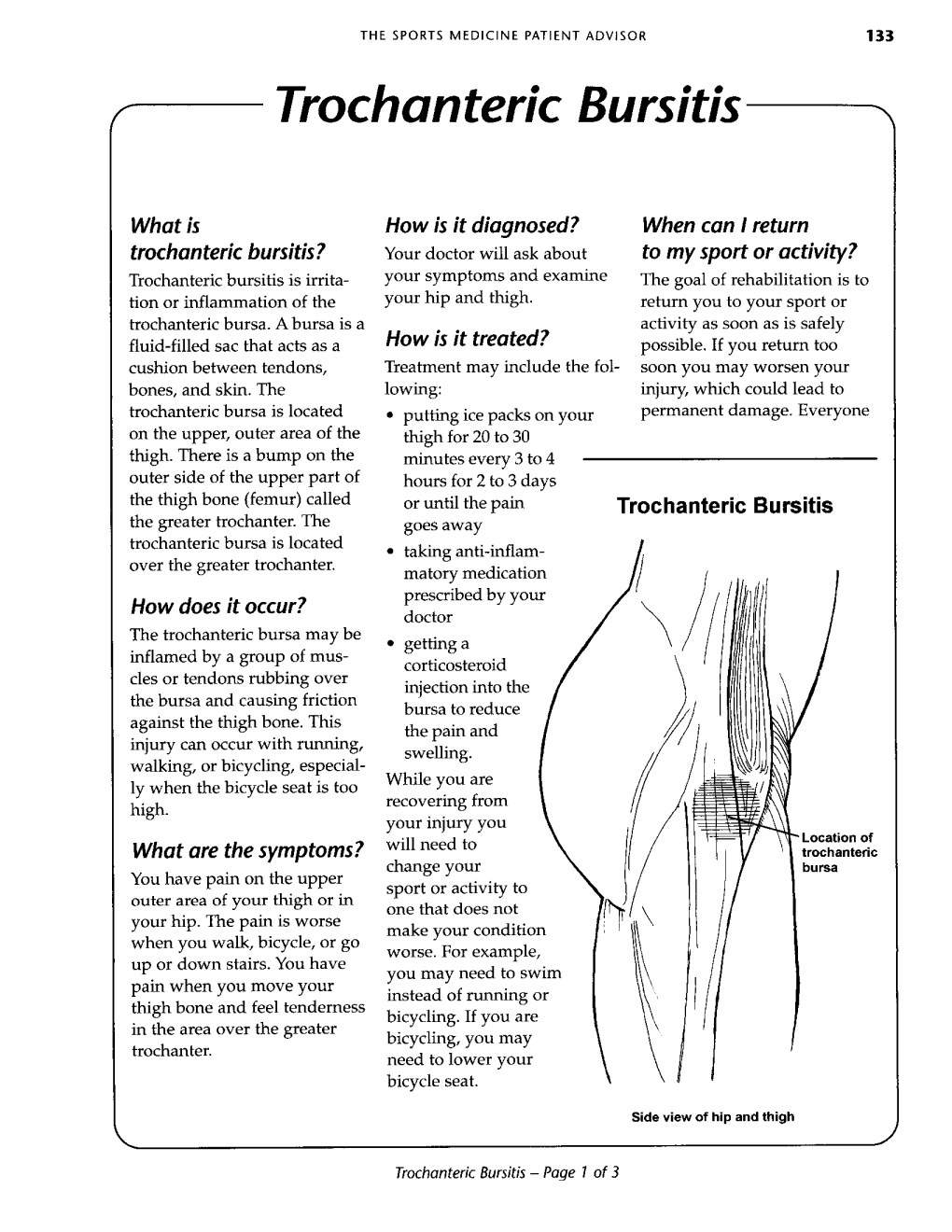
Trochanteric Bursitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Iliopsoas Tendonitis/Bursitis Exercises
ILIOPSOAS TENDONITIS / BURSITIS What is the Iliopsoas and Bursa? The iliopsoas is a muscle that runs from your lower back through the pelvis to attach to a small bump (the lesser trochanter) on the top portion of the thighbone near your groin. This muscle has the important job of helping to bend the hip—it helps you to lift your leg when going up and down stairs or to start getting out of a car. A fluid-filled sac (bursa) helps to protect and allow the tendon to glide during these movements. The iliopsoas tendon can become inflamed or overworked during repetitive activities. The tendon can also become irritated after hip replacement surgery. Signs and Symptoms Iliopsoas issues may feel like “a pulled groin muscle”. The main symptom is usually a catch during certain movements such as when trying to put on socks or rising from a seated position. You may find yourself leading with your other leg when going up the stairs to avoid lifting the painful leg. The pain may extend from the groin to the inside of the thigh area. Snapping or clicking within the front of the hip can also be experienced. Do not worry this is not your hip trying to pop out of socket but it is usually the iliopsoas tendon rubbing over the hip joint or pelvis. Treatment Conservative treatment in the form of stretching and strengthening usually helps with the majority of patients with iliopsoas bursitis. This issue is the result of soft tissue inflammation, therefore rest, ice, anti- inflammatory medications, physical therapy exercises, and/or injections are effective treatment options. -

Pes Anserine Bursitis
BRIGHAM AND WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: Pes Anserine Bursitis ICD 9 Codes: 726.61 Case Type / Diagnosis: The pes anserine bursa lies behind the medial hamstring, which is composed of the tendons of the sartorius, gracilis and semitendinosus (SGT) muscles. Because these 3 tendons splay out on the anterior aspect of the tibia and give the appearance of the foot of a goose, pes anserine bursitis is also known as goosefoot bursitis.1 These muscles provide for medial stabilization of the knee by acting as a restraint to excessive valgus opening. They also provide a counter-rotary torque function to the knee joint. The pes anserine has an eccentric role during the screw-home mechanism that dampens the effect of excessively forceful lateral rotation that may accompany terminal knee extension.2 Pes anserine bursitis presents as pain, tenderness and swelling over the anteromedial aspect of the knee, 4 to 5 cm below the joint line.3 Pain increases with knee flexion, exercise and/or stair climbing. Inflammation of this bursa is common in overweight, middle-aged women, and may be associated with osteoarthritis of the knee. It also occurs in athletes engaged in activities such as running, basketball, and racquet sports.3 Other risk factors include: 1 • Incorrect training techniques, or changes in terrain and/or distanced run • Lack of flexibility in hamstring muscles • Lack of knee extension • Patellar malalignment Indications for Treatment: • Knee Pain • Knee edema • Decreased active and /or passive ROM of lower extremities • Biomechanical dysfunction lower extremities • Muscle imbalances • Impaired muscle performance (focal weakness or general conditioning) • Impaired function Contraindications: • Patients with active signs/symptoms of infection (fever, chills, prolonged and obvious redness or swelling at hip joint). -

Gluteal Tendinopathy
Gluteal Tendinopathy What is a Gluteal Tendinopathy? In lying Up until recently hip bursitis was diagnosed as the main Either on your bad hip or with bad cause of lateral hip pain but recent studies suggest that an hip hanging across body like so irritation of the gluteus muscle tendon is the likeliest cause. The tendon attaches onto a bony prominence (greater trochanter) and it is here that the tendon is subject to All these positions lead to increase friction of the tendon, compressive forces leading to irritation. can cause pain and slow the healing process. This can result in pain over the lateral hip which can refer down the outside For sleeping you might like to try these positions: of the thigh and into the knee. How common is it? Gluteal tendinopathy is relatively common affecting 10-25% of the population. It is 3 times more prevalent in women than men and is most common in women between the ages of 40 and 60. One of the reasons for this is women It is also important to modify your activity. Avoid or reduce tend to have a greater angle at their hip joint increasing things that flare up your pain, this could be climbing stairs compressive forces on the tendon. or hills or those longer walks/runs. Signs and Symptoms Exercise Therapy • Pain on the outside of your hip, can refer down outside of the thigh to the knee This is best administered by a Physiotherapist to suit the • Worse when going up and/or down stairs individual but below is a rough guide to exercises which • Worse lying on affected side (and sometimes on the can help a gluteal tendinopathy. -
A New Caenagnathid Dinosaur from the Upper Cretaceous Wangshi
www.nature.com/scientificreports OPEN A new caenagnathid dinosaur from the Upper Cretaceous Wangshi Group of Shandong, China, with Received: 12 October 2017 Accepted: 7 March 2018 comments on size variation among Published: xx xx xxxx oviraptorosaurs Yilun Yu1, Kebai Wang2, Shuqing Chen2, Corwin Sullivan3,4, Shuo Wang 5,6, Peiye Wang2 & Xing Xu7 The bone-beds of the Upper Cretaceous Wangshi Group in Zhucheng, Shandong, China are rich in fossil remains of the gigantic hadrosaurid Shantungosaurus. Here we report a new oviraptorosaur, Anomalipes zhaoi gen. et sp. nov., based on a recently collected specimen comprising a partial left hindlimb from the Kugou Locality in Zhucheng. This specimen’s systematic position was assessed by three numerical cladistic analyses based on recently published theropod phylogenetic datasets, with the inclusion of several new characters. Anomalipes zhaoi difers from other known caenagnathids in having a unique combination of features: femoral head anteroposteriorly narrow and with signifcant posterior orientation; accessory trochanter low and confuent with lesser trochanter; lateral ridge present on femoral lateral surface; weak fourth trochanter present; metatarsal III with triangular proximal articular surface, prominent anterior fange near proximal end, highly asymmetrical hemicondyles, and longitudinal groove on distal articular surface; and ungual of pedal digit II with lateral collateral groove deeper and more dorsally located than medial groove. The holotype of Anomalipes zhaoi is smaller than is typical for Caenagnathidae but larger than is typical for the other major oviraptorosaurian subclade, Oviraptoridae. Size comparisons among oviraptorisaurians show that the Caenagnathidae vary much more widely in size than the Oviraptoridae. Oviraptorosauria is a clade of maniraptoran theropod dinosaurs characterized by a short, high skull, long neck and short tail. -

The Anatomy of the Deep Infrapatellar Bursa of the Knee Robert F
0363-5465/98/2626-0129$02.00/0 THE AMERICAN JOURNAL OF SPORTS MEDICINE, Vol. 26, No. 1 © 1998 American Orthopaedic Society for Sports Medicine The Anatomy of the Deep Infrapatellar Bursa of the Knee Robert F. LaPrade,* MD Department of Orthopaedic Surgery, University of Minnesota, Minneapolis, Minnesota ABSTRACT knee joint, and to define a consistent surgical approach to the deep infrapatellar bursa. Disorders of the deep infrapatellar bursa are important to include in the differential diagnosis of anterior knee pain. Knowledge regarding its anatomic location can MATERIALS AND METHODS aid the clinician in establishing a proper diagnosis. Fifty cadaveric knees were dissected, and the deep infrapa- Thorough dissections of the anterior aspect of the knee of tellar bursa had a consistent anatomic location in all 50 nonpaired cadaveric knees were performed. There were specimens. The deep infrapatellar bursa was located 27 male and 23 female cadaveric knees with 25 right and directly posterior to the distal 38% of the patellar ten- 25 left knees. The average age of the specimens was 71.8 don, just proximal to its insertion on the tibial tubercle. years (range, 42 to 93). After the skin and subcutaneous There was no communication to the knee joint. Its tissues of the anterior aspect of the knee were carefully average width at the most proximal margin of the tibial dissected away, an approach to the deep infrapatellar tubercle was slightly wider than the average distal bursa of the knee was made through medial and lateral width of the patellar tendon. It was found to be partially arthrotomy incisions along the patella, followed by compartmentalized, with a fat pad apron extending transection of the quadriceps tendon from the patella. -

Percutaneous Reduction Techniques
AAOS 2016 Specialty Day Orthopaedic Trauma Associacion (OTA) Percutaneous Reduction Techniques Christian Krettek Trauma Department, Hannover Medical School, Germany [email protected] www.mhh-unfallchirurgie.de Short segment tibial fractures can be stabilized using different implants like plates, screws, external fixators and nails. This syllabus deals mainly with reduction techniques in the context of the use of intramedullary nails. 1.1 PREOPERATIVE PLANNING AND MANAGEMENT 1.1.1 Primary shortening and secondary overdistraction eases definitive nailing In the acute setting primary shortening of a shaft fracture is a helpful strategy to de- crease soft tissue tension and intra-compartmental pressure. However, reduction gets more difficult and more time consuming, the longer the fracture is kept in a shortened position. The concept of primary shortening (acute phase) and secondary (after 3 or 4 days) overdistraction eases definitive nailing. Using a electro-mechanical load cell, our group has compared the reduction forces in patients undergoing femoral nailing after Damage Control in shortend vs overdistracted fracture configuration. In the overdistrac- tion group, the reduction forces were lower (200 N +/-43.1 N vs. 336 N +/- 51.9 N, p = 0.007) and the reduction time was shorter (5.8 min +/-4.0 min vs. 28.3 min +/-21.8 min, p = 0.056). It was concluded, that DCO with the fracture shortened leads to higher restrai- ning forces & prolonged reduction time. Overdistraction should be performed as soon as possible under careful soft-tissue monitoring [1a, 2a]. Primary shortening and secondary overdistraction eases definitive nailing Example of a femoral shaft fracture stabilized in shortening first with an external fixator. -

Case Report Septic Infrapatellar Bursitis in an Immunocompromised Female
Hindawi Case Reports in Orthopedics Volume 2018, Article ID 9086201, 3 pages https://doi.org/10.1155/2018/9086201 Case Report Septic Infrapatellar Bursitis in an Immunocompromised Female Kenneth Herring , Seth Mathern, and Morteza Khodaee 1Department of Family Medicine, University of Colorado School of Medicine, 3055 Roslyn Street, Denver, CO 80238, USA Correspondence should be addressed to Kenneth Herring; [email protected] Received 8 April 2018; Revised 19 April 2018; Accepted 20 April 2018; Published 6 June 2018 Academic Editor: John Nyland Copyright © 2018 Kenneth Herring et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Bursitis is a relatively common occurrence that may be caused by traumatic, inflammatory, or infectious processes. Septic bursitis most commonly affects the olecranon and prepatellar bursae. Staphylococcus aureus accounts for 80% of all septic bursitis, and most cases affect men and are associated with preceding trauma. We present a case of an 86-year-old female with an atypical septic bursitis involving the infrapatellar bursa. Not only are there very few reported cases of septic infrapatellar bursitis, but also this patient’s case is particularly unusual in that she is a female with no preceding trauma who had Pseudomonas aeruginosa on aspirate. The case also highlights the diagnostic workup of septic bursitis through imaging modalities and aspiration. This patient had full resolution of her septic bursitis with appropriate IV antibiotics. 1. Introduction and relative superficial location, the olecranon and prepa- tellar bursae are the most common sites of septic bursitis The human body contains upwards of 150 bursae, many [3, 4]. -

Plantar Fasciitis Thomas Trojian, MD, MMB, and Alicia K
Plantar Fasciitis Thomas Trojian, MD, MMB, and Alicia K. Tucker, MD, Drexel University College of Medicine, Philadelphia, Pennsylvania Plantar fasciitis is a common problem that one in 10 people will experience in their lifetime. Plantar fasciopathy is an appro- priate descriptor because the condition is not inflammatory. Risk factors include limited ankle dorsiflexion, increased body mass index, and standing for prolonged periods of time. Plantar fasciitis is common in runners but can also affect sedentary people. With proper treatment, 80% of patients with plantar fasciitis improve within 12 months. Plantar fasciitis is predominantly a clinical diagnosis. Symp- toms are stabbing, nonradiating pain first thing in the morning in the proximal medioplantar surface of the foot; the pain becomes worse at the end of the day. Physical examination findings are often limited to tenderness to palpation of the proximal plantar fascial insertion at the anteromedial calcaneus. Ultrasonogra- phy is a reasonable and inexpensive diagnostic tool for patients with pain that persists beyond three months despite treatment. Treatment should start with stretching of the plantar fascia, ice massage, and nonsteroidal anti-inflamma- tory drugs. Many standard treatments such as night splints and orthoses have not shown benefit over placebo. Recalcitrant plantar fasciitis can be treated with injections, extracorporeal shock wave therapy, or surgical procedures, although evidence is lacking. Endoscopic fasciotomy may be required in patients who continue to have pain that limits activity and function despite exhausting nonoperative treatment options. (Am Fam Physician. 2019; 99(12):744-750. Copyright © 2019 American Academy of Family Physicians.) Illustration by Todd Buck Plantar fasciitis (also called plantar fasciopathy, reflect- than 27 kg per m2 (odds ratio = 3.7), and spending most ing the absence of inflammation) is a common problem of the workday on one’s feet 4,5 (Table 1 6). -

Bursitis of the Knee
Bursitis of the knee What is bursitis? The diagram below shows the position of the Bursitis means inflammation within a bursa. A prepatellar and infrapatellar bursa in the knee. bursa is a small sac of fluid with a thin lining. There are a number of bursae in the body. Bursae are normally found around joints and in places where ligaments and tendons pass over bones and are there to stop the ligaments and bone rubbing together. What is prepatellar bursitis? Prepatellar bursitis is a common bursitis in the knee and can also be known as ‘housemaid’s knee’. There are four bursae located around the knee joint. They are all prone to inflammation. What causes prepatellar bursitis? There are a number of different things that can cause prepatellar bursitis, such as: • A sudden, one-off injury to the knee such as a fall or direct blow on to the knee during sport. People receiving steroid treatment or those on chemotherapy treatment for cancer are also at • Recurrent minor injury to the knee such as an increased risk of developing bursitis. spending long periods of time kneeling down, i.e. at work or whilst cleaning. Prepatellar bursitis is more common in tradesmen who spend long periods of time Infection: the fluid in the prepatellar bursa sac kneeling. For example, carpet fitters, concrete can become infected and cause bursitis. This is finishers and roofers. particularly common in children with prepatellar bursitis and usually follows a cut, scratch or injury to the skin on the surface of the knee. This What are the symptoms of injury allows bacteria (germs) to spread infection prepatellar bursitis? into the bursa. -

Congenital Abnormalities of the Femur
Arch Dis Child: first published as 10.1136/adc.36.188.410 on 1 August 1961. Downloaded from CONGENITAL ABNORMALITIES OF THE FEMUR BY P. A. RING From the Royal College of Surgeons (RECEIVED FOR PUBLICATION NOVEMBER 25, 1960) Congenital defects of the femur vary from simple tion of its incidence is difficult to obtain, but it hypoplasia of the bone to complete absence. appears to be the commonest congenital defect Classification of these defects has been suggested causing major abnormalities of limb growth. by Nilsonne (1928) and by Mouchet and Ibos (1928), but neither has met with general acceptance. In more recent years Golding (1939, 1948) has demon- Clinical Features strated the close association of the short femur with There is no evidence that this is a familial disorder, congenital coxa vara, and has emphasized that and careful inquiry of the parents has revealed no these are variations of the same underlying abnor- evidence of other congenital disorders within the mality. The clinical distinction between the various immediate family. The history of the pregnancy types of femoral defect is important as a guide to and delivery has failed to indicate any significant the prognosis of limb development. infection or abnormality at this time. In most From an examination of patients with congenital patients the abnormality is apparent at birth, but abnormalities of the femur the following classifica- where the inequality of leg length is slight, the by copyright. tion is suggested: diagnosis may not be made until the child begins to 1. Simple femoral hypoplasia. walk. To ordinary clinical testing the abnormality 2. -

Periprosthetic Fractures
Periprosthetic Fractures SRS 2017 Stephen R Smith Orthopaedic Surgeon Northeast Nebraska Orthopaedics P C Norfolk Nebraska SRS 2017 Periprosthetic Fractures Fractures around Joint Replacements Mostly Lower Limb Knee Arthroplasty 700,000/ yr. Hip Arthroplasty 350,000/yr. Shoulder Arthroplasty ? 60,000/yr. Elbow Arthroplasty ? 20,000/yr. Periprosthetic Fractures Incidence Increasing due Increasing Demand and High Demands of Older Patients Projections 2025 2,000,000 (2 million) Knee Replacements 750,000 Total Hip Replacements Periprosthetic Fractures Risk Factors Mechanical Patient Factors Implant Loosening Rheumatoid Arthritis Chronic Steroid Use Neurologic Osteolysis Disease/Disorders Osteoporosis Osteopenia Femoral Notching Female Gender (Above TKA) Increasing Age SRS 2017 Periprosthetic Fractures Incidence Hip Intraoperative Acetabulum Cemented 0.2% Uncemented 0.4% During Impaction Under reaming> 2mm, Osteoporosis, Dysplasia Radiation Periprosthetic Fractures Incidence Hip Intraoperative Primary 0.1-5% Classification Osteoporosis,Cementless, Technique, Revision, Minimally Invasive, Revision 3-21% Periprosthetic Fractures Risk Factors DON’T FALL Remove Loose Rugs Minimize Stair Use Rail Stay Home in Bad Weather!!! Use Common Sense SRS 2017 Periprosthetic Fractures Risk Factors This Is Ice DON’T FALL Remove Loose Rugs Minimize Stair Use Rail Stay Home in Bad Weather!!! Use Common Sense SRS 2017 Periprosthetic Fractures Incidence Knee Intraoperative ?? Occasional Medial Femoral Condyle Often Tibial Crack after Stem Impaction Postoperative -

Fracture of the Lesser Trochanter As a Sign of Undiagnosed Tumor Disease in Adults Christian Herren*, Christian D
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Herren et al. Eur J Med Res (2015) 20:72 DOI 10.1186/s40001-015-0167-8 CASE REPORT Open Access Fracture of the lesser trochanter as a sign of undiagnosed tumor disease in adults Christian Herren*, Christian D. Weber, Miguel Pishnamaz, Thomas Dienstknecht, Philipp Kobbe, Frank Hildebrand and Hans‑Christoph Pape Abstract Isolated avulsion fractures of the pelvic ring are rare and occur predominantly in adolescent athletes. Isolated fractures of the lesser trochanter are reported to be pathognomic for tumor diseases in adults. We present a case of a female patient with an isolated avulsion of the lesser trochanter after treatment by her chiropractor. After staging exami‑ nation, we determine the diagnosis of a left-sided carcinoma of the mamma. Additional imaging shows multiple metastases in liver, spine and pelvis. Palliative therapy has started over the course of time. We suggest, on suspicion of a malignant metastatic process, further investigation. Keywords: Fracture, Lesser trochanter, Metastatic, Tumor disease Background described unexplained weight loss of 5 kg in 4 months. Isolated fractures of the lesser trochanter are uncommon Sporadic onset of night sweats was also reported. She had and have been reported predominantly in adolescent ath- no other musculoskeletal or constitutional diseases in her letes [1]. This injury is caused by severe impact, usually medical history. Physical examination showed tenderness in context of contact sports and following a forceful and in the right groin, almost preserved passive mobility of sudden muscle contraction of the iliopsoas with avulsion the right hip joint in the full range of motion.