Iliopsoas Muscle and Postural Stability
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Static Stretching Time Required to Reduce Iliacus Muscle Stiffness
Sports Biomechanics ISSN: 1476-3141 (Print) 1752-6116 (Online) Journal homepage: https://www.tandfonline.com/loi/rspb20 Static stretching time required to reduce iliacus muscle stiffness Shusuke Nojiri, Masahide Yagi, Yu Mizukami & Noriaki Ichihashi To cite this article: Shusuke Nojiri, Masahide Yagi, Yu Mizukami & Noriaki Ichihashi (2019): Static stretching time required to reduce iliacus muscle stiffness, Sports Biomechanics, DOI: 10.1080/14763141.2019.1620321 To link to this article: https://doi.org/10.1080/14763141.2019.1620321 Published online: 24 Jun 2019. Submit your article to this journal Article views: 29 View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=rspb20 SPORTS BIOMECHANICS https://doi.org/10.1080/14763141.2019.1620321 Static stretching time required to reduce iliacus muscle stiffness Shusuke Nojiri , Masahide Yagi, Yu Mizukami and Noriaki Ichihashi Human Health Sciences, Graduate School of Medicine, Kyoto University, Kyoto, Japan ABSTRACT ARTICLE HISTORY Static stretching (SS) is an effective intervention to reduce muscle Received 25 September 2018 stiffness and is also performed for the iliopsoas muscle. The iliop- Accepted 9 May 2019 soas muscle consists of the iliacus and psoas major muscles, KEYWORDS among which the former has a greater physiological cross- Iliacus muscle; static sectional area and hip flexion moment arm. Static stretching stretching; ultrasonic shear time required to reduce muscle stiffness can differ among muscles, wave elastography and the required time for the iliacus muscle remains unclear. The purpose of this study was to investigate the time required to reduce iliacus muscle stiffness. Twenty-six healthy men partici- pated in this study. -

Anatomical Study on the Psoas Minor Muscle in Human Fetuses
Int. J. Morphol., 30(1):136-139, 2012. Anatomical Study on the Psoas Minor Muscle in Human Fetuses Estudio Anatómico del Músculo Psoas Menor en Fetos Humanos *Danilo Ribeiro Guerra; **Francisco Prado Reis; ***Afrânio de Andrade Bastos; ****Ciro José Brito; *****Roberto Jerônimo dos Santos Silva & *,**José Aderval Aragão GUERRA, D. R.; REIS, F. P.; BASTOS, A. A.; BRITO, C. J.; SILVA, R. J. S. & ARAGÃO, J. A. Anatomical study on the psoas minor muscle in human fetuses. Int. J. Morphol., 30(1):136-139, 2012. SUMMARY: The anatomy of the psoas minor muscle in human beings has frequently been correlated with ethnic and racial characteristics. The present study had the aim of investigating the anatomy of the psoas minor, by observing its occurrence, distal insertion points, relationship with the psoas major muscle and the relationship between its tendon and muscle portions. Twenty-two human fetuses were used (eleven of each gender), fixed in 10% formol solution that had been perfused through the umbilical artery. The psoas minor muscle was found in eight male fetuses: seven bilaterally and one unilaterally, in the right hemicorpus. Five female fetuses presented the psoas minor muscle: three bilaterally and two unilaterally, one in the right and one in the left hemicorpus. The muscle was independent, inconstant, with unilateral or bilateral presence, with distal insertions at different anatomical points, and its tendon portion was always longer than the belly of the muscle. KEY WORDS: Psoas Muscles; Muscle, Skeletal; Anatomy; Gender Identity. INTRODUCTION When the psoas minor muscle is present in humans, The aim of the present study was to investigate the it is located in the posterior wall of the abdomen, laterally to anatomy of the psoas minor muscle in human fetuses: the lumbar spine and in close contact and anteriorly to the establishing the frequency of its occurrence according to sex; belly of the psoas major muscle (Van Dyke et al., 1987; ascertaining the distal insertion points; analyzing the possible Domingo, Aguilar et al., 2004; Leão et al., 2007). -
Evaluation of Iliopsoas Strain with Findings from Diagnostic Musculoskeletal Ultrasound in Agility Performance Canines – 73 Cases
Evaluation of Iliopsoas Strain with Findings from Diagnostic Musculoskeletal Ultrasound in Agility Performance Canines – 73 Cases Robert E. Cullen DVM 1 Debra A. Canapp DVM, DACVSMR, CCRT 1* 1 Brittany J. Carr DVM 1 David L. Dycus DVM, MS, DACVSSA, CCRP 2 Victor Ibrahim MD 1 Sherman O. Canapp, Jr DVM, MS, DACVSSA, DACVSMR, CCRT 1 Veterinary Orthopedic and Sports Medicine Group, 10975 Guilford Rd, Annapolis Junction, MD 20701 2 Regenerative Orthopedics and Sports Medicine, 600 Pennsylvania Ave SE, Washington, DC 20003 * Corresponding Author ([email protected]) ISSN: 2396-9776 Published: 13 Jun 2017 in: Vol 2, Issue 2 DOI: http://dx.doi.org/10.18849/ve.v2i2.93 Reviewed by: Wanda Gordon-Evans (DVM, PhD, DACVS) and Gillian Monsell (MA, VetMB, PhD, MRCVS) ABSTRACT Objective: Iliopsoas injury and strain is a commonly diagnosed disease process, especially amongst working and sporting canines. There has been very little published literature regarding iliopsoas injuries and there is no information regarding the ultrasound evaluation of abnormal iliopsoas muscles. This manuscript is intended to describe the ultrasound findings in 73 canine agility athletes who had physical examination findings consistent with iliopsoas discomfort. The population was chosen given the high incidence of these animals for the development of iliopsoas injury; likely due to repetitive stress. Methods: Medical records of 73 agility performance canines that underwent musculoskeletal ultrasound evaluation of bilateral iliopsoas muscle groups were retrospectively reviewed. Data included signalment, previous radiographic findings, and ultrasound findings. A 3-tier grading scheme for acute strains was used while the practitioner also evaluated for evidence of chronic injury and bursitis. -

Iliopsoas Pathology, Diagnosis, and Treatment
Iliopsoas Pathology, Diagnosis, and Treatment Christian N. Anderson, MD KEYWORDS Iliopsoas Psoas Coxa saltans interna Snapping hip Iliopsoas bursitis Iliopsoas tendinitis Iliopsoas impingement KEY POINTS The iliopsoas musculotendinous unit is a powerful hip flexor used for normal lower extrem- ity function, but disorders of the iliopsoas can be a significant source of groin pain in the athletic population. Arthroscopic release of the iliopsoas tendon and treatment of coexisting intra-articular ab- normality is effective for patients with painful iliopsoas snapping or impingement that is refractory to conservative treatment. Tendon release has been described at 3 locations: in the central compartment, the periph- eral compartment, and at the lesser trochanter, with similar outcomes observed between the techniques. Releasing the tendon lengthens the musculotendinous unit, resulting in transient hip flexor weakness that typically resolves by 3 to 6 months postoperatively. INTRODUCTION The iliopsoas musculotendinous unit is a powerful hip flexor that is important for normal hip strength and function. Even so, pathologic conditions of the iliopsoas have been implicated as a significant source of anterior hip pain. Iliopsoas disorders have been shown to be the primary cause of chronic groin pain in 12% to 36% of ath- letes and are observed in 25% to 30% of athletes presenting with an acute groin injury.1–4 Described pathologic conditions include iliopsoas bursitis, tendonitis, impingement, and snapping. Acute trauma may result in injury to the musculotendi- nous unit or avulsion fracture of the lesser trochanter. Developing an understanding of the anatomy and function of the musculotendinous unit is necessary to accurately determine the diagnosis and formulate an appropriate treatment strategy for disorders of the iliopsoas. -

A Medical Case Masquerading As Surgical Pathology in an Individual Living with Diabetes
ISSN: 2377-3634 Ravindran and Obuobie. Int J Diabetes Clin Res 2019, 6:100 DOI: 10.23937/2377-3634/1410100 Volume 6 | Issue 1 International Journal of Open Access Diabetes and Clinical Research Case RepORt A Medical Case Masquerading as Surgical Pathology in an Individ- ual Living with Diabetes Ravikumar Ravindran1,* and Kofi Obuobie2 1 Specialist Registrar (ST6) in Diabetes and Endocrinology, Diabetes and Endocrinology, Royal Gwent Check for Hospital, United Kingdom updates 2Consultant in Diabetes and Endocrinology, Diabetes and Endocrinology, Royal Gwent Hospital, United Kingdom *Corresponding author: Ravikumar Ravindran, Md, MRCP, Dnb, Diploma in Endocrinology, Specialist Registrar (ST6) in Diabetes and Endocrinology, Diabetes and Endocrinology, Royal Gwent Hospital, 32 Ffordd mograif, Llanishen, Cardiff CF14 5EW, United Kingdom Abstract Introduction Diagnosing the cause of abdominal pain in a young type The Differential diagnosis of abdominal pain in a 1 diabetic can be a challenging task and involves a wide patient with Type 1 Diabetes is wide. We present a array of differential diagnosis. Most commonly the pain is medical case masquerading as surgical pathology in a thought to be secondary to diabetic neuropathy. It becomes even more problematic if there is significant weight loss, young type 1 diabetic individual. if extensive investigations have not found any organic pathology and if the pain does not fit into any pattern of Case Description diabetic neuropathy. A young 21-years-old female type 1 diabetic patient We present such a case where a young 21-years-old female had presented with significant weight loss (16 kgs over diabetic had lost 16 kgs in 6 months due to diffuse left 6 months), decreased appetite, constipation, nausea sided abdominal pain with radiation to the back. -

Psoas Muscle and Lumbar Spine Stability: a Concept Uniting Existing Controversies Critical Review and Hypothesis
Eur Spine J (2000) 9:577–585 © Springer-Verlag 2000 NEW IDEAS L. Penning Psoas muscle and lumbar spine stability: a concept uniting existing controversies Critical review and hypothesis Abstract Psoas muscle (PM) func- tate the LS, will be brought into Received: 12 February 2000 Revised: 12 May 2000 tion with regard to the lumbar spine more lordosis, with maintenance of Accepted: 22 May 2000 (LS) is disputed. Electromyographic vertical position, if a string fastened studies attribute to the PM a possible at its upper end is pulled downward role as stabilizer. Anatomical text- in a very specific direction. Con- books describe the PM as an LS versely, any increase of lordosis of flexor, but not a stabilizer. According the strip brought about by vertical to more recent anatomical studies, downward pushing of its top, will be the PM does not act on the LS, be- stabilized by tightening the pulling cause it tends to pull the LS into string in the same specific direction. more lordosis by simultaneously As this direction corresponded with flexing the lower and extending the the psoas orientation, the experi- upper region, but due to the short ments show that the PM probably moment arms of its fascicles, this functions as a stabilizer of the lor- would require maximal muscular ef- dotic LS in an upright stance by fort and would expose the LS motion adapting the state of contraction of segments to dangerous compression each of its fascicles to the momen- and shear. The findings of the pre- tary degree of lordosis imposed by sent study indicate that the described factors outside the LS, such as gen- opposite action of the PM on upper eral posture, general muscle activity L. -

Posterior Abdominal Wall- I (Muscles & Nerves)
Posterior Abdominal wall- I (Muscles & nerves) Dr Garima Sehgal Associate Professor Department of Anatomy King George’s Medical University DISCLAIMER: • The presentation includes images which are either hand drawn or have been taken from google images or books. • They are being used in the presentation only for educational purpose. • The author of the presentation claims no personal ownership over images taken from books or google images. • However, the hand drawn images are the creation of the author of the presentation Learning Objectives By the end of this teaching session you should be able to- • Describe the muscles of posterior abdominal wall (origin, insertion, actions, nerve supply) • Enumerate the nerves of the posterior abdominal wall • Describe the lumbar plexus (location , formation , branches) Understanding the anatomical reconstruction Muscles of posterior abdominal wall Skeletal Background Ligamentous background Musculofascial Background 1. T 12 vertebra th 1. Iliolumbar ligament 2. 12 rib 2. Anterior longitudnal 3. L 1 – L5 vertebrae ligament 1. Psoas major muscle 4. Iliac crest and iliac 3. Ventral sacroiliac fossa and fascia ligament 2. Quadratus lumborum 3. Iliacus and fascia iliaca 4. Psoas minor Psoas major Occupies 3 regions- abdomen, false pelvis & upper thigh Origin – 14 fleshy strips Continous attachment from T12(lower border) to L5 (upper border) 1. discs above 5 lumbar vertebrae 2. adjoining parts of vertebral bodies 3. 4 fibrous arches across the sides of upper 4 lumbar vertebrae Actions – i. Chief flexor of -

Unilateral Variant Psoas Major with Split Femoral Nerve
S Journal of O p s e s n Acce Anatomy and Physiological Studies CASE REPORT Unilateral Variant Psoas Major with Split Femoral Nerve Tiraj Parikh*1, Caleb Parry1, Marina Motina1, Shahana Momin1, Rebecca Mickle1, Peter Nguyen1, Aaron Perez1, Cara Fisher PhD2 1Texas College of Osteopathic Medicine 2Center for Anatomical Sciences, University of North Texas Health Science Center Introduction [4]. Psoas tertius is described as a slip of muscle originating from the inner half of the 12th rib and transverse processes of The psoas major muscle includes slips of muscle that originate lumbar vertebrae 1-4 and attaching to the iliopsoas muscle [5]. from the transverse processes of lumbar vertebrae 1-5 and Another study describes their findings of an accessory psoas intervertebral discs of T12-L4. These slips of muscle combine major muscle originating on the left costal process of L3 and and join with the iliacus muscle to then course inferiorly and the intertransverse ligament between L3 and L4 [6]. Although insert onto the lesser trochanter of the femur [1].The psoas rare, these variants have also been shown to split the femoral muscle is considered one of the primary flexors of the hip nerve. It has been proposed that this occurrence is associated joint and is innervated by the femoral nerve, which arises with neuropathies. [5-9]. from ventral rami of lumbar spinal nerves 2-4. The femoral nerve then passes through the psoas major in an inferolateral Case Presentation direction until it emerges on the lateral border of the muscle Here we present a novel variant of the psoas major muscle. -

Previously Unreported Variation in the Innervation of the Psoas Major
ogy: iol Cu ys r h re P n t & R y e s Anatomy & Physiology: Current m e o a t r a c n h Voin et al., Anat Physiol 2017, 7:S6 A Research ISSN: 2161-0940 DOI: 10.4172/2161-0940.S6-003 Case Report Open Access Previously Unreported Variation in the Innervation of the Psoas Major Muscle Voin V1*, Topale N2, Schmidt C1, Iwanaga J1 and Tubbs RS1 1Seattle Science Foundation, Seattle, WA, USA 2St George’s University, St. George’s, Grenada *Corresponding author: Voin V, Seattle Science Foundation, Seattle, WA, USA, Tel: +1-206-334-8399; E-mail: [email protected] Received Date: February 15, 2017; Accepted Date: February 20, 2017; Published Date: February 28, 2017 Copyright: © 2017 Voin V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Injury to the nerves of the lumbar plexus can result in significant disability. Therefore, the clinician should be knowledgeable of both the normal and variant anatomy of these branches. We report what we believe to be the first description of the accessory obturator nerve providing a branch to the psoas major muscle. Such a variant innervation to the psoas major muscle should be kept in mind by those who examine patients or operate near the lumbar plexus. Keywords: Posterior Abdominal Wall; Lumbar Plexus; Variation and Anatomy Introduction The psoas major is a large, long muscle that lies on either side of the lumbar vertebral column [1]. -
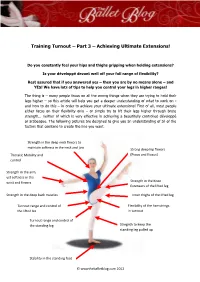
Training Turnout – Part 3 – Achieving Ultimate Extensions!
Training Turnout – Part 3 – Achieving Ultimate Extensions! Training Turnout – Part 3 – Achieving Ultimate Extensions! Do you constantly feel your hips and thighs gripping when holding extensions? Is your développé devant well off your full range of flexibility? Rest assured that if you answered yes – then you are by no means alone – and YES! We have lots of tips to help you control your legs in higher ranges! The thing is – many people focus on all the wrong things when they are trying to hold their legs higher – so this article will help you get a deeper understanding of what to work on - and how to do this – in order to achieve your ultimate extensions! First of all, most people either focus on their flexibility only – or simply try to lift their legs higher through brute strength… neither of which is very effective in achieving a beautifully controlled développé or arabesque. The following pictures are designed to give you an understanding of all of the factors that combine to create the line you want. Strength in the deep neck flexors to maintain softness in the neck and jaw Strong deep hip flexors Thoracic Mobility and (Psoas and Iliacus) control Strength in the arm, yet softness in the wrist and fingers Strength in the Knee Extensors of the lifted leg Strength in the deep back muscles Inner thighs of the lifted leg Turnout range and control of Flexibility of the hamstrings the lifted leg in turnout Turnout range and control of the standing leg Stregnth to keep the standing leg pulled up Stability in the standing foot © wwwtheballetblog.com 2012 Training Turnout – Part 3 – Achieving Ultimate Extensions! Now that is a lot to take in all at once! Which is why this is part three of a three part series! Please make sure that you have read the first two PDFs before you start on the exercises in this section. -
Hip Adduction
BONES AND JOINTS OF THE LOWER LIMBS Yasser Moh. Aneis, PhD, MSc., PT. Lecturer of Physical Therapy Basic Sciences Department BONES AND JOINTS OF THE LOWER LIMBS The Pelvis The top portion of the femur with its head in the acetabulum Bones of the right thigh, anterior and posterior view Bones of the lower leg Bones of the foot PELVIC ELEVATION (Hip Hiking) oThe Primary muscle •Quadratus Lumborum Origin: -Iliac crest. -Iliolumber ligament. Insertion: -Inferior border of 12th rib. -Apices of transverse processes of L1- 4. - Iliolumber ligament. Nerve supply: -Anterior primary rami (T12, L1, L2, L3) Range of Motion: -In standing position pelvis may be raised on one side until foot is well clear of floor. Action: -Elevates the pelvis laterally by producing a lateral flexion of the lumber spine. -Depress the last rib and fixes the last two ribs during forced expiration. Action of Quadratus Lumborum Muscle •Factors Limiting Motion: -Tension of spinal ligaments on opposite side. -Contact of iliac crest with thorax. Testing procedure oGrades 4-5. "Good and Normal strength" -Back lying with lumbar area of spine in moderate extension. -Patient grasps edge of table to stabilize thorax. -Therapist stands at the foot of the table, both hands grasping the lower limb above or proximal to the ankle joint. •Command: -Pull up your pelvis toward the thorax on one side ----Relax. •Resistance: -resistance is given in a form of traction on the extremity directly opposing the line of pull. oGrade 3 and Grade 2 (Fair and Poor Strength) -Patient starting position :Same as for Grade 4&5. -
Anatomy of the Posterior Approach to the Lumbar Plexus Block
480 Anatomy of the posterior approach to the lumbar plexus Juliana Farny MD,* Pierre Dmlet mD FRCPC,~ block Michel Girard MD MHPE FRCPC~ The purpose of this study was to describe the relation of the qu'entre celui-ci et le carrd des lombes. Le nerf fdmoral est lumbar plexus with the psoas major and with the superficial situd entre les nerfs fdmoro-cutand latdral et obturateur. Ce- and deep landmarks close to it. Four cadavers were dissected pendant, alors que le nerf fdmoro-cutand latdral est dans le and 22 computed tomography files of the lumbosacral region m~me plan que le nerf fkmoral, le nerf obturateur peut les studied. Cadaver dissections demonstrated that the lumbar y accompagner ou se retrouver dans un repli du muscle psoas plexus, at the level of L 5, is within the substance of the psoas quile sdpare des deux autres nerfs. Ins dtudes radiologiques major muscle rather than between this muscle and the quad- ont fourni les donndes suivantes: le neorfdmoral est it une pro- ratus lumborum. The femoral nerve lies between the lateral fondeur de 9,01 + 2,43 cm; le bord interne du psoas est it femoral cutaneous and obturator nerves. However, while the 2, 73 + 0,64 cm du plan sagital mddian; alors que le bord externe lateral femoral cutaneous nerve is in the same fascial plane de ce muscle est it 6,41 + 1,61 cm de ce m~me plan. Nous as the femoral nerve, the obturator nerve can be found in the concluons que le plexus lombaire est clans le muscle psoas, same plane as the two other nerves or in its own muscular que la position du neff obturateur varie par rapport au neff fold.