Rehabilitation Institute Patient Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Channel Affiliate Market Timeframe of Move Call
TV Broadcasters’ Impact on Alabama Impact on AL 04 Broadcasters have an impact of $14.16 billion annually on Alabama’s economy. 31,130 Jobs 34 Commercial TV Stations Call Channel Affiliate Market Timeframe of Move WANN-CD 32 Independent Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WATC-DT 57 Independent Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WCIQ 7 Public Television Atlanta, GA (10) Phase 10: May 2, 2020 - Jul 3, 2020 WGTV 8 Public Television Atlanta, GA (10) Phase 10: May 2, 2020 - Jul 3, 2020 WHSG-TV 63 Trinity Broadcasting Network Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WIRE-CD 40 Independent Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WKTB-CD 38 Telemundo Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WPCH-TV 17 Independent Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WPXA-TV 14 ION Media Networks Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WSB-TV 2 ABC Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WSKC-CD 0 Independent Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WUPA 69 CW Television Network Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WUVG-DT 34 Univision Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 WYGA-CD 16 Independent-Spanish Atlanta, GA (10) Phase 5: Aug 3, 2019 - Sept 6, 2019 W47EI-D 0 Independent Birmingham (Anniston, Tuscaloosa), AL (45) Phase 5: Aug 3, 2019 - Sept 6, 2019 WABM 68 My Network TV Birmingham (Anniston, Tuscaloosa), AL (45) Phase 5: Aug 3, 2019 - Sept 6, 2019 WBRC 6 FOX Birmingham (Anniston, Tuscaloosa), AL (45) -

Nexstar Media Group to Host First Televised Debate in Race for Mississippi Governor
NEXSTAR MEDIA GROUP TO HOST FIRST TELEVISED DEBATE IN RACE FOR MISSISSIPPI GOVERNOR Nexstar Stations Partner with Select Broadcasters to Bring Live General Election Debate Coverage to Local Voters Across Mississippi Jackson, MS and IRVING, Texas (Oct 7, 2019) – Nexstar Media Group, Inc. (Nasdaq: NXST) (the “Company”) announced today that it will host the first live televised statewide debate in the race for Mississippi Governor between Lt. Governor Tate Reeves (R) and Attorney General Jim Hood (D) on Thursday, October 10 at 7 p.m. The Mississippi Governor’s Debate will last one hour. The debate will air on five Nexstar Broadcasting, Inc., stations across the state, including WJTV-TV (CBS), WHLT-TV (CBS), KZUP-CD (Ind), WREG-TV (CBS), and WFNA-TV (CW), in addition to select television broadcast partners including WMDN-TV (CBS) and WTVA-TV (ABC), and WXXV-TV (NBC), and radio partners SuperTalk, Mississippi Public Broadcasting, and Jackson State University. Local viewers may also access a live-stream of the debate online by visiting their local Nexstar station’s website (see table below for more information). The Mississippi Governor’s Debate is scheduled to take place on the campus of The University of Southern Mississippi at the Joe Paul Theater in Thad Cochran Center, 121 West Memorial Drive, in Hattiesburg. The debate will be moderated by Byron Brown, anchorman and political reporter for WJTV-TV, and Greg Hurst, anchorman. All questions to the candidates will be focused on topical local and regional issues impacting communities across Mississippi, including education, health care, infrastructure and the economy, as well as candidate- specific subjects. -

All Full-Power Television Stations by Dma, Indicating Those Terminating Analog Service Before Or on February 17, 2009
ALL FULL-POWER TELEVISION STATIONS BY DMA, INDICATING THOSE TERMINATING ANALOG SERVICE BEFORE OR ON FEBRUARY 17, 2009. (As of 2/20/09) NITE HARD NITE LITE SHIP PRE ON DMA CITY ST NETWORK CALLSIGN LITE PLUS WVR 2/17 2/17 LICENSEE ABILENE-SWEETWATER ABILENE TX NBC KRBC-TV MISSION BROADCASTING, INC. ABILENE-SWEETWATER ABILENE TX CBS KTAB-TV NEXSTAR BROADCASTING, INC. ABILENE-SWEETWATER ABILENE TX FOX KXVA X SAGE BROADCASTING CORPORATION ABILENE-SWEETWATER SNYDER TX N/A KPCB X PRIME TIME CHRISTIAN BROADCASTING, INC ABILENE-SWEETWATER SWEETWATER TX ABC/CW (DIGITALKTXS-TV ONLY) BLUESTONE LICENSE HOLDINGS INC. ALBANY ALBANY GA NBC WALB WALB LICENSE SUBSIDIARY, LLC ALBANY ALBANY GA FOX WFXL BARRINGTON ALBANY LICENSE LLC ALBANY CORDELE GA IND WSST-TV SUNBELT-SOUTH TELECOMMUNICATIONS LTD ALBANY DAWSON GA PBS WACS-TV X GEORGIA PUBLIC TELECOMMUNICATIONS COMMISSION ALBANY PELHAM GA PBS WABW-TV X GEORGIA PUBLIC TELECOMMUNICATIONS COMMISSION ALBANY VALDOSTA GA CBS WSWG X GRAY TELEVISION LICENSEE, LLC ALBANY-SCHENECTADY-TROY ADAMS MA ABC WCDC-TV YOUNG BROADCASTING OF ALBANY, INC. ALBANY-SCHENECTADY-TROY ALBANY NY NBC WNYT WNYT-TV, LLC ALBANY-SCHENECTADY-TROY ALBANY NY ABC WTEN YOUNG BROADCASTING OF ALBANY, INC. ALBANY-SCHENECTADY-TROY ALBANY NY FOX WXXA-TV NEWPORT TELEVISION LICENSE LLC ALBANY-SCHENECTADY-TROY AMSTERDAM NY N/A WYPX PAXSON ALBANY LICENSE, INC. ALBANY-SCHENECTADY-TROY PITTSFIELD MA MYTV WNYA VENTURE TECHNOLOGIES GROUP, LLC ALBANY-SCHENECTADY-TROY SCHENECTADY NY CW WCWN FREEDOM BROADCASTING OF NEW YORK LICENSEE, L.L.C. ALBANY-SCHENECTADY-TROY SCHENECTADY NY PBS WMHT WMHT EDUCATIONAL TELECOMMUNICATIONS ALBANY-SCHENECTADY-TROY SCHENECTADY NY CBS WRGB FREEDOM BROADCASTING OF NEW YORK LICENSEE, L.L.C. -
Image to PDF Conversion Tools
I I • • returns fo 'Ire "Chase Hour" fhls NBC [ IJB P RADIO GUIDE: The National Weekly of programs, pictures and personalities Rudy Vallee Quits after a Decade of Broadcasting IT WAS only yesterday, or perhaps a lillIe longer, Cover: When Nelson Local Boy: Bob Robin Bums is a local boy no when Rudy Vallee was singing "Rain" and ''I'm Eddy married last year, matter how far he strays from Van Buren, Arkansas. Just a Vagabond Lover" over a local New York station the carpers and croakers Recently he returned to his home in such triumph as advertising diamonds sold by a jewelry store 'way announced that his career formerly came only to world·conquering warriors up town. Lindy had just flown the Atlantic, Babe was finished. Tiley said and polar explorers. On that day a motion picture Ruth had hammered out sixty home runs, and Jack he was every girl's dream named "Our Leading Citizen" was given its premiere Dempsey had almost won back his championship man and no dream man performance in Van Buren and Bob Burns as the from Tunney. Mae West was playing in "Diamond could marry and remain leading citizen of the film was feted right and lell. Lil." People were humming "You're the CIeam in popular. They reckoned Governors and mayors and Arkansas big·shots came My Coffee" and "Button Up Your Overcoat." The boy without Nelson Eddy's from all over the slate to with the slightly nasal voice, the odd trick of timing determination to sing pay him tribute. We his words. -

(City/County) Published Editor Managing Editor Publisher Phone Fax 3 the Sun Herald (Biloxi/Harrison) Daily Stan Tiner Dorothy Wilson Ricky R
A BCDEFG 1 Media Outlet 2 Newspapers (City/County) Published Editor Managing Editor Publisher Phone Fax 3 The Sun Herald (Biloxi/Harrison) Daily Stan Tiner Dorothy Wilson Ricky R. Matthews 228-896-2100 228-896-2104 4 The Daily Leader (Brookhaven/Lincoln) Daily William O. Jacob Nanette Laster William O. Jacob 601-833-6961 601-833-6714 5 Press Register (Clarksdale/Cohoma) Daily Steve Stewart Steve Stewart 662-627-2201 662-624-5125 6 Bolivar Commercial (Cleveland/Bolivar) Daily Mark Williams Wayne Nichols Mark Williams 662-843-4241 662-843-1830 662-329-1521 or 7 Commercial Dispatch (Columbus/Lowndes) Daily Birney Imes III Dan E. Way 662-328-2427 662-329-8937 8 The Daily Corinthian (Corinth/Alcorn) Daily Reece Terry Mark Boehler 662-287-6111 662-287-3525 9 Delta Democrat-Times (Greenville/Washington) Daily Donald Adderton Truman Beasley 662-335-1155 662-335-2860 10 Commonwealth (Greenwood/Leflore) Daily Tom Kalich Tom Kalich 662-453-5312 662-453-2908 11 The Daily Star (Grenada/Grenada) Daily Terri Ferguson Joseph B. Lee III 662-226-4321 662-226-8310 12 Hattiesburg American ( Hattiesburg/Forrest) Daily David Petty Marilyn Mitchell 601-582-4321 601-584-3130 13 DeSoto Times Today (Hernando/DeSoto) Daily Rob Long Tom Pittman 662-429-6397 662-429-5229 14 DeSoto Times Today (Southaven/DeSoto) Daily Rob Long Tom Pittman 662-393-6397 662-393-6463 15 The Clarion Ledger (Jackson/Hinds) Daily Shawn McIntosh Bill Hunsberger 601-961-7000 601-961-7211 16 Leader-Call (Laurel/Jones) Daily Steve Swogentinsky 601-428-0551 601-426-3550 17 Enterprise-Journal (McComb/Pike) Daily Jack Ryan Karen Freeman Jack Ryan 601-684-2421 601-684-0836 18 The Meridian Star (Meridian/Lauderdale) Daily Buddy Bynum John Bohl Paul M. -

List of Directv Channels (United States)
List of DirecTV channels (United States) Below is a numerical representation of the current DirecTV national channel lineup in the United States. Some channels have both east and west feeds, airing the same programming with a three-hour delay on the latter feed, creating a backup for those who missed their shows. The three-hour delay also represents the time zone difference between Eastern (UTC -5/-4) and Pacific (UTC -8/-7). All channels are the East Coast feed if not specified. High definition Most high-definition (HDTV) and foreign-language channels may require a certain satellite dish or set-top box. Additionally, the same channel number is listed for both the standard-definition (SD) channel and the high-definition (HD) channel, such as 202 for both CNN and CNN HD. DirecTV HD receivers can tune to each channel separately. This is required since programming may be different on the SD and HD versions of the channels; while at times the programming may be simulcast with the same programming on both SD and HD channels. Part time regional sports networks and out of market sports packages will be listed as ###-1. Older MPEG-2 HD receivers will no longer receive the HD programming. Special channels In addition to the channels listed below, DirecTV occasionally uses temporary channels for various purposes, such as emergency updates (e.g. Hurricane Gustav and Hurricane Ike information in September 2008, and Hurricane Irene in August 2011), and news of legislation that could affect subscribers. The News Mix channels (102 and 352) have special versions during special events such as the 2008 United States Presidential Election night coverage and during the Inauguration of Barack Obama. -

Ascertainment of Community Needs by Public Television Stations: a Study of Kpbs, Wosu, Wviz, Weta, and the Alabama Educational Television Commission
72-4421 BENNETT, Sandra Williams, 1942- ASCERTAINMENT OF COMMUNITY NEEDS BY PUBLIC TELEVISION STATIONS: A STUDY OF KPBS, WOSU, WVIZ, WETA, AND THE ALABAMA EDUCATIONAL TELEVISION COMMISSION. The Ohio State University, Ph.D., 1971 Mass Communications University Microfilms, A XEROK Company. Ann Arbor, Michigan <§> Copyright by Sandra Williams Bennett 1971 THIS DISSERTATION HAS BEEN MICROFILMED EXACTLY AS RECEIVED ASCERTAINMENT OF COMMUNITY NEEDS BY PUBLIC TELEVISION STATIONS: A STUDY OF KPBS, WOSU, WVIZ, WETA, AND THE ALABAMA EDUCATIONAL TELEVISION COMMISSION DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Sandra Williams Bennett, B.S. in Ed., M.A. * * * * * The Ohio State University 1971 Approved by Department of Speech Communications PLEASE NOTE: Some papes have small and indistinct print. Filmed as received. UNIVERSITY MICROFILMS. ACKNOWLEDGMENTS The successful completion of this study was to tally dependent upon cooperation, encouragement, assis tance, time and devotion--of others. For their coopera tion in freely and openly talking with me, I thank the men and women at each of the stations I visited. For their encouragement and assistance, I thank my graduate professors, and especially my committee members and ad viser. A special note of thanks for their continued en couragement and assistance throughout my graduate studies goes to Dr. Robert Hilliard and Allen Myers at the Federal Communications Commission. And especially to my husband Dick, and son, Richard Daniel, who cooperated, encouraged, assisted, gave of their time, but most especially remained devoted— I thank you. Sandra Jean Williams Bennett ii VITA May 27, 194 2 ..... -

Television Channel Fcc Assignments for Us Channel Repacking (To Channels Less Than 37)
TELEVISION CHANNEL FCC ASSIGNMENTS FOR US CHANNEL REPACKING (TO CHANNELS LESS THAN 37) March 29, 2017 LEGEND FINAL TELEVISION CHANNEL ASSIGNMENT INFORMATION RELATED TO INCENTIVE AUCTION REPACKING Technical Parameters for Post‐Auction Table of Allotments NOTE: These results are based on the 20151020UCM Database, 2015Oct_132Settings.xml study template, and TVStudy version 1.3.2 (patched) FacID Site Call Ch PC City St Lat Lon RCAMSL HAAT ERP DA AntID Az 21488 KYES‐TV 5 5 ANCHORAGE AK 612009 1493055 614.5 277 15 DA 93311 0 804 KAKM 8 8 ANCHORAGE AK 612520 1495228 271.2 240 50 DA 67943 0 10173 KTUU‐TV 10 10 ANCHORAGE AK 612520 1495228 271.2 240 50 DA 89986 0 13815 KYUR 12 12 ANCHORAGE AK 612520 1495228 271.2 240 41 DA 68006 0 35655 KTBY 20 20 ANCHORAGE AK 611309 1495332 98 45 234 DA 90682 0 49632 KTVA 28 28 ANCHORAGE AK 611131 1495409 130.6 60.6 28.9 DA 73156 0 25221 KDMD 33 33 ANCHORAGE AK 612009 1493056 627.9 300.2 17.2 DA 102633 0 787 KCFT‐CD 35 35 ANCHORAGE AK 610400 1494444 539.7 0 15 DA 109112 315 64597 KFXF 7 7 FAIRBANKS AK 645518 1474304 512 268 6.1 DA 91018 0 69315 KUAC‐TV 9 9 FAIRBANKS AK 645440 1474647 432 168.9 30 ND 64596 K13XD‐D 13 13 FAIRBANKS AK 645518 1474304 521.6 0 3 DA 105830 170 13813 KATN 18 18 FAIRBANKS AK 645518 1474258 473 230 16 ND 49621 KTVF 26 26 FAIRBANKS AK 645243 1480323 736 471 27 DA 92468 110 8651 KTOO‐TV 10 10 JUNEAU AK 581755 1342413 37 ‐363 1 ND 13814 KJUD 11 11 JUNEAU AK 581804 1342632 82 ‐290 0.14 DA 78617 0 60520 KUBD 13 13 KETCHIKAN AK 552058 1314018 100 ‐71 0.413 DA 104820 0 20015 KJNP‐TV 20 20 NORTH -

Emily Roane Peck
Emily Roane Peck Education: M.P.A Public Administration/Political Science Auburn University Montgomery, Graduated 1994 B.A., Broadcast Journalism University of Mississippi, Graduated 1981 Certificate of Broadcast Meteorology Mississippi State University, 1990 Achievements: 2020 – Completed UAH Quality Education Practices Online Course to certify the PSC 103 course for teaching online. 2019 – Alabama Commission on Higher Education Grant Recipient to develop an online course using Open Education Resources 2019 – Participated in Super Teacher for Excellence program at Calhoun Community College 2018 – Completed training to become a Peer Reviewer for Quality Matters 2016 – Online course for Calhoun Community College certified by Quality Matters as meeting good standards. 2016 – Completed UAH Quality Education Practices Online Course to certify the PSC 101 Course for teaching online. 2000 – Grant Recipient for the Democracy Project, Public Broadcasting Service, and the Corporation for Public Broadcasting. 1997 - Political Science Alumnae Award, Auburn University Montgomery 1997 – Douglas Cannon Award for Medical Journalism, Presented by the Alabama Medical Association. 1996 – Selected to participate in the RIAS Berlin Commission, a German American Journalist Exchange program. Spent 6 weeks touring Germany and meeting with Journalists to discuss political events and reporting methods. 1992 – Recipient of Troy University’s Hector Award for Meritorious Public Service Reporting 1991 – 1st place recipient of National Federation of Press Women Award -

Federal Communications Commission DA 04-1054 Before the Federal
Federal Communications Commission DA 04-1054 Before the Federal Communications Commission Washington, D.C. 20554 In the Matter of: ) ) WTVA, Inc. ) ) CSR-6147-N For Waiver of Section 76.92(f) of the ) Commission’s Rules ) MEMORANDUM OPINION AND ORDER Adopted: April 15. 2004 Released: April 21, 2004 By the Deputy Chief, Media Bureau: I. INTRODUCTION 1. WTVA, Inc., licensee of television broadcast station WTVA (NBC, Ch. 9), and permittee of WTVA-DT (Ch. 58), Tupelo-Columbus, Mississippi (“WTVA”), has filed a petition for special relief seeking a waiver of the Commission’s significantly viewed exception to the network nonduplication rules.1 An opposition to this petition was filed on behalf of Raycom America, Inc., licensee of station WMC-TV (NBC, Ch. 5), Memphis, Tennessee (“WMC-TV”) to which WTVA has replied. II. BACKGROUND 2. Upon the request of a local television station with exclusive rights to distribute a network program, a cable operator generally may not carry a duplicating network program broadcast by a distant station.2 Under Section 76.92(f) of the Commission’s rules, however, an otherwise distant station is exempt from the application of the network nonduplication rules if it is considered “significantly viewed” in a relevant community.3 The Commission’s rules generally provide stations such protection within a station’s 35-mile geographic zone.4 However, a local station may not exercise this right if an otherwise distant station is considered “significantly viewed” within the community served by the cable system. The significantly viewed exception to the Commission’s exclusivity rules is based on an otherwise distant 1See 47 C.F.R. -
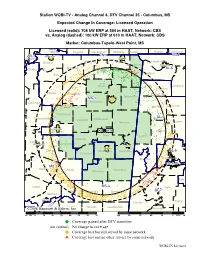
Columbus-Tupelo-West Point, MS
Station WCBI-TV · Analog Channel 4, DTV Channel 35 · Columbus, MS Expected Change In Coverage: Licensed Operation Licensed (solid): 708 kW ERP at 584 m HAAT, Network: CBS vs. Analog (dashed): 100 kW ERP at 610 m HAAT, Network: CBS Market: Columbus-Tupelo-West Point, MS TN-9 Shelby Fayette Hardeman McNairy Hardin Wayne Lawrence AR-1 Southaven TN-7 TN-4 Crittenden Corinth DeSoto Benton Alcorn Lauderdale Tishomingo Florence Marshall AL-5 Tunica Tippah Colbert Tate Prentiss Union Lawrence Franklin Panola Lafayette Lee Itawamba MS-1 Tupelo Quitman Pontotoc Marion Winston Yalobusha AL-4 Tallahatchie Calhoun Chickasaw Monroe Walker Grenada Grenada A4 D35 Fayette Clay Lamar Webster Leflore Greenwood Montgomery Columbus Starkville Carroll Oktibbeha Lowndes AL-6 Choctaw Pickens Tuscaloosa Tuscaloosa MS-2 Holmes Attala Noxubee Winston Bibb Greene Yazoo MS-3 Hale AL-7 Leake Neshoba Kemper Madison Canton Sumter Perry Scott 2008 HammettRankin & Edison, Inc. Newton Lauderdale Marengo 10 MI 0 10 20 30 40 50 60 70 100 80 60 40 20 0 KM 20 Coverage gained after DTV transition (no symbol) No change in coverage Coverage lost but still served by same network Coverage lost and no other service by same network WCBI-TV Licensed Station WMAB-TV · Analog Channel 2, DTV Channel 10 · Mississippi State, MS Expected Change In Coverage: Licensed Operation Licensed (solid): 4.30 kW ERP at 349 m HAAT, Network: PBS vs. Analog (dashed): 100 kW ERP at 379 m HAAT, Network: PBS Market: Columbus-Tupelo-West Point, MS Benton AL-5 Tippah Colbert AR-1 Tunica Tate Marshall Tishomingo -

The Northeast Mississippi
THE NORTHEAST MISSISSIPPI A MONTHLY PUBLICATION OF JOURNAL PUBLISHING AND THE COMMUNITY DEVELOPMENT FOUNDATION AUGUST 2009 CONSTRUCTION, HOUSING MARKET LOOK AHEAD Prsrt Std US Postage PAID Tupelo,MS Permit #353 PAGE 2 BUSINESS JOURNAL FRIDAY, AUGUST 7, 2009 Commercial construction looks for rebound By DENNIS SEID out of every three construction Commercial permits, the rise in government con- “There’s not enough work to go BUSINESS JOURNAL jobs. struction helped offset a de- Since the recession started And according to the BLS, January-June cline in new malls, office build- around for everyone,to be honest. 20 months ago, much atten- the nationwide construction ings and other commercial We’ve been fortunate that we’ve been tion has been paid to the bat- unemployment rate rose from Oxford Starkville Tupelo nonresidential building, which tered housing market. 5.9 percent in 2007 to 8.2 per- fell 0.5 percent. able to keep the vast majority of our And the construction indus- cent last year. Currently, it’s 2008 25 107 12 In Northeast Mississippi, try is feeling the pain. tracking at a 17.4 percent rate. 2009 6 138 11 three cities had mixed results workers employed.” According to the Associated Some Northeast Mississippi over the past year. Jerry Maxcy General Contractors of Ameri- construction companies say In Tupelo, the number of they’re hurting, too. ca, construction dropped in all commercial permits in the first senior vice president of Jesco Inc. “There’s not enough work to some light at the end of the but 19 communities nation- half of 2009 nearly matched go around for everyone, to be dark tunnel.