Snakebite Treatment Protocol Swaziland Antivenom Foundation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Freshwater Fishes
WESTERN CAPE PROVINCE state oF BIODIVERSITY 2007 TABLE OF CONTENTS Chapter 1 Introduction 2 Chapter 2 Methods 17 Chapter 3 Freshwater fishes 18 Chapter 4 Amphibians 36 Chapter 5 Reptiles 55 Chapter 6 Mammals 75 Chapter 7 Avifauna 89 Chapter 8 Flora & Vegetation 112 Chapter 9 Land and Protected Areas 139 Chapter 10 Status of River Health 159 Cover page photographs by Andrew Turner (CapeNature), Roger Bills (SAIAB) & Wicus Leeuwner. ISBN 978-0-620-39289-1 SCIENTIFIC SERVICES 2 Western Cape Province State of Biodiversity 2007 CHAPTER 1 INTRODUCTION Andrew Turner [email protected] 1 “We live at a historic moment, a time in which the world’s biological diversity is being rapidly destroyed. The present geological period has more species than any other, yet the current rate of extinction of species is greater now than at any time in the past. Ecosystems and communities are being degraded and destroyed, and species are being driven to extinction. The species that persist are losing genetic variation as the number of individuals in populations shrinks, unique populations and subspecies are destroyed, and remaining populations become increasingly isolated from one another. The cause of this loss of biological diversity at all levels is the range of human activity that alters and destroys natural habitats to suit human needs.” (Primack, 2002). CapeNature launched its State of Biodiversity Programme (SoBP) to assess and monitor the state of biodiversity in the Western Cape in 1999. This programme delivered its first report in 2002 and these reports are updated every five years. The current report (2007) reports on the changes to the state of vertebrate biodiversity and land under conservation usage. -

Notes on the Distribution and Natural History of the King Cobra (Ophiophagus Hannah Cantor, 1836) from the Kumaon Hills of Uttarakhand, India
Herpetology Notes, volume 11: 217-222 (2018) (published online on 12 March 2018) Notes on the distribution and natural history of the King Cobra (Ophiophagus hannah Cantor, 1836) from the Kumaon Hills of Uttarakhand, India Jignasu Dolia1 Introduction herpetologists believe that the King Cobra may be part of a larger species complex (Das, 2002). However, Native to South and Southeast Asia, the King Cobra further phylogenetic studies based on molecular data (Ophiophagus hannah Cantor, 1836) is the world’s between the different populations are needed to shed longest venomous snake, capable of growing up to 5.49– light on its true taxonomy. 5.79 m (Aagard, 1924; Mehrtens, 1987; Daniel, 2002). The King Cobra’s known altitudinal distribution Its established global distribution includes the following ranges from 150 m to 1530 m in Nepal (Schleich and 15 countries: Bangladesh, Bhutan, Brunei Darussalam, Kästle, 2002) and from sea level to 1800 m in Sumatra Cambodia, China (mainland as well as Hong Kong (David and Vogel, 1996). In India, the species has been Special Administrative Region), India, Indonesia, Lao sighted at 1840 m in Sikkim (Bashir et al., 2010), and People’s Democratic Republic, Malaysia, Myanmar, King Cobra nests have been found between 161 m and Nepal, Philippines, Singapore, Thailand and Vietnam 1170 m in Mizoram (Hrima et al., 2014). The King (Stuart et al., 2012). Although widely distributed, this Cobra has also been recorded up to c. 1830 m in the snake is considered rare in most parts of its range, Nilgiris and in the Western Himalayas (Smith, 1943). except in forested parts of Thailand where it is relatively The highest altitude recorded and published for an common (Stuart et al., 2012). -

(Equatorial Spitting Cobra) Venom a P
The Journal of Venomous Animals and Toxins including Tropical Diseases ISSN 1678-9199 | 2011 | volume 17 | issue 4 | pages 451-459 Biochemical and toxinological characterization of Naja sumatrana ER P (Equatorial spitting cobra) venom A P Yap MKK (1), Tan NH (1), Fung SY (1) RIGINAL O (1) Department of Molecular Medicine, Center for Natural Products and Drug Research (CENAR), Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia. Abstract: The lethal and enzymatic activities of venom from Naja sumatrana (Equatorial spitting cobra) were determined and compared to venoms from three other Southeast Asian cobras (Naja sputatrix, Naja siamensis and Naja kaouthia). All four venoms exhibited the common characteristic enzymatic activities of Asiatic cobra venoms: low protease, phosphodiesterase, alkaline phosphomonoesterase and L-amino acid oxidase activities, moderately high acetylcholinesterase and hyaluronidase activities and high phospholipase A2. Fractionation of N. sumatrana venom by Resource® S cation exchange chromatography (GE Healthcare, USA) yielded nine major protein peaks, with all except the acidic protein peak being lethal to mice. Most of the protein peaks exhibit enzymatic activities, and L-amino acid oxidase, alkaline phosphomonoesterase, acetylcholinesterase, 5’-nucleotidase and hyaluronidase exist in multiple forms. Comparison of the Resource® S chromatograms of the four cobra venoms clearly indicates that the protein composition of N. sumatrana venom is distinct from venoms of the other two spitting cobras, N. sputatrix (Javan spitting cobra) and N. siamensis (Indochinese spitting cobra). The results support the revised systematics of the Asiatic cobra based on multivariate analysis of morphological characters. The three spitting cobra venoms exhibit two common features: the presence of basic, potentially pharmacologically active phospholipases A2 and a high content of polypeptide cardiotoxin, suggesting that the pathophysiological actions of the three spitting cobra venoms may be similar. -

Addo Elephant National Park Reptiles Species List
Addo Elephant National Park Reptiles Species List Common Name Scientific Name Status Snakes Cape cobra Naja nivea Puffadder Bitis arietans Albany adder Bitis albanica very rare Night adder Causes rhombeatus Bergadder Bitis atropos Horned adder Bitis cornuta Boomslang Dispholidus typus Rinkhals Hemachatus hemachatus Herald/Red-lipped snake Crotaphopeltis hotamboeia Olive house snake Lamprophis inornatus Night snake Lamprophis aurora Brown house snake Lamprophis fuliginosus fuliginosus Speckled house snake Homoroselaps lacteus Wolf snake Lycophidion capense Spotted harlequin snake Philothamnus semivariegatus Speckled bush snake Bitis atropos Green water snake Philothamnus hoplogaster Natal green watersnake Philothamnus natalensis occidentalis Shovel-nosed snake Prosymna sundevalli Mole snake Pseudapsis cana Slugeater Duberria lutrix lutrix Common eggeater Dasypeltis scabra scabra Dappled sandsnake Psammophis notosticus Crossmarked sandsnake Psammophis crucifer Black-bellied watersnake Lycodonomorphus laevissimus Common/Red-bellied watersnake Lycodonomorphus rufulus Tortoises/terrapins Angulate tortoise Chersina angulata Leopard tortoise Geochelone pardalis Green parrot-beaked tortoise Homopus areolatus Marsh/Helmeted terrapin Pelomedusa subrufa Tent tortoise Psammobates tentorius Lizards/geckoes/skinks Rock Monitor Lizard/Leguaan Varanus niloticus niloticus Water Monitor Lizard/Leguaan Varanus exanthematicus albigularis Tasman's Girdled Lizard Cordylus tasmani Cape Girdled Lizard Cordylus cordylus Southern Rock Agama Agama atra Burrowing -

Cobra Risk Assessment
Invasive animal risk assessment Biosecurity Queensland Agriculture Fisheries and Department of Cobra (all species) Steve Csurhes and Paul Fisher First published 2010 Updated 2016 Pest animal risk assessment © State of Queensland, 2016. The Queensland Government supports and encourages the dissemination and exchange of its information. The copyright in this publication is licensed under a Creative Commons Attribution 3.0 Australia (CC BY) licence. You must keep intact the copyright notice and attribute the State of Queensland as the source of the publication. Note: Some content in this publication may have different licence terms as indicated. For more information on this licence visit http://creativecommons.org/licenses/ by/3.0/au/deed.en" http://creativecommons.org/licenses/by/3.0/au/deed.en Photo: Image from Wikimedia Commons (this image is reproduced under the terms of a GNU Free Documentation License) Invasive animal risk assessment: Cobra 2 Contents Summary 4 Introduction 5 Identity and taxonomy 5 Taxonomy 3 Description 5 Diet 5 Reproduction 6 Predators and diseases 6 Origin and distribution 7 Status in Australia and Queensland 8 Preferred habitat 9 History as a pest elsewhere 9 Uses 9 Pest potential in Queensland 10 Climate match 10 Habitat suitability 10 Broad natural geographic range 11 Generalist diet 11 Venom production 11 Disease 11 Numerical risk analysis 11 References 12 Attachment 1 13 Invasive animal risk assessment: Cobra 3 Summary The common name ‘cobra’ applies to 30 species in 7 genera within the family Elapidae, all of which can produce a hood when threatened. All cobra species are venomous. As a group, cobras have an extensive distribution over large parts of Africa, Asia, Malaysia and Indonesia. -
Lesotho Fourth National Report on Implementation of Convention on Biological Diversity
Lesotho Fourth National Report On Implementation of Convention on Biological Diversity December 2009 LIST OF ABBREVIATIONS AND ACRONYMS ADB African Development Bank CBD Convention on Biological Diversity CCF Community Conservation Forum CITES Convention on International Trade in Endangered Species CMBSL Conserving Mountain Biodiversity in Southern Lesotho COP Conference of Parties CPA Cattle Post Areas DANCED Danish Cooperation for Environment and Development DDT Di-nitro Di-phenyl Trichloroethane EA Environmental Assessment EIA Environmental Impact Assessment EMP Environmental Management Plan ERMA Environmental Resources Management Area EMPR Environmental Management for Poverty Reduction EPAP Environmental Policy and Action Plan EU Environmental Unit (s) GA Grazing Associations GCM Global Circulation Model GEF Global Environment Facility GMO Genetically Modified Organism (s) HIV/AIDS Human Immuno Virus/Acquired Immuno-Deficiency Syndrome HNRRIEP Highlands Natural Resources and Rural Income Enhancement Project IGP Income Generation Project (s) IUCN International Union for Conservation of Nature and Natural Resources LHDA Lesotho Highlands Development Authority LMO Living Modified Organism (s) Masl Meters above sea level MDTP Maloti-Drakensberg Transfrontier Conservation and Development Project MEAs Multi-lateral Environmental Agreements MOU Memorandum Of Understanding MRA Managed Resource Area NAP National Action Plan NBF National Biosafety Framework NBSAP National Biodiversity Strategy and Action Plan NEAP National Environmental Action -

The Herpetofauna of the Cubango, Cuito, and Lower Cuando River Catchments of South-Eastern Angola
Official journal website: Amphibian & Reptile Conservation amphibian-reptile-conservation.org 10(2) [Special Section]: 6–36 (e126). The herpetofauna of the Cubango, Cuito, and lower Cuando river catchments of south-eastern Angola 1,2,*Werner Conradie, 2Roger Bills, and 1,3William R. Branch 1Port Elizabeth Museum (Bayworld), P.O. Box 13147, Humewood 6013, SOUTH AFRICA 2South African Institute for Aquatic Bio- diversity, P/Bag 1015, Grahamstown 6140, SOUTH AFRICA 3Research Associate, Department of Zoology, P O Box 77000, Nelson Mandela Metropolitan University, Port Elizabeth 6031, SOUTH AFRICA Abstract.—Angola’s herpetofauna has been neglected for many years, but recent surveys have revealed unknown diversity and a consequent increase in the number of species recorded for the country. Most historical Angola surveys focused on the north-eastern and south-western parts of the country, with the south-east, now comprising the Kuando-Kubango Province, neglected. To address this gap a series of rapid biodiversity surveys of the upper Cubango-Okavango basin were conducted from 2012‒2015. This report presents the results of these surveys, together with a herpetological checklist of current and historical records for the Angolan drainage of the Cubango, Cuito, and Cuando Rivers. In summary 111 species are known from the region, comprising 38 snakes, 32 lizards, five chelonians, a single crocodile and 34 amphibians. The Cubango is the most western catchment and has the greatest herpetofaunal diversity (54 species). This is a reflection of both its easier access, and thus greatest number of historical records, and also the greater habitat and topographical diversity associated with the rocky headwaters. -

Evidence for Range Maintenance and Homing in a New World Elapid, The
bioRxiv preprint doi: https://doi.org/10.1101/092833; this version posted December 9, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Evidence for Philopatry and Homing in a New World Elapid Snake Alexander S. Hall1, Abigail M. K. Vázquez-Quinto2, Antonio Ramírez-Velázquez2, Eric N. Smith1 1 Department of Biology, The University of Texas at Arlington, Arlington, TX 76019, USA. E- mail: [email protected], [email protected] 2 Zoológico Regional Miguel Álvarez del Toro, Calzada Cerro Hueco, Col Zapotal, C. P. 29094, Tuxtla Gutiérrez, Chiapas, México. E-mail: [email protected], [email protected] Short running title: Homing elapid bioRxiv preprint doi: https://doi.org/10.1101/092833; this version posted December 9, 2016. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Homing elapid 2 Abstract Animal navigation allows individuals to efficiently find and use best available habitats. Despite the long history of research into well-studied taxa (e.g., pigeons, salmon, sea turtles), we know relatively little about squamate navigational abilities. Among snakes, documented philopatry (range maintenance) in a non-colubrid species has been rare. In this study, we document the first example of philopatry and homing in a new world elapid snake, Micrurus apiatus. -

A Homoeopathic Drug Proving of Hemachatus Haemachatus with A
A homoeopathic drug proving of Hemachatus haemachatus with a subsequent comparison of this remedy to those remedies yielding the highest numerical value and total number of rubrics on repertorisation of the proving symptoms. By Jodi Cahill Mini-dissertation submitted in partial compliance with the requirements of the Master‟s Degree in Technology: Homoeopathy in the Faculty of Health Sciences at the Durban University of Technology I, Jodi Cahill do declare that this mini-dissertation is representative of my own work, both in conception and execution. _____________________ ____________________ Signature of Student Date of signature APPROVED FOR FINAL SUBMISSION _____________________ _____________________ Signature of Supervisor Date of signature Dr. Madhu Maharaj M. Tech: Hom. (T.N) _____________________ _____________________ Signature of Co- Supervisor Date of signature Dr. Ashley Ross M. Tech: Hom. (T.N), B. Mus (UCT) 1 To Niko My greatest fan. 2 Acknowledgements Dr Madhu Maharaj Thank you for your light and guidance. You have so humbly taught me to acknowledge the value in remaining a scholar of homoeopathy, and a scholar of life. It has been an honour to have been guided by you and I will forever hold your insight in high regard. Dr Ashley Ross Your deep understanding and passion for homoeopathy inspires me. I have been truly blessed by having such great teachers who are so open to sharing their knowledge. I can only pray that I may cross paths with such great teachers in my journeys to come. Thank you! My Parents Thank you for supporting me through my journey so far. It has been a tough one at times but we have grown together. -
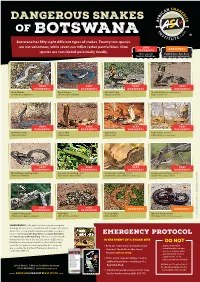
Botswana Has Fifty Eight Different Types of Snakes
DANGEROUS SNAKES OF B OT SWA NA Botswana has fifty eight different types of snakes. Twenty two species are not venomous, while seven can inflict rather painful bites. Nine VERY DANGEROUS species are considered potentially deadly. DANGEROUS Has caused Painful bite, but does human fatalities not require antivenom VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Black Mamba Black Mamba Snouted Cobra Snouted Cobra - banded phase (Dendroaspis polylepis) (Dendroaspis polylepis) (Naja annulifera) (Naja annulifera) VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Anchieta’s Cobra Cape Cobra Cape Cobra Cape Cobra - juvenile (Naja anchietae) (Naja nivea) (Naja nivea) (Naja nivea) Photo Marius Burger VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Mozambique Spitting Cobra Common Boomslang - male Common Boomslang - female Common Boomslang - juvenile (Naja mossambica) (Dispholidus typus viridis) (Dispholidus typus viridis) Photo André Coetzer (Dispholidus typus viridis) VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Southern Twig Snake Puff Adder Horned Adder Bibron’s Stiletto Snake (Thelotornis capensis capensis) (Bitis arietans arietans) (Bitis caudalis) (Atractaspis bibronii) Photo Warren Dick © Johan Marais African Snakebite Institute Snakebite African © Johan Marais JOHAN MARAIS is the author of various books on reptiles including the best-seller A Complete Guide to Snakes of Southern Africa. He is a popular public speaker and offers a variety of courses including Snake Awareness, Scorpion Awareness EMERGENCY PROTOCOL and Venomous Snake Handling. Johan is accredited by the International Society of Zoological Sciences (ISZS) and is a IN THE EVENT OF A SNAKE BITE Field Guides Association of Southern Africa (FGASA) and DO NOT ww Travel Doctor-approved service provider. His courses are 1 Keep the victim calm, immobilized and .. -

Os Répteis De Angola: História, Diversidade, Endemismo E Hotspots
CAPÍTULO 13 OS RÉPTEIS DE ANGOLA: HISTÓRIA, DIVERSIDADE, ENDEMISMO E HOTSPOTS William R. Branch1,2, Pedro Vaz Pinto3,4, Ninda Baptista1,4,5 e Werner Conradie1,6,7 Resumo O estado actual do conhecimento sobre a diversidade dos répteis de Angola é aqui tratada no contexto da história da investigação herpe‑ tológica no país. A diversidade de répteis é comparada com a diversidade conhecida em regiões adjacentes de modo a permitir esclarecer questões taxonómicas e padrões biogeográficos. No final do século xix, mais de 67% dos répteis angolanos encontravam‑se descritos. Os estudos estag‑ naram durante o século seguinte, mas aumentaram na última década. Actualmente, são conhecidos pelo menos 278 répteis, mas foram feitas numerosas novas descobertas durante levantamentos recentes e muitas espécies novas aguardam descrição. Embora a diversidade dos lagartos e das cobras seja praticamente idêntica, a maioria das novas descobertas verifica‑se nos lagartos, particularmente nas osgas e lacertídeos. Destacam‑ ‑se aqui os répteis angolanos mal conhecidos e outros de regiões adjacentes que possam ocorrer no país. A maioria dos répteis endémicos angolanos é constituída por lagartos e encontra ‑se associada à escarpa e à região árida do Sudoeste. Está em curso a identificação de hotspots de diversidade de 1 National Geographic Okavango Wilderness Project, Wild Bird Trust, South Africa 2 Research Associate, Department of Zoology, P.O. Box 77000, Nelson Mandela University, Port Elizabeth 6031, South Africa 3 Fundação Kissama, Rua 60, Casa 560, Lar do Patriota, Luanda, Angola 4 CIBIO ‑InBIO, Centro de Investigação em Biodiversidade e Recursos Genéticos, Laboratório Associado, Campus de Vairão, Universidade do Porto, 4485 ‑661 Vairão, Portugal 5 ISCED, Instituto Superior de Ciências da Educação da Huíla, Rua Sarmento Rodrigues s/n, Lubango, Angola 6 School of Natural Resource Management, George Campus, Nelson Mandela University, George 6530, South Africa 7 Port Elizabeth Museum (Bayworld), P.O. -

Ancestral Reconstruction of Diet and Fang Condition in the Lamprophiidae: Implications for the Evolution of Venom Systems in Snakes
Journal of Herpetology, Vol. 55, No. 1, 1–10, 2021 Copyright 2021 Society for the Study of Amphibians and Reptiles Ancestral Reconstruction of Diet and Fang Condition in the Lamprophiidae: Implications for the Evolution of Venom Systems in Snakes 1,2 1 1 HIRAL NAIK, MIMMIE M. KGADITSE, AND GRAHAM J. ALEXANDER 1School of Animal, Plant and Environmental Sciences, University of the Witwatersrand, Johannesburg. PO Wits, 2050, Gauteng, South Africa ABSTRACT.—The Colubroidea includes all venomous and some nonvenomous snakes, many of which have extraordinary dental morphology and functional capabilities. It has been proposed that the ancestral condition of the Colubroidea is venomous with tubular fangs. The venom system includes the production of venomous secretions by labial glands in the mouth and usually includes fangs for effective delivery of venom. Despite significant research on the evolution of the venom system in snakes, limited research exists on the driving forces for different fang and dental morphology at a broader phylogenetic scale. We assessed the patterns of fang and dental condition in the Lamprophiidae, a speciose family of advanced snakes within the Colubroidea, and we related fang and dental condition to diet. The Lamprophiidae is the only snake family that includes front-fanged, rear-fanged, and fangless species. We produced an ancestral reconstruction for the family and investigated the pattern of diet and fangs within the clade. We concluded that the ancestral lamprophiid was most likely rear-fanged and that the shift in dental morphology was associated with changes in diet. This pattern indicates that fang loss, and probably venom loss, has occurred multiple times within the Lamprophiidae.