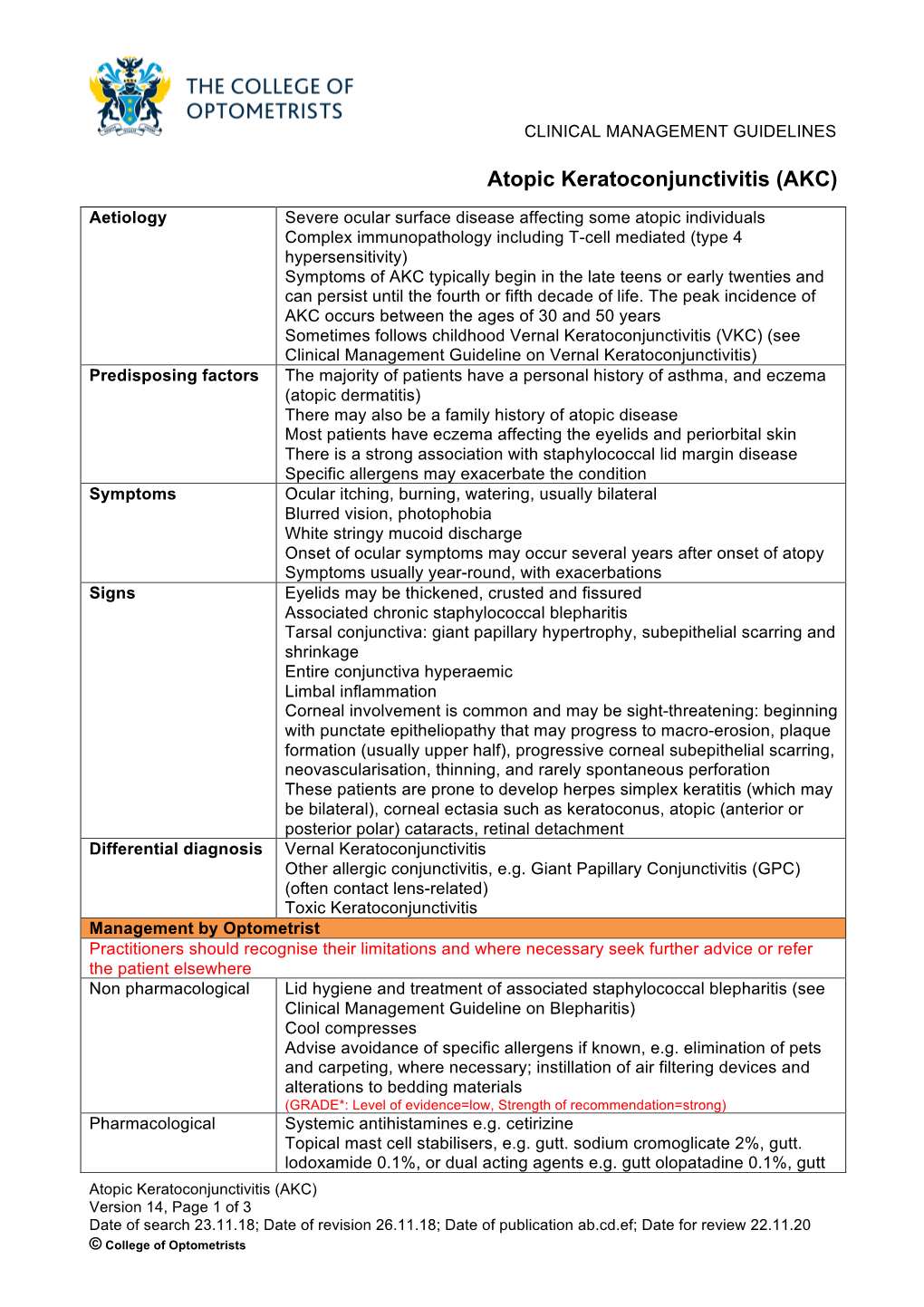
Atopic Keratoconjunctivitis (AKC)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ocular Injury; Hazard to Society: a Case Series
Quest Journals Journal of Medical and Dental Science Research Volume 7~ Issue 8 (2020) pp: 34-44 ISSN(Online) : 2394-076X ISSN (Print):2394-0751 www.questjournals.org Research Paper Ocular Injury; Hazard to Society: A Case Series Dr Rashmi kujur1, Dr Pallavi. M.P2, Dr Harshita Dubey3, Dr Varsha4 1Dept. of ophthalmology, Madhav dispensary JAH, GRMC, Gwalior, Madhyapradesh. 2Senior girls hostel, GRMC, Gwalior, Madhyapradesh. 3Senior girls hostel, GRMC, Gwalior, Madhyapradesh. 4Senior girls hostel, GRMC, Gwalior,Madhyapradesh. Corresponding Author: Dr.Pallavi.M.P ABSTRACT Purpose: To describe various types of ocular trauma due to different modes of injuryoccured on the same day Design: Prospective interventional study (case series) Materials & Methods: A series of cases of ocular trauma in different age group on the same day. Results: Five patients of ocular trauma were studied & managed. All five patients were males. Out of 5 cases, 3 cases had open globe injury and 2 cases had closed globe injury. Three out of five patients required surgical intervention while 2 patients were managed with medical therapy. Conclusion: This study describes the types and characteristics of ocular trauma presenting in eye department. The frequency of ocular trauma is common in males. Eye injuries resulting from ocular trauma pose a frequent threat to vision the world over. While afocussed history and prompt ocular examination are essential to immediate management, patient educationregarding safety precautions and risk reduction help to prevent future recurrences. KEYWORDS: Ocular morbidity, Ocular Injury, globe rupture, iridodialysis, fire cracker injury, hyphema, Road Traffic accident (RTA), loss of vision. Received 05 December, 2020; Accepted 20 December, 2020 © The author(s) 2020. -

Therapeutic and Inducing Effect of Corneal Crosslinking on Infectious
Differenteffectsofcornealcrosslinkingoninfectiouskeratitis 窑Review窑 Therapeuticandinducingeffectofcornealcrosslinking oninfectiouskeratitis 1DepartmentofOphthalmology,ShandongProvincial thecornealintrinsicbiomechanicalpropertyandthestiffness HospitalAffiliatedtoShandongUniversity,Jinan250000, ofcorneatoresistectasiaofcornea [1].Besidesitsoriginal ShandongProvince,China applicationforthekeratoconusandkeratectasia [2],CXLhas 2DepartmentofOphthalmology,thePeople'sHospitalof beenutilizedontothetreatmentofinfectiouskeratitis [3], Linyi,Linyi276000,ShandongProvince,China nowadays.Althoughthesecondaryinfectiouskeratitisafter 3DepartmentofPediatrics,thePeople'sHospitalofLinyi, CXLisrare,therearesomereportsonsecondarykeratitis Linyi276000,ShandongProvince,China infectedby bacteria,fungi,herpessimplexvirusand Co-firstauthors: Liang-ZhuJiangandShi-YanQiu Acanthamoeba.ThisrarecomplicationofCXLcancause Correspondence to: Guo-YingMu.Departmentof seriousocularmorbidityandhaveasubsequentdamaging Ophthalmology,ShandongProvincialHospitalAffiliatedto effectonthepatient'svision.ThesurgicaltechniqueofCXL ShandongUniversity,Jinan250000,ShandongProvince, involvestheremovalofepitheliumintraoperativelyandthe [email protected] applicationofcontactlenspostoperatively.Thesefactors Received:2015-06-30Accepted:2016-08-09 havebeenassociatedwiththeoccurrenceofinfectious keratitisafterCXL.Inpresentstudy,wesummarizedthe Abstract therapeuticeffectofCXLoninfectiouskeratitisandthe · Thecornealcrosslinking (CXL)withriboflavinand keratitissecondarytocorneaCXLreportedbyprevious -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Ocular Photography - External (L34393)
Local Coverage Determination (LCD): Ocular Photography - External (L34393) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information Contractor Name Contract Type Contract Number Jurisdiction State(s) CGS Administrators, LLC MAC - Part A 15101 - MAC A J - 15 Kentucky CGS Administrators, LLC MAC - Part B 15102 - MAC B J - 15 Kentucky CGS Administrators, LLC MAC - Part A 15201 - MAC A J - 15 Ohio CGS Administrators, LLC MAC - Part B 15202 - MAC B J - 15 Ohio Back to Top LCD Information Document Information LCD ID Original Effective Date L34393 For services performed on or after 10/01/2015 Original ICD-9 LCD ID Revision Effective Date L31880 For services performed on or after 10/01/2018 Revision Ending Date LCD Title N/A Ocular Photography - External Retirement Date Proposed LCD in Comment Period N/A N/A Notice Period Start Date Source Proposed LCD N/A N/A Notice Period End Date AMA CPT / ADA CDT / AHA NUBC Copyright Statement N/A CPT only copyright 2002-2018 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association. Applicable FARS/DFARS Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein. The Code on Dental Procedures and Nomenclature (Code) is published in Current Dental Terminology (CDT). -

Keratoconjunctivitis Sicca (“Dry Eye”) Stephanie Shrader, DVM and John Robertson, VMD, Phd
Keratoconjunctivitis sicca (“Dry Eye”) Stephanie Shrader, DVM and John Robertson, VMD, PhD Introduction and Overview How Tears Are Produced Keratoconjunctivitis sicca (KCS) is a disease of the eyes, The tear film that covers the eyes is made up of three distinct characterized by inflammation of the cornea and conjunctiva. layers. The outermost layer is made up of oils, which are This condition occurs secondary to a deficiency in formation secreted by the Meibomian glands. This lipid layer provides of the tear film that normally protects the cornea (Best et al, protection against evaporation, binds the tear film to the 2014), which leads to dry, irritated eyes. As a result, KCS is cornea, and prevents tears from simply pouring out over the commonly known as “dry eye” or in veterinary terminology, lower eyelid onto the face. The middle layer of the tear film is xerophthalmia. This disease occurs often in West Highland the aqueous layer, which is produced by the lacrimal glands. As White Terriers, but is also common in many other breeds, its name would suggest, the aqueous layer consists primarily including Lhasa Apso, English Bulldog, American Cocker of water, along with important proteins and enzymes that help Spaniel, English Springer Spaniel, Pekingese, Pug, Chinese Shar remove bacteria and cellular waste material, and lubricate the Pei, Yorkshire Terrier, Shih Tzu, Miniature Schnauzer, German surface of the cornea. The innermost layer of the tear film is the Shepherd, Doberman Pinscher, and Boston Terrier. While the mucin layer, which is is produced by tiny secretory cells in the reported incidence of KCS across all dog breeds ranges from conjunctiva known as goblet cells. -
Update on Pathologic Diagnosis of Corneal Infections and Inflammations
[Downloaded free from http://www.meajo.org on Tuesday, March 27, 2012, IP: 41.234.93.234] || Click here to download free Android application for this journal Eye Pathology Update Update on Pathologic Diagnosis of Corneal Infections and Inflammations Geeta K. Vemuganti, Somasheila I. Murthy1, Sujata Das2 ABSTRACT Access this article online Website: One of the most frequent types of corneal specimen that we received in our pathology laboratory www.meajo.org is an excised corneal tissue following keratoplasty. Several of these cases are due to corneal DOI: infections or the sequelae, like corneal scar. Advances in the histological and molecular 10.4103/0974-9233.90128 diagnosis of corneal infections and inflammations have resulted in rapid and accurate diagnosis Quick Response Code: of the infectious agent and in the overall understanding of the mechanisms in inflammatory diseases of the cornea. This review provides an update of histopathological findings in various corneal infections and inflammations. Key words: Corneal Histopathology, Corneal Infiltrate, Corneal Inflammations, Microbial Keratitis, Moorens’ Ulcer INTRODUCTION Corneal infections often commence as epithelial ulceration followed by stromal infiltration by polymorphonuclear (PMN) eratitis is an important cause of ocular morbidity worldwide, and lymphomononuclear cells leading to destruction of Bowman’s Kthe outcome of which depends on early diagnosis, prompt layer, stromal necrosis and perforation of the Descemet’s 1 and effective treatment and various host and agent factors. Some membrane in severe cases. Suppurative infections like bacterial of the common causes of infectious keratitis include bacterial, and fungal lead to infiltrates in anterior 2/3 of stroma and abscess fungal, viral, and protozoan, the diagnosis of which is made on formation. -
Reactive Arthritis This Sheet Has Been Written for People Affected by Reactive Arthritis
ARTHRIINFORMATIONTI SHEETS ARTHRIINFORMATIONTI SHEETS Reactive arthritis This sheet has been written for people affected by reactive arthritis. It provides general information to help you understand how you may be affected. This sheet also covers how reactive arthritis usually resolves over time. What is reactive arthritis? It is not known why some people who get these Reactive arthritis is a condition that causes infections develop reactive arthritis and some do not. inflammation, pain and swelling of the joints. It usually A certain gene called HLA-B27 is associated with develops after an infection, often in the bowel or genital reactive arthritis, especially inflammation of the spine. areas. The infection causes activity in the immune However this is a perfectly normal gene and there are system. The normal role of your body’s immune system many more people who have this gene and do not get is to fight off infections to keep you healthy. In some reactive arthritis. people this activity of the immune system causes joints to become inflamed, however the joints themselves How is it diagnosed? are not actually infected. About one in 10 people with Your doctor will diagnose reactive arthritis from your specific types of infections will get reactive arthritis. symptoms and a physical examination. Your doctor may also order blood tests for inflammation, such as the What are the symptoms? erythrocyte sedimentation rate (ESR) and C-reactive Reactive arthritis usually begins a few weeks after an protein (CRP) tests. Blood tests may also help to rule infection. Symptoms can affect many parts of the body out other types of arthritis. -

A Description of the Clinical Features of Brimonidine- Associated Uveitis Alyssa Louie Primary Care Resident, San Francisco VA
Drug-induced intraocular inflammation: A description of the clinical features of brimonidine- associated uveitis Alyssa Louie Primary Care Resident, San Francisco VA Abstract: A description of the clinical features, diagnostic work-up, and management of acute anterior uveitis caused by brimonidine, a widely used glaucoma medication. I. Case History a. Patient demographics: 74 year-old white male b. Chief complaint: eye pain, redness, irritation for last 2 weeks c. Ocular and medical history: i. Ocular history 1. Primary open angle glaucoma OU, diagnosed 8 years ago 2. Senile cataracts OU, not visually significant 3. Type 2 Diabetes without retinopathy OU 4. No prior history of uveitis ii. Medical history: Diabetes Mellitus Type 2 iii. No known drug allergies d. Medications i. Ocular: dorzolamide BID OU (1.5 years), brimonidine BID OU (11 months), travatan QHS OU (5.5 years) ii. Medical: metformin 500mg tab BID PO II. Pertinent Findings a. Clinical exam i. Visual acuities: OD 20/20-, OS 20/20- ii. Goldmann applanation tonometry: 13 mm Hg OD, 13 mm Hg OS iii. Anterior segment 1. OU: 3+ diffuse conjunctival injection 2. OU: central and inferior granulomatous keratic precipitates 3. OU: Grade 1+ cell, 1+ flare 4. OU: No synechiae or iris changes were present iv. Posterior segment 1. Optic Nerve a. OD: Cup-to-disc ratio 0.70H/V, distinct margins b. OS: Cup-to-disc ratio 0.75H/V, distinct margins 2. Posterior pole, periphery, vitreous: unremarkable OU b. Laboratory Studies i. ACE, Lysozyme, FTA-ABS, VDRL, HLA-B27, Rheumatoid Factor, ANA, PPD, Chest X- ray: all negative/unreactive III. -

Diagnosing Dry Eye
MEDICAL ED NG UC UI AT A CONTINUING TIN IO CON N MEDICAL EDUCATION PUBLICATION CME ISSUE 14 Diagnosing Dry Eye ERIC D. DONNENFELD, MD Dry eye a ects tens of millions of patients and is among the most common reasons for eye care provider visits. Knowing what to look for, how, and in whom (hint: everyone) can help stem the tide of this quiet epidemic. Th e exact prevalence of dry eye is diffi cult to ascertain, for several reasons, including the absence of a single test (or universally accepted sequence of tests) for its diagnosis, and the fact that patient-reported symptoms are oft en poorly con- cordant with objective assessments.1 Estimates based on cohort studies suggest that about 5% to 35% of adults worldwide have dry eye, a rate that is expected to rise in the upcoming decades FIGURE 1 Lid margin with inspissated meibomian glands and pasty as common risk factors, including advanced age, increase.2,3 secretions indicative of MGD. Sometimes even higher estimates are cited, as dry eye symp- toms are oft en camoufl aged by other ocular surface condi- tions such as allergic conjunctivitis, surgery, and contact lens CATEGORIES AND MECHANISMS discomfort; in addition, many patients—up to 60% of those Dry eye is generally divided into two main categories based with objective evidence of dry eye—are pre-symptomatic.3 on the underlying cause: aqueous defi cient and evaporative.4 Th e landmark 2007 International Dry Eye Workshop Aqueous defi ciency describes inadequate tear production by (DEWS) report off ered the fi rst thorough expert review around the lacrimal glands. -

Confidential
CONFIDENTIAL CHILD’S MEDICAL INFORMATION The following is important information about my child’s medical condition and how the condition may affect their ability to fully participate in a regular school setting. The goal is to try to normalize every day school routines/activities while also meeting my child’s unique needs in the least disruptive manner. This document is not intended to replace any existing Individual Educational Plan (IEP) or the 504 Plan, but rather to serve as a supplement or addendum to enhance my child’s education. Medical information will be updated at the beginning of each new school year and throughout the school year as deemed necessary. “We may not look sick, but turn our bodies inside out and they will tell different stories.” Wade Sutherland CHILD’S NAME: ____________________________________________________________________________ ACADEMIC YEAR: _____________________GRADE: __________DOB: __________________AGE: _________ HOME ADDRESS: __________________________________________________________________________ PARENT/LEGAL GUARDIAN: ________________________________________________________________ PARENT/LEGAL GUARDIAN CONTACT NUMBER: ______________________________________________ SCHOOL: ________________________________________________________________________________ EMERGENCY CONTACT (2 PEOPLE) NAME: __________________________________________________________________________________ RELATIONSHIP: ____________________________ PHONE NUMBER: ________________________________ NAME: __________________________________________________________________________________ -

Comprehensive Pediatric Eye and Vision Examination
Guideline Brief 2017 EVIDENCE-BASED CLINICAL PRACTICE GUIDELINE COMPREHENSIVE PEDIATRIC EYE AND VISION EXAMINATION OVERVIEW TOPICS The American Optometric Association (AOA) convened an expert panel to develop a new evidence-based guideline that recommends annual comprehensive eye exams for children. This guideline is intended to help educate caregivers and ensure doctors of optometry are empowered to provide the best care for their young patients. With this guideline, parents and other healthcare professionals know which tests and interventions are proven to optimize a child’s eye care and the frequency with which children should receive a comprehensive eye exam to ensure their visual health. 1 1. AN EPIDEMIC OF UNDIAGNOSED EYE AND VISION PROBLEMS Children play and learn to develop skills needed for a successful life. If their eyes have problems or their vision is limited – as is the case with at least 25 percent of school-age 1 IN 5 PRESCHOOLERS children – their ability to participate in sports, learn in school, and observe the world around them may be significantly impaired and they can easily fall behind their peers. HAVE VISION PROBLEMS, AND BY THE TIME THEY Further evidence is provided in the Health and Medicine Division of the National Acade- mies of Sciences, Engineering, and Medicine (NASEM) report. ENTER SCHOOL, 25% WILL NEED OR WEAR Eyes mature even as a fetus develops, and the rapid changes a child goes through in CORRECTIVE LENSES the first six years of life are critical in the development of good eyesight. This same time frame represents a “vulnerability” period – one in which children are most susceptible to harmful vision changes. -
A Case of Anterior Ischemic Optic Neuropathy Associated with Uveitis
Clinical Ophthalmology Dovepress open access to scientific and medical research Open Access Full Text Article CASE REPORT A case of anterior ischemic optic neuropathy associated with uveitis Michitaka Sugahara Introduction: Here, we describe a patient who presented with anterior ischemic optic Takayuki Fujimoto neuropathy (AION) and subsequently developed uveitis. Kyoko Shidara Case: A 69-year-old man was referred to our hospital and initially presented with best-corrected Kenji Inoue visual acuities (BCVA) of 20/40 (right eye) and 20/1000 (left eye) and relative afferent pupillary Masato Wakakura defect. Slit-lamp examination revealed no signs of ocular inflammation in either eye. Fundus examination revealed left-eye swelling and a pale superior optic disc, and Goldmann perimetry Inouye Eye Hospital, Tokyo, Japan revealed left-eye inferior hemianopia. The patient was diagnosed with nonarteritic AION in the left eye. One week later, the patient returned to the hospital because of vision loss. The BCVA of the left eye was so poor that the patient could only count fingers. Slit-lamp examination revealed 1+ cells in the anterior chamber and the anterior vitreous in both eyes. Funduscopic examination revealed vasculitis and exudates in both eyes. The patient was diagnosed with bilateral panuveitis, and treatment with topical betamethasone was started. No other physical findings resulting from other autoimmune or infectious diseases were found. No additional treatments were administered, and optic disc edema in the left eye improved, and the retinal exudates disappeared in 3 months. The patient’s BCVA improved after cataract surgery was performed. Conclusion: Panuveitis most likely manifests after the development of AION.