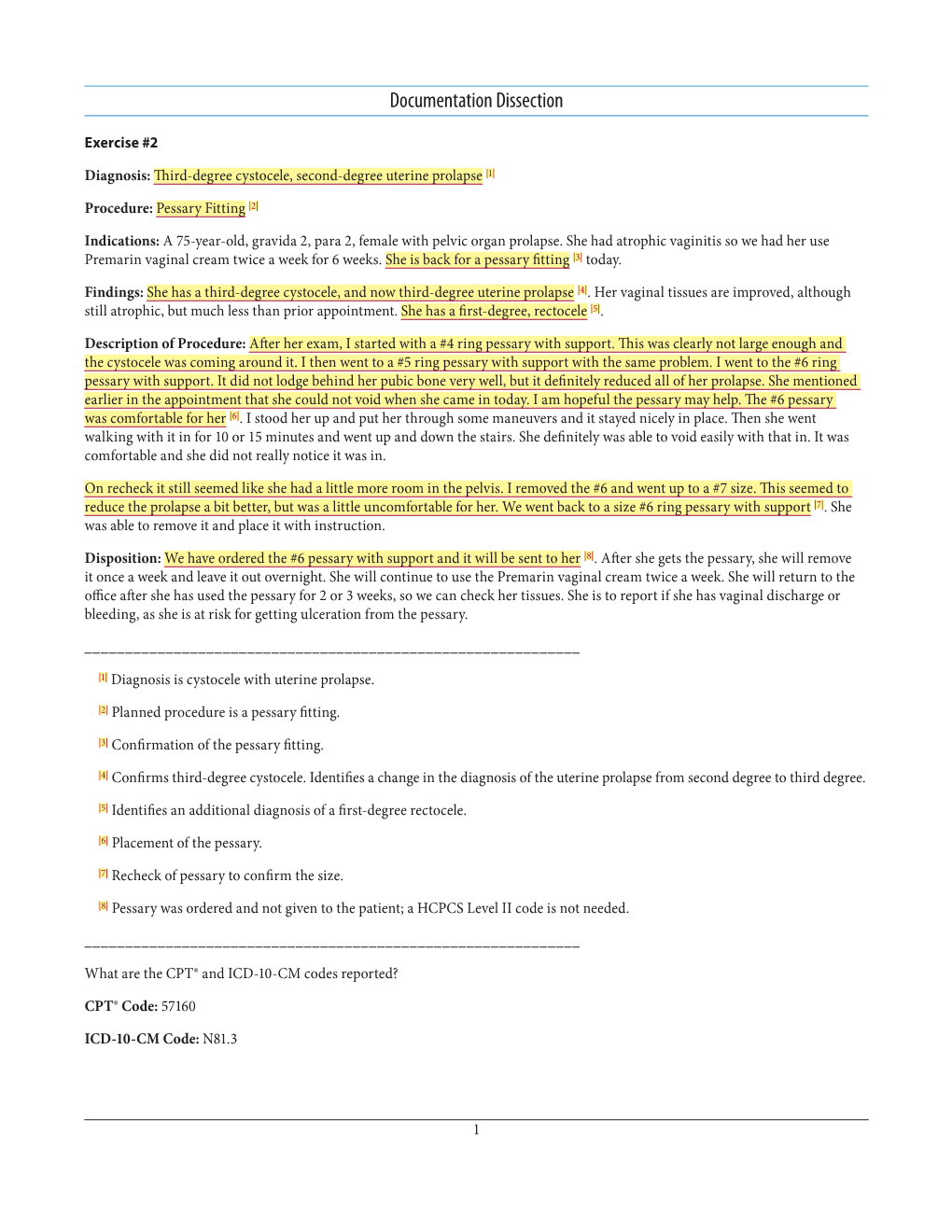
Load more
Recommended publications
-

What Is a Hysterectomy?
Greenwich Hospital What is a Hysterectomy? PATIENT/FAMILY INFORMATION SHEET What is a Hysterectomy? A hysterectomy is the surgical removal of the uterus (womb). Sometimes the fallopian tubes, ovaries, and cervix are removed at the same time that the uterus is removed. When the ovaries and both tubes are removed, this is called a bilateral salpingo- oophorectomy. There are three types of hysterectomies: • A complete or total hysterectomy, which is removal of the uterus and cervix. • A partial or subtotal hysterectomy, which is removal of the upper portion of the uterus, leaving the cervix in place. • A radical hysterectomy, which is removal of the uterus, cervix, the upper part of the vagina, and supporting tissue. If you have not reached menopause yet, a hysterectomy will stop your monthly periods. You also will not be able to get pregnant. How is a hysterectomy performed? A hysterectomy can be performed in three ways: • Abdominal hysterectomy: The surgeon will make a cut, or incision, in your abdomen either vertically (up and down) in the middle of the abdomen below the umbilicus (belly button); or horizontally (side ways) in the pelvic area. The horizontal incision is sometimes referred to as a “bikini” incision and is usually hidden by undergarments. • Vaginal hysterectomy: The surgeon goes through the vagina and the incision is on the inside of the vagina, not on the outside of the body. • Laparoscopically assisted vaginal hysterectomy: This involves using a small, telescope-like device called a laparoscope, which is inserted into the abdomen through a small cut. This brings light into the abdomen so that the surgeon can see inside. -

Perceived Gynecological Morbidity Among Young Ever-Married Women
Perceived Gynecological Morbidity among Young ever-married Women living in squatter settlements of Karachi, Pakistan Pages with reference to book, From 92 To 97 Fatima Sajan,Fariyal F. Fikree ( Department of Community Health Sciences, The Aga Khan University, Karachi, Pakistan. ) Abstract Background: Community-based information on obstetric and gynecological morbidity in developing countries is meager and nearly non-existent in Pakistan. Objectives: To estimate the prevalence of specific gynecological morbidities and investigate the predictors of pelvic inflammatory disease Methods: Users and non-users of modem contraceptives were identified from eight squatter settlements of Karachi, Pakistan and detailed information on basic demographics, contraceptive use, female mobility, decision-making and gynecological morbidities were elicited. Results: The perceived prevalence of menstrual disorders were 45.3%, uterine prolapse 19.1%, pelvic inflammatory disease 12.8% and urinary tract infection 5.4%. The magnitude of gynecological morbidity was high with about 55% of women reporting at least one gynecological morbidity though fewer reported at least two gynecological morbidities. Significant predictors of pelvic inflammatory disease were intrauterine contraceptive device users (OR = 3.1; 95% CI 1.7- 5.6), age <20 years (OR = 2.3; 95% CI 1.1 - 4.8) and urban life style (OR = 2.1; 95% CI 1.0-4.6). Conclusion: There is an immense burden of reproductive ill-health and a significant association between eyer users of intrauterine contraceptive device and pelvic inflammatory disease. We therefore suggest improvement in the quality of reproductive health services generally, but specifically for family planning services (JPMA 49:92, 1999). Introduction Gynecological morbidity has been defined as structural and functional disorders of the genital tract which are not directly related to pregnancy, delivery and puerperium. -

Vaginitis and Abnormal Vaginal Bleeding
UCSF Family Medicine Board Review 2013 Vaginitis and Abnormal • There are no relevant financial relationships with any commercial Vaginal Bleeding interests to disclose Michael Policar, MD, MPH Professor of Ob, Gyn, and Repro Sciences UCSF School of Medicine [email protected] Vulvovaginal Symptoms: CDC 2010: Trichomoniasis Differential Diagnosis Screening and Testing Category Condition • Screening indications – Infections Vaginal trichomoniasis (VT) HIV positive women: annually – Bacterial vaginosis (BV) Consider if “at risk”: new/multiple sex partners, history of STI, inconsistent condom use, sex work, IDU Vulvovaginal candidiasis (VVC) • Newer assays Skin Conditions Fungal vulvitis (candida, tinea) – Rapid antigen test: sensitivity, specificity vs. wet mount Contact dermatitis (irritant, allergic) – Aptima TMA T. vaginalis Analyte Specific Reagent (ASR) Vulvar dermatoses (LS, LP, LSC) • Other testing situations – Vulvar intraepithelial neoplasia (VIN) Suspect trich but NaCl slide neg culture or newer assays – Psychogenic Physiologic, psychogenic Pap with trich confirm if low risk • Consider retesting 3 months after treatment Trichomoniasis: Laboratory Tests CDC 2010: Vaginal Trichomoniasis Treatment Test Sensitivity Specificity Cost Comment Aptima TMA +4 (98%) +3 (98%) $$$ NAAT (like GC/Ct) • Recommended regimen Culture +3 (83%) +4 (100%) $$$ Not in most labs – Metronidazole 2 grams PO single dose Point of care – Tinidazole 2 grams PO single dose •Affirm VP III +3 +4 $$$ DNA probe • Alternative regimen (preferred for HIV infected -

Uterine Prolapse
Uterine prolapse Definition Uterine prolapse is falling or sliding of the uterus from its normal position in the pelvic cavity into the vaginal canal. Alternative Names Pelvic relaxation; Pelvic floor hernia Causes The uterus is normally supported by pelvic connective tissue and the pubococcygeus muscle, and held in position by special ligaments. Weakening of these tissues allows the uterus to descend into the vaginal canal. Tissue trauma sustained during childbirth, especially with large babies or difficult labor and delivery, is typically the cause of muscle weakness. The loss of muscle tone and the relaxation of muscles, which are both associated with normal aging and a reduction in the female hormone estrogen, are also thought to play an important role in the development of uterine prolapse. Descent can also be caused by a pelvic tumor, however, this is fairly rare. Uterine prolapse occurs most commonly in women who have had one or more vaginal births, and in Caucasian women. Other conditions associated with an increased risk of developing problems with the supportive tissues of the uterus include obesity and chronic coughing or straining. Obesity places additional strain on the supportive muscles of the pelvis, as does excessive coughing caused by lung conditions such as chronic bronchitis and asthma. Chronic constipation and the pushing associated with it causes weakness in these muscles. Symptoms z Sensation of heaviness or pulling in the pelvis z A feeling as if "sitting on a small ball" z Low backache z Protrusion from the vaginal opening (in moderate to severe cases) z Difficult or painful sexual intercourse Exams and Tests A pelvic examination (with the woman bearing down) reveals protrusion of the cervix into the lower part of the vagina (mild prolapse), past the vaginal introitus/opening (moderate prolapse), or protrusion of the entire uterus past the vaginal introitus/opening (severe prolapse). -

Uterine Prolapse Treatment Without Hysterectomy
Uterine Prolapse Treatment Without Hysterectomy Authored by Amy Rosenman, MD Can The Uterine Prolapse Be Treated Without Hysterectomy? A Resounding YES! Many gynecologists feel the best way to treat a falling uterus is to remove it, with a surgery called a hysterectomy, and then attach the apex of the vagina to healthy portions of the ligaments up inside the body. Other gynecologists, on the other hand, feel that hysterectomy is a major operation and should only be done if there is a condition of the uterus that requires it. Along those lines, there has been some debate among gynecologists regarding the need for hysterectomy to treat uterine prolapse. Some gynecologists have expressed the opinion that proper repair of the ligaments is all that is needed to correct uterine prolapse, and that the lengthier, more involved and riskier hysterectomy is not medically necessary. To that end, an operation has been recently developed that uses the laparoscope to repair those supporting ligaments and preserve the uterus. The ligaments, called the uterosacral ligaments, are most often damaged in the middle, while the lower and upper portions are usually intact. With this laparoscopic procedure, the surgeon attaches the intact lower portion of the ligaments to the strong upper portion of the ligaments with strong, permanent sutures. This accomplishes the repair without removing the uterus. This procedure requires just a short hospital stay and quick recovery. A recent study from Australia found this operation, that they named laparoscopic suture hysteropexy, has excellent results. Our practice began performing this new procedure in 2000, and our results have, likewise, been very good. -

Pessary Information
est Ridge obstetrics & gynecology, LLP 3101 West Ridge Road, Rochester, NY 14626 1682 Empire Boulevard, Webster, NY 14580 www.wrog.org Tel. (585) 225‐1580 Fax (585) 225‐2040 Tel. (585) 671‐6790 Fax (585) 671‐1931 USE OF THE PESSARY The pessary is one of the oldest medical devices available. Pessaries remain a useful device for the nonsurgical treatment of a number of gynecologic conditions including pelvic prolapse and stress urinary incontinence. Pelvic Support Defects The pelvic organs including the bladder, uterus, and rectum are held in place by several layers of muscles and strong tissues. Weaknesses in this tissue can lead to pelvic support defects, or prolapse. Multiple vaginal deliveries can weaken the tissues of the pelvic floor. Weakness of the pelvic floor is also more likely in women who have had a hysterectomy or other pelvic surgery, or in women who have conditions that involve repetitive bearing down, such as chronic constipation, chronic coughing or repetitive heavy lifting. Although surgical repair of certain pelvic support defects offers a more permanent solution, some patients may elect to use a pessary as a very reasonable treatment option. Classification of Uterine Prolapse: Uterine prolapse is classified by degree. In first‐degree uterine prolapse, the cervix drops to just above the opening of the vagina. In third‐degree prolapse, or procidentia, the entire uterus is outside of the vaginal opening. Uterine prolapse can be associated with incontinence. Types of Vaginal Prolapse: . Cystocele ‐ refers to the bladder falling down . Rectocele ‐ refers to the rectum falling down . Enterocele ‐ refers to the small intestines falling down . -
Gynecological-DBQ
INTERNAL VETERANS AFFAIRS USE GYNECOLOGICAL CONDITIONS DISABILITY BENEFITS QUESTIONNAIRE IMPORTANT - THE DEPARTMENT OF VETERANS AFFAIRS (VA) WILL NOT PAY OR REIMBURSE ANY EXPENSES OR COST INCURRED IN THE PROCESS OF COMPLETING AND/OR SUBMITTING THIS FORM. PLEASE READ THE PRIVACY ACT AND RESPONDENT BURDEN INFORMATION ON REVERSE BEFORE COMPLETING FORM. NAME OF PATIENT/VETERAN PATIENT/VETERAN'S SOCIAL SECURITY NUMBER NOTE TO PHYSICIAN - Your patient is applying to the U.S. Department of Veterans Affairs (VA) for disability benefits. VA will consider the information you provide on this questionnaire as part of their evaluation in processing the claim. VA reserves the right to confirm the authenticity of ALL DBQs completed by private health care providers. IS THIS DBQ BEING COMPLETED IN CONJUNCTION WITH A VA21-2507, C&P EXAMINATION REQUEST? YES NO If no, how was the examination completed (check all that apply)? In-person examination Records reviewed Other, please specify: Comments: ACCEPTABLE CLINICAL EVIDENCE (ACE) INDICATE METHOD USED TO OBTAIN MEDICAL INFORMATION TO COMPLETE THIS DOCUMENT: Review of available records (without in-person or video telehealth examination) using the Acceptable Clinical Evidence (ACE) process because the existing medical evidence provided sufficient information on which to prepare the DBQ and such an examination will likely provide no additional relevant evidence. Review of available records in conjunction with a telephone interview with the Veteran (without in-person or telehealth examination) using the ACE process because the existing medical evidence supplemented with a telephone interview provided sufficient information on which to prepare the DBQ and such an examination would likely provide no additional relevant evidence. -

ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics
Diagnostic Services ICD-9-CM and ICD-10-CM Codes for Gynecology and Obstetrics ICD-9 ICD-10 ICD-9 ICD-10 Diagnoses Diagnoses Code Code Code Code Menstral Abnormalities 622.12 Moderate Dysplasia Of Cervix (CIN II) N87.2 625.3 Dysmenorrhea N94.6 Menopause 625.4 Premenstrual Syndrome N94.3 627.1 Postmenopausal Bleeding N95.0 626.0 Amenorrhea N91.2 627.2 Menopausal Symptoms N95.1 626.1 Oligomenorrhea N91.5 627.3 Senile Atrophic Vaginitis N95.2 626.2 Menorrhagia N92.0 627.4 Postsurgical Menopause N95.8 626.4 Irregular Menses N92.6 627.8 Perimenopausal Bleeding N95.8 626.6 Metrorrhagia N92.1 Abnormal Pap Smear Results 626.8 Dysfunctional Uterine Bleeding N93.8 795.00 Abnormal Pap Smear Result, Cervix R87.619 Disorders Of Genital Area 795.01 ASC-US, Cervix R87.610 614.9 Pelvic Inflammatory Disease (PID) N73.9 795.02 ASC-H, Cervix R87.611 616.1 Vaginitis, Unspecified N76.0 795.03 LGSIL, Cervix R87.612 616.2 Bartholin’s Cyst N75.0 795.04 HGSIL, Cervix R87.613 Cervical High-Risk HPV DNA 616.4 Vulvar Abscess N76.4 795.05 R87.810 Test Positive 616.5 Ulcer Of Vulva N76.6 Unsatisfactory Cervical 795.08 R87.615 616.89 Vaginal Ulcer N76.5 Cytology Sample 623.1 Leukoplakia Of Vagina N89.4 795.10 Abnormal Pap Smear Result, Vagina R87.628 Vaginal High-Risk HPV DNA 623.5 Vaginal Discharge N89.8 795.15 R87.811 Test Positive 623.8 Vaginal Bleeding N93.9 Disorders Of Uterus And Ovary 623.8 Vaginal Cyst N89.8 218.9 Uterine Fibroid/Leiomyoma D25.9 Noninflammatory Disorder 623.9 N89.9 Of Vagina 256.39 Ovarian Failure E28.39 624.8 Vulvar Lesion N90.89 256.9 Ovarian -

How to Evaluate Vaginal Bleeding and Discharge
How to Evaluate Vaginal Bleeding and Discharge Is the bleeding normal or abnormal? When does vaginal discharge reflect something as innocuous as irritation caused by a new soap? And when does it signal something more serious? The authors’ discussion of eight actual patient presentations will help you through the next differential diagnosis for a woman with vulvovaginal complaints. By Vincent Ball, MD, MAJ, USA, Diane Devita, MD, FACEP, LTC, USA, and Warren Johnson, MD, CPT, USA bnormal vaginal bleeding or discharge is typically due to either inadequate levels of estrogen one of the most common reasons women or a persistent corpus luteum. Structural causes of come to the emergency department.1,2 bleeding include leiomyomas, endometrial polyps, or Because the possible underlying causes malignancy. Infectious etiologies include pelvic in- Aare diverse, the patient’s age, key historical factors, flammatory disease (PID). Additionally, a variety of and a directed physical examination are instrumental bleeding dyscrasias involving platelet or clotting fac- in deciding on diagnosis and treatment. This article tors can complicate the normal menstrual period. Iat- will review some common case presentations of rogenic causes of vaginal bleeding include hormone nonpregnant female patients with abnormal vaginal replacement therapy, steroid hormone contraception, bleeding, inflammation, or discharge. and contraceptive intrauterine devices.3-5 Anovulatory bleeding is common in perimenar- ABNORMAL VAGINAL BLEEDING chal girls as a result of an immature hypothalamic- To ensure appropriate patient management, “Is she pituitary axis and in perimenopausal women due to pregnant?” should be the first question addressed, declining levels of estrogen. During reproductive since some vulvovaginal signs and symptoms will years, dysfunctional uterine differ in significance and urgency depending on the bleeding (DUB) is the most >>FAST TRACK<< answer. -

Grading Pelvic Prolapse and Pelvic Floor Relaxation Using Dynamic Magnetic Resonance Imaging
ADULT UROLOGY GRADING PELVIC PROLAPSE AND PELVIC FLOOR RELAXATION USING DYNAMIC MAGNETIC RESONANCE IMAGING CRAIG V. COMITER, SANDIP P. VASAVADA, ZORAN L. BARBARIC, ANGELO E. GOUSSE, AND SHLOMO RAZ ABSTRACT Objectives. With significant vaginal prolapse, it is often difficult to differentiate among cystocele, enterocele, and high rectocele by physical examination alone. Our group has previously demonstrated the utility of magnetic resonance imaging (MRI) for evaluating pelvic prolapse. We describe a simple objective grading system for quantifying pelvic floor relaxation and prolapse. Methods. One hundred sixty-four consecutive women presenting with pelvic pain (n ϭ 39) or organ prolapse (n ϭ 125) underwent dynamic MRI. The “H-line” (levator hiatus) measures the distance from the pubis to the posterior anal canal. The “M-line” (muscular pelvic floor relaxation) measures the descent of the levator plate from the pubococcygeal line. The “O” classification (organ prolapse) characterizes the degree of visceral prolapse beyond the H-line. Results. The image acquisition time was 2.5 minutes per study. Each study cost $540. In the pain group, the H-line averaged 5.2 Ϯ 1.1 cm versus 7.5 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). The M-line averaged 1.9 Ϯ 1.2 cm in the pain group versus 4.1 Ϯ 1.5 cm in the prolapse group (P Ͻ0.001). Incidental pelvic pathologic features were commonly noted, including uterine fibroids, ovarian cysts, hydroureter, urethral diverticula, and foreign body. Conclusions. The HMO classification provides a straightforward and reproducible method for staging and quantifying pelvic floor relaxation and visceral prolapse. -
Vaginal Atrophy (VVA)
Information Sheet Vulvovaginal symptoms after menopause Key points • Vulvovaginal symptoms are numerous and varied and result from declining oestrogen levels. • Investigate any post- menopausal bleeding or malodorous discharge. • Management includes lifestyle changes as well as prescription and non- prescription medications. • As women age they will experience changes to their vagina and urinary system largely due to decreasing levels of the hormone oestrogen. • The changes, which may cause dryness, irritation, itching and pain with intercourse1-3 are known as the genito-urinary syndrome of menopause (GSM) and can affect up to 50% of postmenopausal women4. GSM was previously known as atrophic vaginitis or vulvovaginal atrophy (VVA). • Unlike some menopausal symptoms, such as hot flushes, which may disappear as time passes; genito-urinary problems often persist and may progress with time. Genito-urinary symptoms are associated both with menopause and with ageing4. • Changes in vaginal and urethral health occur with natural and surgical menopause, as well as after treatments for certain medical conditions (Please refer to AMS Information Sheet Vaginal health after breast cancer: A guide for patients). Why is oestrogen important for vaginal health? • The vaginal area needs adequate levels of oestrogen to maintain tissue integrity. • The vaginal epithelium contains oestrogen receptors which, when stimulated by the hormone, keep the walls thick and elastic. • When the amount of oestrogen in the body decreases this is commonly associated with dryness of the vulva and vagina. • A normal pre-menopausal vagina is naturally acidic, but with menopause it may become more alkaline, increasing susceptibility to urinary tract infections. A number of factors, including low oestrogen levels, have been implicated in the development of UTIs4-7 and vaginitis8-9 in postmenopausal women. -

The Woman with Postmenopausal Bleeding
THEME Gynaecological malignancies The woman with postmenopausal bleeding Alison H Brand MD, FRCS(C), FRANZCOG, CGO, BACKGROUND is a certified gynaecological Postmenopausal bleeding is a common complaint from women seen in general practice. oncologist, Westmead Hospital, New South Wales. OBJECTIVE [email protected]. This article outlines a general approach to such patients and discusses the diagnostic possibilities and their edu.au management. DISCUSSION The most common cause of postmenopausal bleeding is atrophic vaginitis or endometritis. However, as 10% of women with postmenopausal bleeding will be found to have endometrial cancer, all patients must be properly assessed to rule out the diagnosis of malignancy. Most women with endometrial cancer will be diagnosed with early stage disease when the prognosis is excellent as postmenopausal bleeding is an early warning sign that leads women to seek medical advice. Postmenopausal bleeding (PMB) is defined as bleeding • cancer of the uterus, cervix, or vagina (Table 1). that occurs after 1 year of amenorrhea in a woman Endometrial or vaginal atrophy is the most common cause who is not receiving hormone therapy (HT). Women of PMB but more sinister causes of the bleeding such on continuous progesterone and oestrogen hormone as carcinoma must first be ruled out. Patients at risk for therapy can expect to have irregular vaginal bleeding, endometrial cancer are those who are obese, diabetic and/ especially for the first 6 months. This bleeding should or hypertensive, nulliparous, on exogenous oestrogens cease after 1 year. Women on oestrogen and cyclical (including tamoxifen) or those who experience late progesterone should have a regular withdrawal bleeding menopause1 (Table 2).