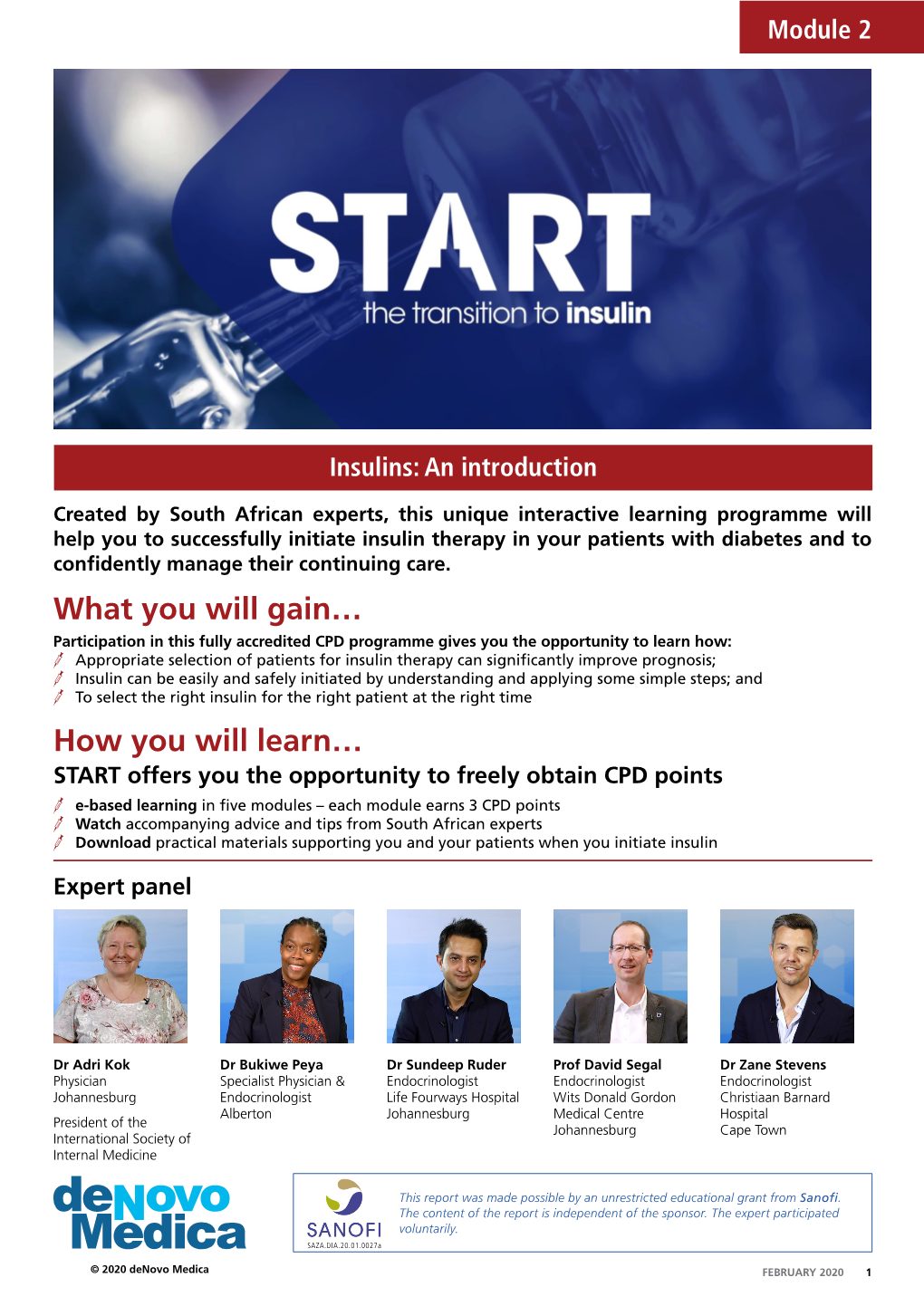
Insulins: an Introduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ATC) Codes and Drug Identification Numbers (Dins
Anatomical Therapeutic Chemical (ATC) Codes and Drug Identification Numbers (DINs) of Drugs in the Drug Program Information Network (DPIN) Used to Define Diabetes in Manitoba Children from 2001/02–2003/04 to 2007/08–2009/10 DIN ATC Code Equivalent Generic Product Name Product Description Ingredients 446564 A10AA01 INSULIN ZINC (BEEF/PORK) ILETIN INSULIN REGULAR 100UNIT INSULIN ZINC (100 UNIT) 1986805 A10AA01 INSULIN INJECTION HUMAN SEMI-* VELOSULIN HUMAN INJ LIQ 100U/M INSULIN INJECTION HUMAN SEMI-SYNTHETIC (100 UNIT) 446572 A10AA02 INSULIN ISOPHANE(NPH) ((BEEF * ILETIN NPH INSULIN 100UNIT/ML INSULIN ISOPHANE (NPH) (100 UNIT) 446580 A10AA02 INSULIN ZINC ((BEEF & PORK)) ILETIN LENTE INSULIN INJ 100UN INSULIN ZINC (100 UNIT) 586714 A10AB01 INSULIN DNA ORIGIN HUMAN HUMULIN R INJ INSULIN SEMI SYNTHETIC HUMAN (100 UNIT) 1959220 A10AB01 INSULIN INJECTION HUMAN BIOSY HUMULIN R CARTRIDGE INSULIN INJECTION HUMAN BIOSYNTHETIC (100 UNIT) 2024233 A10AB01 INSULIN INJECTION HUMAN BIOSY NOVOLIN GE TORONTO INJ 100U/ML INSULIN INJECTION HUMAN BIOSYNTHETIC (100 UNIT) 2024284 A10AB01 INSULIN INJECTION HUMAN BIOSY* NOVOLIN GE TORONTO PENFILL INJ INSULIN INJECTION HUMAN BIOSYNTHETIC (100 UNIT) 2025256 A10AB01 INSULIN INJECTION HUMAN BIOSY NOVOLINSET GE TORONTO INSULIN INJECTION HUMAN BIOSYNTHETIC (100 UNIT) 1934074 A10AB02 INSULIN SULPHATED BEEF SULPHATED INSULIN INJ LIQ 100U INSULIN SULPHATED BEEF (100 UNIT) 513644 A10AB03 INSULIN (REGULAR) PORK REGULAR PURIFIED PORK INSULIN INSULIN (PORK) (100 UNIT) 2275872 A10AB03 INSULIN INJECTION PORK HYPURIN REGULAR -

United States Experience of Insulin Degludec Alone Or in Combination for Type 1 and Type 2 Diabetes
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2017 Volume: 11 Drug Design, Development and Therapy Dovepress Running head verso: Rendell Running head recto: Degludec insulin in the USA open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S132581 Open Access Full Text Article REVIEW United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes Marc Rendell1,2 Abstract: Insulin degludec has been the product of a sophisticated and systematic biochemical 1The Rose Salter Medical Research engineering program which began with the release of insulin detemir. The goal was to pro- Foundation, 2The Association of duce a long-lasting basal insulin with low individual variability. Certainly, this goal has been Diabetes Investigators, Newport achieved. Degludec has a duration of action approaching twice that of glargine. Another advan- Coast, CA, USA tage of degludec is in its lack of unpredictable copolymerization of added aspart. In several studies, degludec has shown lower rates of nocturnal hypoglycemia than glargine. Degludec can be administered flexibly with a very flat insulin concentration curve at any time of day. Initial US Food and Drug Administration concerns about a possible increase in cardiac events in degludec-treated patients have been allayed by the results of a study targeting individuals with high cardiac risk. Degludec is now marketed in the US competing with glargine. Despite the long duration of action of degludec, attempted administration three times weekly resulted For personal use only. in less effective lowering of glycated hemoglobin and an increased incidence of hypoglycemia compared to daily glargine. -

Institute of Pharmacology Madras Medical College Chennai - 600 003
RED BLOOD CELL MORPHOLOGY AS A MARKER OF OXIDATIVE STRESS IN EARLY TYPE 2 DIABETES PATIENTS AND EFFICACY OF ANTIOXIDANTS AS AN ADD ON THERAPY TO STANDARD TREATMENT - A RANDOMIZED, OPEN LABEL, COMPARATIVE PILOT STUDY Dissertation submitted to THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY In partial fulfillment for the award of the degree of DOCTOR OF MEDICINE IN PHARMACOLOGY INSTITUTE OF PHARMACOLOGY MADRAS MEDICAL COLLEGE CHENNAI - 600 003 OCTOBER 2016 CERTIFICATE This is to certify that the dissertation entitled, “RED BLOOD CELL MORPHOLOGY AS A MARKER OF OXIDATIVE STRESS IN EARLY TYPE 2 DIABETES PATIENTS AND EFFICACY OF ANTIOXIDANTS AS AN ADD ON THERAPY TO STANDARD TREATMENT - A RANDOMIZED, OPEN LABEL, COMPARATIVE PILOT STUDY” submitted by DR. ROHINI ANN MATHEW, in partial fulfilment for the award of the degree of Doctor of Medicine in Pharmacology by The Tamil Nadu Dr.M.G.R.Medical University, Chennai is a bonafide record of the work done by her in the Institute of Pharmacology, Madras Medical College during the academic year 2013-16. DEAN DIRECTOR AND PROFESSOR, Madras Medical College & Institute of Pharmacology, Rajiv Gandhi Govt. General Hospital Madras Medical College, Chennai – 600 003. Chennai – 600 003. CERTIFICATE OF THE GUIDE This is to certify that the dissertation entitled, “RED BLOOD CELL MORPHOLOGY AS A MARKER OF OXIDATIVE STRESS IN EARLY TYPE 2 DIABETES PATIENTS AND EFFICACY OF ANTIOXIDANTS AS AN ADD ON THERAPY TO STANDARD TREATMENT - A RANDOMIZED, OPEN LABEL, COMPARATIVE PILOT STUDY” submitted by DR. ROHINI ANN MATHEW, in partial fulfillment for the award of the degree of Doctor of Medicine in Pharmacology by The Tamil Nadu Dr.M.G.R.Medical University, Chennai is a record of original work done by her under my guidance and supervision in the Institute of Pharmacology, Madras Medical College during the academic year 2013-16. -

BRINK: 2021: Insulin Page 1 of 43 Insulin Past, Present and Future: 100 Years from the Nobel Prize* Stuart J. Brink, MD Senior E
BRINK: 2021: Insulin Insulin Past, Present and Future: 100 Years from the Nobel Prize* Stuart J. Brink, MD Senior Endocrinologist, New England Diabetes and Endocrinology Center (NEDEC) and Associate Clinical Professor of Pediatrics, Tufts University School of Medicine, Boston, MA, USA Clinical Instructor in Pediatrics, Harvard Medical School, Boston, MA, USA Address: NEDEC, 196 Pleasant Street, Newton Centre MA 02459 USA The Pancreas, the In the pre- almost universally fatal. Most presented in childhood or adolescence with classical symptoms of diabetes, became cachectic and emaciated from significant glycosuria as well as catabolic changes causing muscle wasting, weakness and loss of body fat, severe weight loss reflecting acute insulin deficiency and often there was diabetic ketoacidosis, decompensation, coma and deat mellitus. In financially distressed parts of the world where medical care is minimally available or just too expensive or too far away, not much has changed about diabetes mellitus for children and adolescents until programs such as Changing Diabetes in Children and Life for a Child as well as Insulin for Life offered hope and insulin - sometimes also offering trained diabetes staff, glucose meters, test strips and lancets as well - in recent years.1 Instead of dying at rates exceeding 95%, such children now are living relatively normal lives with their families and friends, attending schools and thriving. It took a very long time, however, for medical specialists to determine that it was the pancreas that was the site of the problem.2 Oskar Minkowski working with Joseph Von Mering in 1889 in Strasbourg identified that the pancreas was the likely source of the problem after pancreatectomized dogs, in experiments concerning digestive effects of the pancreas, became diabetic and died in their laboratories. -

Feline Diabetes Mellitus Updates on Diagnosis & Treatment David Bruyette, DVM, Diplomate ACVIM, and Karen Eiler, DVM, MS, Diplomate ACVIM
PEER REVIEWED FELINE DIABETES MELLITUS Updates on Diagnosis & Treatment David Bruyette, DVM, Diplomate ACVIM, and Karen Eiler, DVM, MS, Diplomate ACVIM Feline Friendly Article iabetes mellitus (DM) is a commonly encoun- tinction to Type II DM in which the cause of insulin tered feline endocrine disease.1 DM is defined resistance is often unknown. as persistent hyperglycemia and glycosuria Ddue to an absolute or relative insulin defi- PATHOGENESIS ciency. The most common causes of feline DM are: Amylin, also known as islet amyloid polypeptide • Islet cell amyloidosis (IAPP), is synthesized in the Islets of Langerhans and • Obesity co-secreted with insulin. In cats with insulin resis- • Chronic pancreatitis. tance, amylin and insulin secretion increase concur- rently. Over time, amylin overproduction progresses CLASSIFICATION to diabetes due to 2 phenomena: Insulin is secreted exclusively from beta cells in the 1. Amylin can be enzymatically converted to amyloid, pancreas’ Islets of Langerhans. Insulin deficiency which has a direct cytotoxic effect on islet cells.5 occurs when beta cells are destroyed or their function 2. In addition, amylin itself inhibits further insulin impaired, and the pathogenesis of beta cell dysfunc- secretion in a paracrine effect.5 tion is used to classify DM. Both contribute to initial glucose intolerance and, In humans, DM is classified as: eventually, overt hyperglycemia and glucosuria. • Type I (insulin dependent): Results from autoim- mune damage to the Islets; associated with complete DIAGNOSIS lack of insulin DM is diagnosed based on clinical signs and laboratory • Type II (noninsulin dependent): Characterized by testing. abnormal insulin secretion and peripheral insulin resistance Clinical Signs • Gestational, congenital, neonatal, or monogenic. -

WHAT I LEARNED from MY DIABETIC CAT: TREATMENTENDOCRINOLOGY Ellen N
WHAT I LEARNED FROM MY DIABETIC CAT: TREATMENTENDOCRINOLOGY Ellen N. Behrend, VMD, PhD, DACVIM Treatment of diabetes mellitus (DM) can be quite frustrating. Human recombinant Lente and Ultralente preparations, long used to treat DM in veterinary medicine, are no longer available. Vetsulin, a porcine Lente, is available and is the only insulin approved for use in dogs. Glargine (Lantus) is a genetically-engineered recombinant human insulin available now for a number of years. Within the last few years, glargine has been used in cats; reports are very promising for getting good control and, more importantly, for inducing DM remission. Therapy of any disease is ideally aimed toward the underlying abnormality. In Type I DM, a lack of insulin exists, so treatment provides an exogenous source. Type I diabetics do not have the metabolic abnormalities present in Type II DM that are addressed by oral hypoglycemics. Consequently, administration of oral hypoglycemics to Type I diabetics is inappropriate, with the exception of acarbose. For Type II DM, oral hypoglycemic agents can be used initially, but as Type II DM progresses, exogenous insulin injections will be required. Dogs are mainly Type I diabetics.1;2 Accordingly, oral hypoglycemics have not been used widely in this species. Cats are believed to be mainly Type II, at least initially. In any case, patients with advanced Type II DM and glucose toxicity, a population likely to represent the majority of diabetic cats, will have totally lost insulin secretory ability. Accordingly, some diabetic cats will respond to oral hypoglycemic agents but most will require insulin therapy. For cats, the best case scenario is to have the DM resolve. -

Future of Newer Basal Insulin
ESICON 2012 Kolkata Mini-Review Future of newer basal insulin S. V. Madhu, M. Velmurugan1 Department of Medicine, Division of Endocrinology and Metabolism, 1Department of Medicine, University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, India ABSTRACT Basal insulin have been developed over the years. In recent times newer analogues have been added to the armanentarium for diabetes therapy. This review specifically reviews the current status of different basal insulins Key words: Basal insulin, diabetes, degludec INTRODUCTION insulin that mimics the basal insulin secretion and to provide short‑acting insulin with meals that approximates Since its first clinical use in 1920s, insulin remains the the insulin bursts occurring with meals [Figure 1]. cornerstone in the management of both type 1 and type 2 diabetes mellitus. Further, in late 1970s, insulin therapy was EVOLUTION OF BASAL INSULINS complimented by the availability of recombinant human insulin,[1] which was a more acceptable form of insulin An ideal, basal insulin should have a peak‑less as it had fewer side effects. Subsequently, recombinant pharmacodynamic profile, at least 24 h of duration of technology led to development of insulin analogs, in which action, very low risk of hypoglycemia, should be tolerated structural modifications were introduced in the amino well in both type 1 and type 2 diabetes mellitus, and should have predictable action without any intra and inter acid sequences to human insulin so as to get the desired [3] pharmacokinetic and pharmacodynamic profile. individual variability. The quest for the search of such an ideal basal insulin continues. The strategy behind insulin therapy is to simulate the body’s Intermediate acting insulin neutal protamine physiological insulin secretion. -

Management of Type 2 Diabetes Mellitus - a Pharmacoepidemiological Review
MANAGEMENT OF TYPE 2 DIABETES MELLITUS - A PHARMACOEPIDEMIOLOGICAL REVIEW ANUSOOYA SAUGUR 2011 MANAGEMENT OF TYPE 2 DIABETES MELLITUS - A PHARMACOEPIDEMIOLOGICAL REVIEW By Anusooya Saugur Submitted in fulfilment of the requirements for the degree of Magister Pharmaciae at the Nelson Mandela Metropolitan University November 2011 Supervisor: Ms Lia Kritiotis Co-supervisor: Ms Susan Burton DECLARATION I, Anusooya Saugur (206080380), hereby declare that the dissertation for Magister Pharmaciae is my own work and that it has not been previously submitted for assessment or completion of any postgraduate qualification to another university or for another qualification. Anusooya Saugur ACKNOWLEDGEMENTS During the course of this masters‟ degree, I have encountered numerous people who have helped and supported me in different ways. I would like to genuinely acknowledge their contribution to this journey and they are: My supervisors, Ms Lia Kritiotis and Mrs Susan Burton for their support. The Nelson Mandela Metropolitan University for providing the financial assistance over the two years of the postgraduate degree. Mr Danie Venter from the Statistics Department and Mrs Hayley Irvine from the Computing Sciences Department who both played a major role in the initial phase of the research. Dr Jacques Pietersen who helped me extensively with statistical assistance. My friends for their support in this endeavour. My family for encouraging me to pursue a postgraduate degree, for being supportive of my decisions and for their patience with me. Their -

New Options in Insulin Therapy Helena Schmid*
0021-7557/07/83-05-Suppl/S146 Jornal de Pediatria Copyright © 2007 by Sociedade Brasileira de Pediatria REVIEW ARTICLE New options in insulin therapy Helena Schmid* Abstract Objective: To review the new options in insulin therapy for controlling diabetes mellitus in children and adolescents. Sources: Articles indexed in PubMed were located using the search terms insulin analogs in children and adolescents and reviewed. Information was also obtained from American Diabetes Association and Sociedade Brasileira de Diabetes consensus documents. Summary of the findings: Information is presented on new analogs of insulin and, for purposes of comparison, the other insulin modalities currently available are also reviewed, focusing on insulin therapies which attempt to ap- proximate basal-bolus treatment strategies to physiology. With the objective of obtaining improved metabolic control, more and more children are being put on multiple daily injection regimes or using continuous subcutaneous insulin infusion. It is difficult to achieve optimum glycemic control in children due to the increased risk of hypoglycemia result- ing from the great variability in dietary intake habits and in physical activity levels. With diabetes type 1, if rapid-acting analogs are given subcutaneously in bolus, they generally reduce hypoglycemia episodes and postprandial glycemia levels, compared with regular human insulin, while basal analogs tend to reduce particularly the number of episodes of nocturnal hypoglycemia. Conclusions: Although the benefits to individual metabolic and clinical outcomes appear modest, the majority of studies demonstrate benefits when insulin analogs are used in the treatment of diabetes type 1 or 2. J Pediatr (Rio J). 2007;83(5 Suppl):S146-154: Diabetes mellitus, insulin analogs, infusion pumps, monitoring. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0017238 A1 Kidron (43) Pub
US 2015.0017238A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0017238 A1 Kidron (43) Pub. Date: Jan. 15, 2015 (54) METHODS AND COMPOSITIONS FOR Publication Classification TREATING DABETES (51) Int. Cl. (71) Applicant: Oramed Ltd., Jerusalem (IL) A638/28 (2006.01) A638/57 (2006.01) (72) Inventor: Miriam Kidron, Jerusalem (IL) A638/55 (2006.01) A638/56 (2006.01) (73) Assignee: Oramed, Ltd., Jerusalem (IL) 469/48 (2006.01) A638/26 (2006.01) (21) Appl. No.: 14/370,452 (52) U.S. Cl. CPC ............... A61K 38/28 (2013.01); A61 K9/4808 (22) PCT Filed: Jan. 3, 2013 (2013.01); A61 K38/26 (2013.01); A61K38/55 (2013.01); A61 K38/56 (2013.01); A61K38/57 S371 (c)(1), USPC ............................................ 424/455; 514/6.5 Related U.S. Application Data d herein a methods and compositions for treating iabetes mellitus, concerning oral pharmaceutical composi (60) Provisional application No. 61/631,339, filed on Jan. tions comprising insulin in combination with a GLP-1 ana 3, 2012. logue. Patent Application Publication Jan. 15, 2015 Sheet 1 of 5 US 2015/001 7238A1 Patent Application Publication Jan. 15, 2015 Sheet 2 of 5 US 2015/0017238A1 Z-|| *| Patent Application Publication Jan. 15, 2015 Sheet 3 of 5 US 201S/0017238A1 e C r 5 e E O " c 3 CS S E S. s N d S 3S 3 g S S S S S. S S E R S S S Se Glucose (mg/dL) Glucose (mg/dL) d ve e 2 9. s s E cd E od s g E. -

United States Experience of Insulin Degludec Alone Or in Combination for Type 1 and Type 2 Diabetes
Journal name: Drug Design, Development and Therapy Article Designation: Review Year: 2017 Volume: 11 Drug Design, Development and Therapy Dovepress Running head verso: Rendell Running head recto: Degludec insulin in the USA open access to scientific and medical research DOI: http://dx.doi.org/10.2147/DDDT.S132581 Open Access Full Text Article REVIEW United States experience of insulin degludec alone or in combination for type 1 and type 2 diabetes Marc Rendell1,2 Abstract: Insulin degludec has been the product of a sophisticated and systematic biochemical 1The Rose Salter Medical Research engineering program which began with the release of insulin detemir. The goal was to pro- Foundation, 2The Association of duce a long-lasting basal insulin with low individual variability. Certainly, this goal has been Diabetes Investigators, Newport achieved. Degludec has a duration of action approaching twice that of glargine. Another advan- Coast, CA, USA tage of degludec is in its lack of unpredictable copolymerization of added aspart. In several studies, degludec has shown lower rates of nocturnal hypoglycemia than glargine. Degludec can be administered flexibly with a very flat insulin concentration curve at any time of day. Initial US Food and Drug Administration concerns about a possible increase in cardiac events in degludec-treated patients have been allayed by the results of a study targeting individuals with high cardiac risk. Degludec is now marketed in the US competing with glargine. Despite the long duration of action of degludec, attempted administration three times weekly resulted in less effective lowering of glycated hemoglobin and an increased incidence of hypoglycemia compared to daily glargine. -

Article (Published Version)
Article Insulin under the influence of light URSINO, Gloria, COPPARI, Roberto Abstract The discovery and administration of exogenous insulin has revolutionised diabetes treatment and continues, almost 100 years on, to be the basis for the management of insulin deficiency. However, insulin therapy still has potentially life-threatening side effects such as hypoglycaemia and increased risk of cardiovascular disease. So far, improvements in insulin therapy have focused mainly on modulating its pharmacokinetic and pharmacodynamic properties and improving delivery methods, while variations in the insulin sensitivity of peripheral tissues has received relatively little attention. Notably, tissue insulin sensitivity has been shown to vary considerably around the clock, which could contribute greatly to the effect (and risk of side effects) of a given dose of insulin. Recent evidence suggests that photic inputs regulate diurnal variations in the insulin sensitivity of metabolically relevant tissues via a previously unrecognised mechanism involving the ventromedial hypothalamic nucleus. Therefore, understanding the mechanisms underlying photic control of insulin action is of paramount medical importance. In [...] Reference URSINO, Gloria, COPPARI, Roberto. Insulin under the influence of light. Swiss Medical Weekly, 2020, vol. 150, p. w20273 DOI : 10.4414/smw.2020.20273 PMID : 32564344 Available at: http://archive-ouverte.unige.ch/unige:138000 Disclaimer: layout of this document may differ from the published version. 1 / 1 Review article: Biomedical intelligence | Published 17 June 2020 | doi:10.4414.smw.2020.20273 Cite this as: Swiss Med Wkly. 2020;150:w20273 Insulin under the influence of light Ursino Gloriaab, Coppari Robertoab a Department of Cell Physiology and Metabolism, University of Geneva, Switzerland b Diabetes Centre of the Faculty of Medicine, University of Geneva, Switzerland Summary islet and the tight regulation of insulin output [4–6].