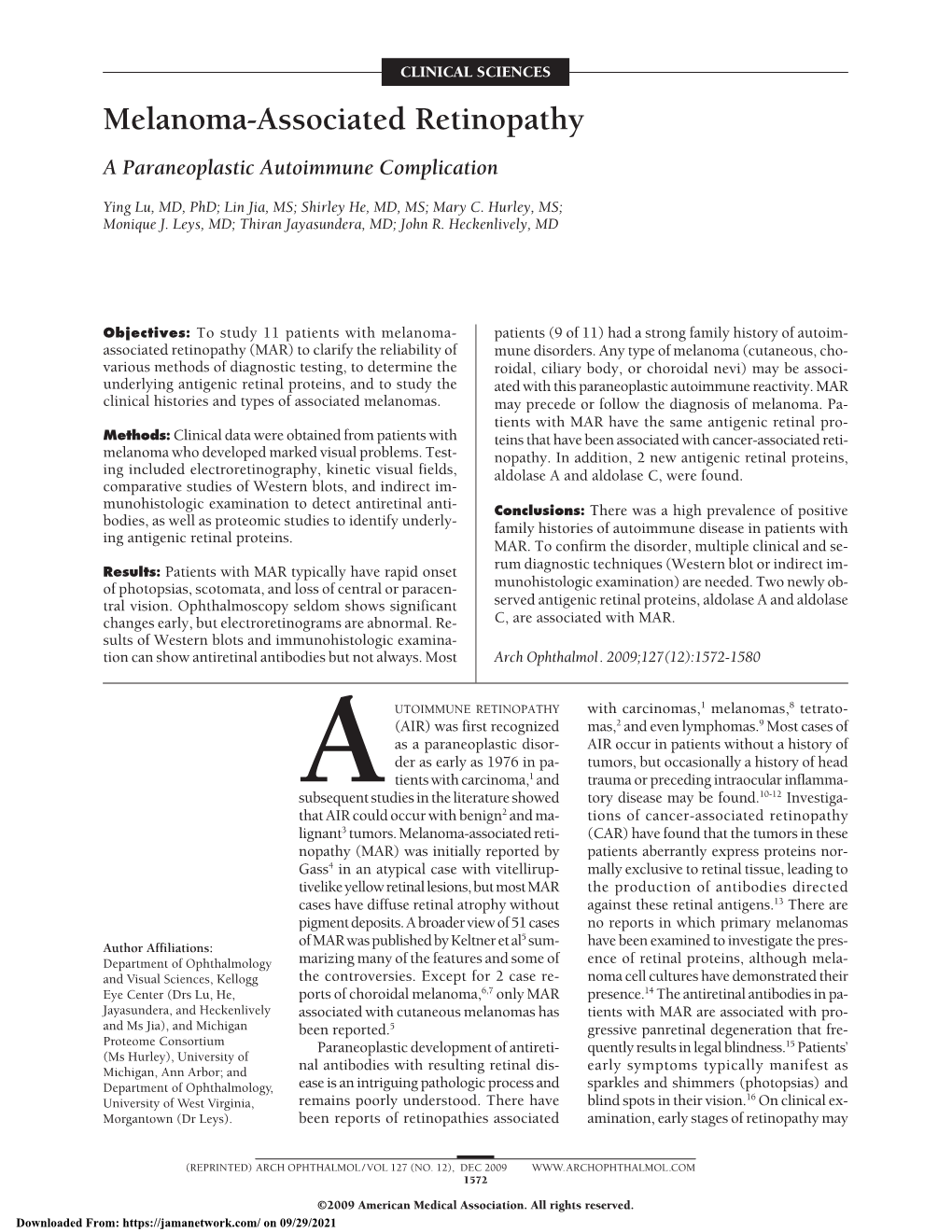
Melanoma-Associated Retinopathy a Paraneoplastic Autoimmune Complication
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early B-Cell Factors Are Required for Specifying Multiple Retinal Cell Types and Subtypes from Postmitotic Precursors
11902 • The Journal of Neuroscience, September 8, 2010 • 30(36):11902–11916 Development/Plasticity/Repair Early B-Cell Factors Are Required for Specifying Multiple Retinal Cell Types and Subtypes from Postmitotic Precursors Kangxin Jin,1,2 Haisong Jiang,1,2 Zeqian Mo,3 and Mengqing Xiang1,2 1Center for Advanced Biotechnology and Medicine and Department of Pediatrics, 2Graduate Program in Molecular Genetics, Microbiology and Immunology, and 3Department of Cell Biology and Neuroscience, University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School, Piscataway, New Jersey 08854 The establishment of functional retinal circuits in the mammalian retina depends critically on the proper generation and assembly of six classes of neurons, five of which consist of two or more subtypes that differ in morphologies, physiological properties, and/or sublaminar positions. How these diverse neuronal types and subtypes arise during retinogenesis still remains largely to be defined at the molecular level. Here we show that all four family members of the early B-cell factor (Ebf) helix-loop-helix transcription factors are similarly expressedduringmouseretinogenesisinseveralneuronaltypesandsubtypesincludingganglion,amacrine,bipolar,andhorizontalcells, and that their expression in ganglion cells depends on the ganglion cell specification factor Brn3b. Misexpressed Ebfs bias retinal precursors toward the fates of non-AII glycinergic amacrine, type 2 OFF-cone bipolar and horizontal cells, whereas a dominant-negative Ebf suppresses the differentiation of these cells as well as ganglion cells. Reducing Ebf1 expression by RNA interference (RNAi) leads to an inhibitory effect similar to that of the dominant-negative Ebf, effectively neutralizes the promotive effect of wild-type Ebf1, but has no impact on the promotive effect of an RNAi-resistant Ebf1. -

Synergetic Effect of Recoverin and Calmodulin on Regulation of Rhodopsin Kinase
Thomas Jefferson University Jefferson Digital Commons Department of Biochemistry and Molecular Department of Biochemistry and Molecular Biology Faculty Papers Biology 1-1-2012 Synergetic effect of recoverin and calmodulin on regulation of rhodopsin kinase. Ilya I Grigoriev Lomonosov Moscow State University Ivan I Senin Lomonosov Moscow State University Natalya K Tikhomirova Lomonosov Moscow State University Konstantin E Komolov Lomonosov Moscow State University; University of Oldenburg, Oldenburg, Germany; Department of FBiochemistrollow this andy and additional Molecular works Biology at: ,https:/ Thomas/jdc.jeff Jeffersonerson.edu/bmpfp University Ser geiPar tE of P theermy Medicalakov Biochemistry Commons, and the Medical Molecular Biology Commons LetInstitute us for knowBiological Instrumentationhow access of the tRussiano this Academy document of Sciences benefits ouy RecommendedSee next page for Citation additional authors Grigoriev, Ilya I; Senin, Ivan I; Tikhomirova, Natalya K; Komolov, Konstantin E; Permyakov, Sergei E; Zernii, Evgeni Yu; Koch, Karl-Wilhelm; and Philippov, Pavel P, "Synergetic effect of recoverin and calmodulin on regulation of rhodopsin kinase." (2012). Department of Biochemistry and Molecular Biology Faculty Papers. Paper 36. https://jdc.jefferson.edu/bmpfp/36 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Biochemistry and Molecular Biology Faculty Papers by an authorized administrator of the Jefferson Digital Commons. -

Diagnosis and Treatment of Paraneoplastic Syndromes 1
Instructions: • Each speaker will prepare a syllabus that must be submitted through the online submission system. • The length of the syllabus will be no shorter than 4 single spaced pages in essay (not point) format, plus references. • Use single spaced, 11 point type and (if possible) Times New Roman font. • When typing the text use word wrap, not hard returns to determine your lines. • If headings and subheadings are used, these may be highlighted by using all caps and bold. • Do not use the header or footer feature or endnotes in preparing the text. • The submission must be submitted online. Title: Diagnosis and Treatment of Paraneoplastic Syndromes Learning Objectives: 1. Describe the spectrum of paraneoplastic syndromes with neuro-ophthalmic features 2. Define the challenges in diagnosis of the paraneoplastic syndromes 3. Explain the therapeutic options for treatment of these diseases CME Questions: 1. The presence of serum antibodies against recoverin a. are pathognomonic for CAR b. are found in the majority of patients with lung cancer c. may be responsible apoptotic cell death in CAR patients d. are best detected by immunofluorescent studies on retina 2. Which of the following is correct regarding therapy for paraneoplastic neuro-ophthalmic disease: a. steroid therapy may be helpful in control of disease b. should be initiated only after there is validation for the presence of autoreactive antibodies c. cytoreduction of the primary tumor is not helpful in controlling the autoimmune component d. biologic immunomodulatory agents have no role in therapy 3. Lambert-Eaton myasthenic syndrome is associated with which of the following: a. -

Absence of S100A4 in the Mouse Lens Induces an Aberrant Retina-Specific Differentiation Program and Cataract
www.nature.com/scientificreports OPEN Absence of S100A4 in the mouse lens induces an aberrant retina‑specifc diferentiation program and cataract Rupalatha Maddala1*, Junyuan Gao2, Richard T. Mathias2, Tylor R. Lewis1, Vadim Y. Arshavsky1,3, Adriana Levine4, Jonathan M. Backer4,5, Anne R. Bresnick4 & Ponugoti V. Rao1,3* S100A4, a member of the S100 family of multifunctional calcium‑binding proteins, participates in several physiological and pathological processes. In this study, we demonstrate that S100A4 expression is robustly induced in diferentiating fber cells of the ocular lens and that S100A4 (−/−) knockout mice develop late‑onset cortical cataracts. Transcriptome profling of lenses from S100A4 (−/−) mice revealed a robust increase in the expression of multiple photoreceptor‑ and Müller glia‑specifc genes, as well as the olfactory sensory neuron‑specifc gene, S100A5. This aberrant transcriptional profle is characterized by corresponding increases in the levels of proteins encoded by the aberrantly upregulated genes. Ingenuity pathway network and curated pathway analyses of diferentially expressed genes in S100A4 (−/−) lenses identifed Crx and Nrl transcription factors as the most signifcant upstream regulators, and revealed that many of the upregulated genes possess promoters containing a high‑density of CpG islands bearing trimethylation marks at histone H3K27 and/or H3K4, respectively. In support of this fnding, we further documented that S100A4 (−/−) knockout lenses have altered levels of trimethylated H3K27 and H3K4. Taken together, -

Miami University – the Graduate School
MIAMI UNIVERSITY – THE GRADUATE SCHOOL CERTIFICATE FOR APPROVING THE DISSERTATION We hereby approve the Dissertation Of Elvis K. Tiburu Candidate for the Degree: Doctor of Philosophy Dr. Gary A. Lorigan, Director Dr. Christopher A. Makaroff, Reader Dr. Robert E. Minto, Reader Dr. Richard T. Taylor, Reader Dr. David G. Pennock Graduate School Representative ABSTRACT DEVELOPMENT OF NEW METHODS FOR THE ALIGNMENT OF LONGER CHAIN PHOSPHOLIPIDS IN BICELLES AND SOLID-STATE NMR STUDIES OF PHOSPHOLAMBAN by Elvis K. Tiburu Magnetically aligned phospholipid bilayers or bicelles are model systems that mimic biological membranes for magnetic resonance studies. A long chain phospholipid bilayer system that spontaneously aligns in a static magnetic field was characterized utilizing solid-state NMR spectroscopy. The oriented membrane system was composed of a mixture of the bilayer-forming phospholipid palmitoylstearoylphosphatidylcholine (PSPC) and the short-chain phospholipid dihexanoylphosphatidylcholine (DHPC) that breaks up the extended bilayers into bilayered micelles or bicelles that are highly hydrated. Traditionally, the shorter 14-carbon chain phospholipid dimyristoyl- phosphatidylcholine (DMPC) has been utilized as the bilayer-forming phospholipid in bicelle studies. The effect of cholesterol in bicelles containing chain perdeuterated 2 DMPC, a partially deuterated (a-[2,2,3,4,4,6- H6]) cholesterol, and stearic acid-d35 has been reported as a function of temperature using 2H solid-state NMR spectroscopy. The order parameters of the labeled probes were calculated and compared with values obtained from unoriented samples in the literature. In addition, 2H solid-state NMR spectroscopy was used to investigate the orientation and side chain dynamics of specific- labeled methyl groups of leucines in PLB in unoriented as well as in magnetically and mechanically aligned phospholipids bilayers. -

Biochemical Journal
www.biochemj.org Biochem. J. (2007) 405, 199–221 (Printed in Great Britain) doi:10.1042/BJ20070255 199 REVIEW ARTICLE Structures and metal-ion-binding properties of the Ca2+-binding helix–loop–helix EF-hand motifs Jessica L. GIFFORD*, Michael P. WALSH† and Hans J. VOGEL*1 *Structural Biology Research Group, Department of Biological Sciences, University of Calgary, Calgary, Alberta, Canada T2N 1N4, and †Department of Biochemistry and Molecular Biology, Faculty of Medicine, University of Calgary, Calgary, Alberta, Canada T2N 4N1 The ‘EF-hand’ Ca2+-binding motif plays an essential role in interaction site or structure formation from a molten-globule eukaryotic cellular signalling, and the proteins containing this apo state. EF-hand proteins exhibit various sensitivities to Ca2+, motif constitute a large and functionally diverse family. The EF- reflecting the intrinsic binding ability of the EF-hand as well as hand is defined by its helix–loop–helix secondary structure as the degree of co-operativity in Ca2+ binding to paired EF-hands. well as the ligands presented by the loop to bind the Ca2+ ion. The Two additional factors can influence the ability of an EF-hand identity of these ligands is semi-conserved in the most common to bind Ca2+: selectivity over Mg2+ (a cation with very similar (the ‘canonical’) EF-hand; however, several non-canonical EF- chemical properties to Ca2+ and with a cytoplasmic concentration hands exist that bind Ca2+ by a different co-ordination mechanism. several orders of magnitude higher) and interaction with a protein EF-hands tend to occur in pairs, which form a discrete domain so target. -

Autoantibody Profiles and Clinical Association in Thai Patients With
www.nature.com/scientificreports OPEN Autoantibody profles and clinical association in Thai patients with autoimmune retinopathy Aulia Rahmi Pawestri1,8, Niracha Arjkongharn2,8, Ragkit Suvannaboon2,3,8, Aekkachai Tuekprakhon2,4, Vichien Srimuninnimit5, Suthipol Udompunthurak6, La‑ongsri Atchaneeyasakul2, Ajchara Koolvisoot7* & Adisak Trinavarat2* Autoimmune retinopathy (AIR) is a rare immune‑mediated infammation of the retina. The autoantibodies against retinal proteins and glycolytic enzymes were reported to be involved in the pathogenesis. This retrospective cohort study assessed the antiretinal autoantibody profles and their association with clinical outcomes of AIR patients in Thailand. We included 44 patients, 75% were females, with the overall median age of onset of 48 (17–74, IQR 40–55.5) years. Common clinical presentations were nyctalopia (65.9%), blurred vision (52.3%), constricted visual feld (43.2%), and nonrecordable electroretinography (65.9%). Underlying malignancy and autoimmune diseases were found in 2 and 12 female patients, respectively. We found 41 autoantibodies, with anti‑α‑enolase (65.9%) showing the highest prevalence, followed by anti‑CAII (43.2%), anti‑aldolase (40.9%), and anti‑GAPDH (36.4%). Anti‑aldolase was associated with male gender (P = 0.012, OR 7.11, 95% CI 1.54– 32.91). Anti‑CAII showed signifcant association with age of onset (P = 0.025, 95% CI − 17.28 to − 1.24), while anti‑α‑enolase (P = 0.002, OR 4.37, 95% CI 1.83–10.37) and anti‑GAPDH (P = 0.001, OR 1.87, 95% CI 1.32–2.64) were signifcantly associated with nonrecordable electroretinography. Association between the antibody profles and clinical outcomes may be used to direct and adjust the treatment plans and provide insights in the pathogenesis of AIR. -
Dimerization of Neuronal Calcium Sensor Proteins
UC Davis UC Davis Previously Published Works Title Dimerization of Neuronal Calcium Sensor Proteins. Permalink https://escholarship.org/uc/item/8426s2jv Author Ames, James B Publication Date 2018 DOI 10.3389/fnmol.2018.00397 Peer reviewed eScholarship.org Powered by the California Digital Library University of California REVIEW published: 02 November 2018 doi: 10.3389/fnmol.2018.00397 Dimerization of Neuronal Calcium Sensor Proteins James B. Ames* Department of Chemistry, University of California, Davis, Davis, CA, United States 2 Neuronal calcium sensor (NCS) proteins are EF-hand containing Ca C binding proteins that regulate sensory signal transduction. Many NCS proteins (recoverin, GCAPs, neurocalcin and visinin-like protein 1 (VILIP1)) form functional dimers under physiological conditions. The dimeric NCS proteins have similar amino acid sequences (50% homology) but each bind to and regulate very different physiological targets. Retinal 2 recoverin binds to rhodopsin kinase and promotes Ca C-dependent desensitization of light-excited rhodopsin during visual phototransduction. The guanylyl cyclase activating proteins (GCAP1–5) each bind and activate retinal guanylyl cyclases (RetGCs) in light- adapted photoreceptors. VILIP1 binds to membrane targets that modulate neuronal secretion. Here, I review atomic-level structures of dimeric forms of recoverin, GCAPs and VILIP1. The distinct dimeric structures in each case suggest that NCS dimerization may play a role in modulating specific target recognition. The dimerization of recoverin 2 2 and VILIP1 is Ca C-dependent and enhances their membrane-targeting Ca C-myristoyl switch function. The dimerization of GCAP1 and GCAP2 facilitate their binding to dimeric 2 RetGCs and may allosterically control the Ca C-dependent activation of RetGCs. -

Paraneoplastic Neurological and Muscular Syndromes
Paraneoplastic neurological and muscular syndromes Short compendium Version 4.5, April 2016 By Finn E. Somnier, M.D., D.Sc. (Med.), copyright ® Department of Autoimmunology and Biomarkers, Statens Serum Institut, Copenhagen, Denmark 30/01/2016, Copyright, Finn E. Somnier, MD., D.S. (Med.) Table of contents PARANEOPLASTIC NEUROLOGICAL SYNDROMES .................................................... 4 DEFINITION, SPECIAL FEATURES, IMMUNE MECHANISMS ................................................................ 4 SHORT INTRODUCTION TO THE IMMUNE SYSTEM .................................................. 7 DIAGNOSTIC STRATEGY ..................................................................................................... 12 THERAPEUTIC CONSIDERATIONS .................................................................................. 18 SYNDROMES OF THE CENTRAL NERVOUS SYSTEM ................................................ 22 MORVAN’S FIBRILLARY CHOREA ................................................................................................ 22 PARANEOPLASTIC CEREBELLAR DEGENERATION (PCD) ...................................................... 24 Anti-Hu syndrome .................................................................................................................. 25 Anti-Yo syndrome ................................................................................................................... 26 Anti-CV2 / CRMP5 syndrome ............................................................................................ -
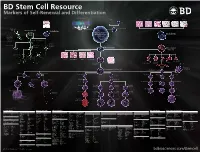
BD Stem Cell Resource Markers of Self-Renewal and Differentiation
BD Stem Cell Resource Markers of Self-Renewal and Differentiation 23-9953-02 Self Renewing Pathway TGF-β/Activin Sperm Liver Thymus Pancreas Thyroid Lung Intestine Wnt BMP-SMad Erk-MAPK Skin and Hair JAK-STAT Wnt TGF-β/Activin BMP4 bFGF LIF LIFR gp130 Egg p p p Jak β-catenin Smads 175 MEK/ERK Stat3 C-myc Sox2 Oct4 Nanog Smads 2/3 Neural Crest Primordial Germ Cell Stem Cell Neural Stem Cell Self Renewal Ectoderm Embryonic Stem Cell or Induced Pluripotent Endoderm Neurons, Glia Stem Cell Smooth Muscle Cardiac Tissue Chondrocytes Glial Restricted Progenitor Osteocytes Neuronal Type 1 Astrocyte Oligodendrocyte Restricted Progenitor Progenitor Mesoderm Mesenchymal Stem Cell Type 2 Astrocyte Endothelium Oligodendrocyte Neuron Heart Skeletal Muscle Kidney Smooth Muscle Myoblast Adipocyte (Fat) Chondrocyte Fibroblast Osteoblast (Bone) Hemangioblast (Cartilage) Myotube (Muscle) Plasmacytoid Dendritic Cell Hematopoietic Stem Cell Committed Lymphoid Progenitor Monoblast Megakaryoblast Proerythroblast Pre-NK Cell Thymocyte Pre B Cell Myeloblast Erythroblast Progranulocyte Monocyte Myeloid Dendrtitic Cell Megakaryocyte NK Lymphoblast T-Lymphoblast B-Lymphoblast Normoblast Neutrophilic Eosinophilic Basophilic Myelocyte Myelocyte Myelocyte NK Cell T Cell B Cell Macrophage Thrombocytes Reticulocyte Neutrophilic Eosinophilic Basophilic (Platelets) Band Cell Band Cell Band Cell Plasma Cell Erythrocyte Neutrophil Eosinophil Basophil (Red Blood Cell) White colored markers are available from BD Biosciences Ectoderm Markers Embryonic Stem Cells Mesoderm Markers -

New Approach for Untangling the Role of Uncommon Calcium-Binding Proteins in the Central Nervous System
brain sciences Review New Approach for Untangling the Role of Uncommon Calcium-Binding Proteins in the Central Nervous System Krisztina Kelemen * and Tibor Szilágyi Department of Physiology, Doctoral School, Faculty of Medicine, George Emil Palade University of Medicine, Pharmacy, Science, and Technology of Targu Mures, 540142 Târgu Mures, , Romania; [email protected] * Correspondence: [email protected]; Tel.: +40-746-248064 Abstract: Although Ca2+ ion plays an essential role in cellular physiology, calcium-binding proteins (CaBPs) were long used for mainly as immunohistochemical markers of specific cell types in different regions of the central nervous system. They are a heterogeneous and wide-ranging group of proteins. Their function was studied intensively in the last two decades and a tremendous amount of informa- tion was gathered about them. Girard et al. compiled a comprehensive list of the gene-expression profiles of the entire EF-hand gene superfamily in the murine brain. We selected from this database those CaBPs which are related to information processing and/or neuronal signalling, have a Ca2+- buffer activity, Ca2+-sensor activity, modulator of Ca2+-channel activity, or a yet unknown function. In this way we created a gene function-based selection of the CaBPs. We cross-referenced these findings with publicly available, high-quality RNA-sequencing and in situ hybridization databases (Human Protein Atlas (HPA), Brain RNA-seq database and Allen Brain Atlas integrated into the HPA) and created gene expression heat maps of the regional and cell type-specific expression levels of the selected CaBPs. This represents a useful tool to predict and investigate different expression patterns and functions of the less-known CaBPs of the central nervous system. -

Control of Rhodopsin Activity in Vision
Control of rhodopsin DENIS A. BAYLOR, MARIE E. BURNS activity in vision Abstract high concentration in the cytoplasm in darkness and that binds to cationic channels in the Although rhodopsin's role in activating the surface membrane, holding them open. phototransduction cascade is well known, the Hydrolysis of cGMP allows the channels to processes that deactivate rhodopsin, and thus close, interrupting an inward current of sodium, the rest of the cascade, are less well calcium and magnesium ions and producing a understood. At least three proteins appear to hyperpolarisation of the membrane. The play a role: rhodopsin kinase, arrestin and hyperpolarisation reduces the rate at which recoverin. Here we review recent physiological neurotransmitter is released from the synaptic studies of the molecular mechanisms of terminal of the rod. rhodopsin deactivation. The approach was to The purpose of this paper is to review recent monitor the light responses of individual work on the important but still poorly mouse rods in which rhodopsin was altered or understood mechanisms that terminate the arrestin was deleted by transgenic techniques. light-evoked catalytic activity of rhodopsin. Removal of rhodopsin's carboxy-terminal These mechanisms, which fix the intensity and residues which contain phosphorylation sites duration of the activation of the transduction implicated in deactivation, prolonged the flash cascade, need to satisfy strong functional response 20-fold and caused it to become constraints. Rhodopsin activity must be highly variable. In rods that did not express arrestin the flash response recovered partially, terminated rapidly so that an absorbed photon but final recovery was slowed over lOO-fold.