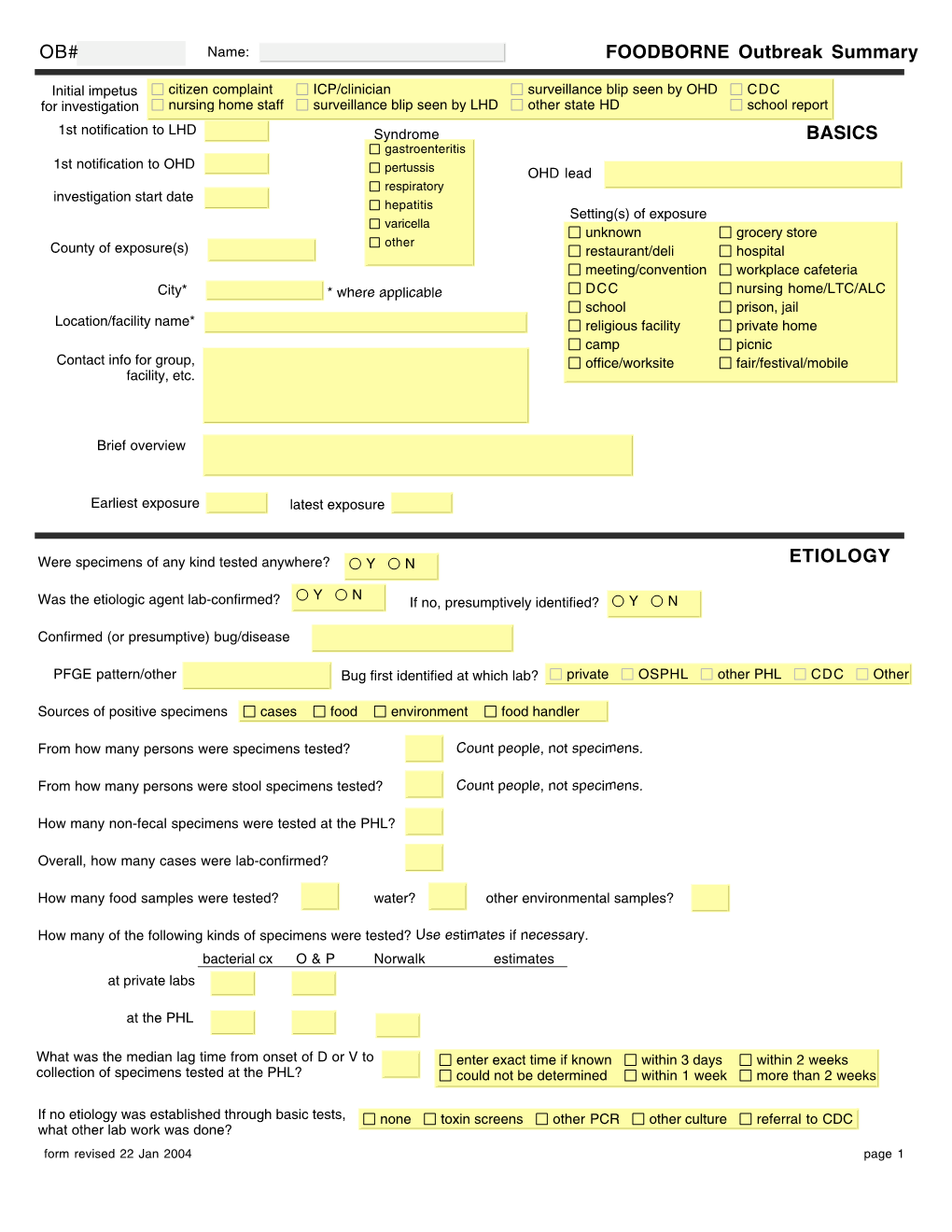
OB# FOODBORNE Outbreak Summary BASICS ETIOLOGY CASES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Journ. of Intell Prop 7- October, 2013.Pmd
133 Journal of Intellectual Property. Companies and Intellectual Property Office Dominica VOL. 4 ROSEAU, THURSDAY, OCTOBER 10, 2013 NO. 7 Applications for Trademark Registration ANSA MCAL CHEMICALS LIMITED, a limited liability ANSA MCAL CHEMICALS LIMITED, a limited liability company organized and existing under the laws of company organized and existing under the laws of TRINIDAD AND TOBAGO of NORTH SEA DRIVE, POINT LISAS IN- TRINIDAD AND TOBAGO of NORTH SEA DRIVE, POINT LISAS IN- DUSTRIAL ESTATE, SAVONETTA, TRINIDAD AND TOBAGO has ap- DUSTRIAL ESTATE, SAVONETTA, TRINIDAD AND TOBAGO has ap- plied through their agent, DE FREITAS, DE FREITAS & plied through their agent, DE FREITAS, DE FREITAS & JOHNSON of CHAMBER, 14 CORK STREET, ROSEAU to the JOHNSON of CHAMBER, 14 CORK STREET, ROSEAU to the Companies and Intellectual Property Office for the regis- Companies and Intellectual Property Office for the regis- tration of one trade mark consisting of the following word tration of one trade mark consisting of the following word th and device, based on an application received on the 08th and device, based on an application received on the 08 day of January, 2013. day of January, 2013. in Class 3 that is to say: Bleaching preparations and other substances for laundry use; cleaning, polishing, scouring and abrasive (cleaning) preparations; soaps; perfumery, in Class 3 that is to say: Bleaching preparations and other essential oils, cosmetics, hair lotions; dentifrices. substances for laundry use; cleaning, polishing, scouring and abrasive (cleaning) preparations; soaps; perfumery, No claim is made to the words “Bleach”, “Cloro” and essential oils, cosmetics, hair lotions; dentifrices. “Liquido’. -

Journal-Notice-July
Vol. 16 - No. 15 Belmopan, July 29, 2016 1 INTELLECTUAL PROPERTY JOURNAL BELIZE INTELLECTUAL PROPERTYO OFFICE BEL P Vol. 16 - No. 15 Belmopan, July 29, 2016 2 BELIPO’S MISSION STATEMENT “To build a modern intellectual property system that values and protects the vibrant creative culture of Belize” Vol. 16 - No. 15 Belmopan, July 29, 2016 3 CONTENTS Page Numbers TRADEMARKS: APPLICATIONS FOR TRADEMARK REGISTRATION ………………….………………………………………………… 4 - 70 NOTICES OF TRADEMARK RENEWAL ………………………………….……………………………………………….... 71 - 94 NOTICES OF ASSIGNMENT……………………………………………………………………………………………….… 95 - 97 NOTICES OF CHANGE OF ADDRESS OF PROPRIETOR………………………………………………………………….. 98 - 99 NOTICES OF CHANGE OF NAME OF PROPRIETOR………………………………………………………………………. 100 NOTICES OF RECORDAL OF AGENT AND ADDRESS FOR SERVICE………………………………………………….. 101-107 NOTICES OF PUBLICATION CORRECTION……………………………………………………………………………….. 108 NOTICES OF TRADEMARK REGISTRATIONS………………………………………………………………….….….… .. 109-111 PATENTS: NOTICES OF PATENT GRANT……………………………………………………………………………………………… 112 NOTE: CFE - International Classification of the Figurative Elements of Marks under the Vienna Agreement (Sixth Edition) __________ …________ Vol. 16 - No. 15 Belmopan, July 29, 2016 4 APPLICATIONS FOR TRADEMARK REGISTRATION (3rd issue) WHEREAS, the Registrar is in receipt of an application filed on the 22nd day of April, 2015, by Whirlpool Properties, Inc., of 500 Renaissance Drive, Suite 101, Saint Joseph, Michigan, USA 49085, through its agent Glenn D. Godfrey & Company LLP, Attorneys-at- Law, of No. 35 Barrack -

Carbonated Dairy Beverages: Challenges and Opportunities
beverages Review Carbonated Dairy Beverages: Challenges and Opportunities Daniel Newbold and Kadri Koppel * Center for Sensory Analysis and Consumer Behavior, Kansas State University, 1310 Research Park Dr, Manhattan, KS 66502, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-785-532-0163 Received: 25 July 2018; Accepted: 28 August 2018; Published: 2 September 2018 Abstract: Yogurt drinks have seen a 66% increase in consumption in the United States over the last five years. Even though there has been an increase in yogurt drink consumption, the market share of drinkable dairy beverages remains small. Carbonated dairy beverages have become increasingly popular in recent years, and innovations in this area could help drive increased consumption of these beverages. Currently traditionally carbonated dairy beverages, like kefir, are the most popular carbonated dairy beverages on the market. Carbonation at appropriate levels in dairy products, especially dairy beverages, has been shown to improve the sensory attributes, quality, and shelf life of these products. Probiotics, which are added to yogurt drinks for their health benefits, are not harmed or negatively affected by carbonation. Several methods have been developed to carbonate dairy beverages in a manufacturing setting, although these methods have not been widely applied to commercially available products. The increased consumption of dairy beverages and the benefits of carbonation upon these beverages means that there are opportunities to develop widely accepted and popular carbonated dairy beverages. The objective of this article was to review available literature on carbonated dairy beverages and to discuss the challenges and opportunities in this area. Keywords: Carbonation; dairy; drinkable yogurt; carbonated yogurt; carbonated beverage 1. -

Culture-Independent Bacterial Community Profiling of Carbon Dioxide Treated Raw Milk
ÔØ ÅÒÙ×Ö ÔØ Culture-independent bacterial community profiling of carbon dioxide treated raw milk Raquel Lo, Mark S. Turner, Mike Weeks, Nidhi Bansal PII: S0168-1605(16)30308-7 DOI: doi: 10.1016/j.ijfoodmicro.2016.06.015 Reference: FOOD 7262 To appear in: International Journal of Food Microbiology Received date: 1 March 2016 Revised date: 30 May 2016 Accepted date: 14 June 2016 Please cite this article as: Lo, Raquel, Turner, Mark S., Weeks, Mike, Bansal, Nidhi, Culture-independent bacterial community profiling of carbon dioxide treated raw milk, International Journal of Food Microbiology (2016), doi: 10.1016/j.ijfoodmicro.2016.06.015 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT Culture-independent bacterial community profiling of carbon dioxide treated raw milk Raquel Lo a, Mark S. Turner a,c, Mike Weeksb, Nidhi Bansal a,* a School of Agriculture and Food Sciences, The University of Queensland, St Lucia, QLD 4072, Australia b Dairy Innovation Australia, Werribee, VIC 3030, Australia c Queensland Alliance for Agriculture and Food Innovation, The University of Queensland, St Lucia, QLD 4072, Australia *Corresponding author. Tel.: +61 7 33651673. E-mail address: [email protected] (N. -
全文本) Acceptance for Registration (Full Version)
公報編號 Journal No.: 395 公布日期 Publication Date: 29-10-2010 分項名稱 Section Name: 接納註冊 (全文本) Acceptance for Registration (Full Version) 香港特別行政區政府知識產權署商標註冊處 Trade Marks Registry, Intellectual Property Department The Government of the Hong Kong Special Administrative Region 接納註冊 (全文本) 商標註冊處處長已根據《商標條例》(第 559 章)第 42 條,接納下列商標的註冊申請。現根據《商標條 例》第 43 條及《商標規則》(第 559 章附屬法例)第 15 條,公布申請的詳情。 根據《商標條例》第 44 條及《商標規則》第 16 條,任何人擬就下列商標的註冊提出反對,須在本公告 公布日期起計的三個月內,採用表格第 T6 號提交反對通知。(例如,若果公布日期爲 2003 年 4 月 4 日,則該三個月的最後一日爲 2003 年 7 月 3 日。)反對通知須載有反對理由的陳述及《商標規則》第 16(2)條所提述的事宜。反對人須在提交反對通知的同時,將該通知的副本送交有關申請人。 有關商標註冊處處長根據商標條例(第 43 章)第 13 條/商標條例(第 559 章)附表 5 第 10 條所接納的註冊申 請,請到 http://www.gld.gov.hk/cgi-bin/gld/egazette/index.cgi?lang=c&agree=0 檢視電子憲報。 ACCEPTANCE FOR REGISTRATION (FULL VERSION) The Registrar of Trade Marks has accepted the following trade marks for registration under section 42 of the Trade Marks Ordinance (Cap. 559). Under section 43 of the Trade Marks Ordinance and rule 15 of the Trade Marks Rules (Cap. 559 sub. leg.), the particulars of the applications are published. Under section 44 of the Trade Marks Ordinance and rule 16 of the Trade Marks Rules, any person who wishes to oppose the registration of any of these marks shall, within the 3-month period beginning on the date of this publication, file a notice of opposition on Form T6. (For example, if the publication date is 4 April 2003, the last day of the 3-month period is 3 July 2003.) The notice of opposition shall include a statement of the grounds of opposition and the matters referred to in rule 16(2). -
Carbonation and Its Interaction with Other Sensory Modalities
AN ABSTRACT OF THE THESIS OF Niann-Jou Newton. Yau 'for the degree of Doctor of Philosophy in Food Science and Technology presentedon August 27. 1991. Title: Carbonation and Its Interaction with Other Sensory Modalities Signature redacted for privacy. Abstract approved: rof. Mina R. McDaniel The study of carbonation perception is limited, even though carbonated beverages are very popular. A series of experiments were conducted to determine the sensory properties of carbonation itself and its interaction with other sensory modalities. First, the power functions of carbonation in carbonated spring water were developed by a trained panel using two assessing conditions, swallowing and expectoration. Five carbonation levels, 1.2 2.0. 2.5, 3.0, and 3.9 volumes CO2, were employed. The size of the exponents, 2.79 (swallowing) and 2.65 (expectoration), suggested a sharp increase of perceived carbonation magnitude with increasing concentration. There was no significant difference between exponents resulting from the two assessing conditions. Second, the effects of temperature on carbonation perception in carbonated spring water were determined by use of both a trained panel and a naive panel. Two carbonation levels, 2.4 and 3.0 volumes, and four temperature levels, 30, 10°, 160 and 220C, were employed. Carbonation intensity was perceived to be higher at lower temperatures than at higher temperatures. This effect held true for both trained and naive panels. The temperature effect on carbonation perception, however, was carbonation level dependent. Differences were more evident at the higher carbonation level. Thirdly, the mutual effects of carbonation and tastants (sweetener and acidulant) were determined by a trained panel. -

The Antioxidative Capacity of Kefir Produced from Goat Milk
International Journal of Chemical Engineering and Applications, Vol. 7, No. 1, February 2016 The Antioxidative Capacity of Kefir Produced from Goat Milk Lutfiye Yilmaz-Ersan, Tulay Ozcan, Arzu Akpinar-Bayizit, and Saliha Sahin lightly yellow in colour, and look like tiny clumps of Abstract—In this present study, the antioxidant properties cauliflower varying in size from 1 to 6 mm in diameter of kefir produced from goat milk with kefir grains were (0.3–3.5 cm). The function of the microorganisms of the investigated. The antioxidant capacity of kefir was evaluated kefir grains during fermentation may include the production by assessing the DPPH (2,2-Diphenyl-1-picrylhydrazyl), the of lactic acid, natural antibiotics, all of which are able to ABTS-based method [2,2’-azino-bis-(3-ethylbenzthiazoline-6- sulphonic acid)] radical-scavenging activity and ferric inhibit the growth of undesirable and pathogenic reducing antioxidant power (FRAP) at different stages of microorganisms in kefir milk. However, kefir has a uniform fermentation and storage period. Generally, the antioxidant creamy consistency with acidic, yeasty flavor, a low alcohol capacity of goat milk-kefir samples was mainly dependent on content and contains vitamins (vitamin B1, B12, K and folic the fermentation and storage period and good stability in acid), minerals, amino acids, easily digestible complete DPPH, ABTS and FRAPS assays. During fermentation and proteins, and a variety of aromatic substances, such as storage, the total phenolic content in samples demonstrated significantly decreased. acetaldehyde, acetoin, and diacetyl that give it its characteristic flavor [5], [6]. Index Terms—Kefir, goat milk, antioxidant. Kefir has long being considered beneficial to human health. -

Development of Chocolate-Flavored, Peanut-Soy Beverage
DEVELOPMENT OF CHOCOLATE-FLAVORED, PEANUT-SOY BEVERAGE by RASHMI PRAKASH DESHPANDE (Under the Direction of Manjeet Singh Chinnan) ABSTRACT A novel formulation and pilot-plant scale processing protocol was developed for a protein-based, nutritious beverage. Roasted peanut and chocolate flavors were utilized to enhance acceptability and soy flour or soy protein isolate to improve nutritional profile. Extreme vertices, constrained- mixture design for peanut (X1:30.56%-58.70%), soy (X2:28.26%-43.52%), and chocolate syrup (X3:13.04%-25.93%) yielded 28 formulations for sensory evaluation. Commercial chocolate milk was used as a control. Optimization of sensory data was done using response surface methodology. Since control ratings were 6-7, the regions of maximum consumer acceptability for each sensory attribute were ratings ≥ 5.0. Optimum formulations for soy flour were all combinations of 34.1%-45.5% X1, 31.2%-42.9% X2, and 22.4%-24.1% X3; and for soy protein isolate 35.8%-47.6% X1, 31.2%-43.5% X2, and 18.3%-23.6% X3. A formulation with 43.9% peanut, 36.3% soy protein isolate, and 19.8% chocolate syrup had the highest consumer acceptability. Soy protein isolate performed better than soy flour and gave beverage characteristics closer to that of control. INDEX WORDS: Chocolate-flavored, peanut-soy beverage, Soy flour, Soy protein isolate, Extreme vertices constrained mixture design, Sensory evaluation, Response surface methodology (RSM), Consumer acceptability DEVELOPMENT OF CHOCOLATE-FLAVORED, PEANUT-SOY BEVERAGE by RASHMI PRAKASH DESHPANDE B. Tech., Laxminarayan Institute of Technology, Nagpur University, India, 1999 A Thesis Submitted to the Graduate Faculty of The University of Georgia in Partial Fulfillment of the Requirements for the Degree MASTER OF SCIENCE ATHENS, GEORGIA 2004 © 2004 Rashmi Prakash Deshpande All Rights Reserved DEVELOPMENT OF CHOCOLATE-FLAVORED, PEANUT-SOY BEVERAGE by RASHMI PRAKASH DESHPANDE Major Professor: Manjeet S. -
全文本) Acceptance for Registration (Full Version)
公報編號 Journal No.: 179 公布日期 Publication Date: 08-09-2006 分項名稱 Section Name: 接納註冊 (全文本) Acceptance for Registration (Full Version) 香港特別行政區政府知識產權署商標註冊處 Trade Marks Registry, Intellectual Property Department The Government of the Hong Kong Special Administrative Region 接納註冊 (全文本) 商標註冊處處長已根據《商標條例》(第 559 章)第 42 條,接納下列商標的註冊申請。現根據《商標條 例》第 43 條及《商標規則》(第 559 章附屬法例)第 15 條,公布申請的詳情。 根據《商標條例》第 44 條及《商標規則》第 16 條,任何人擬就下列商標的註冊提出反對,須在本公告 公布日期起計的三個月內,採用表格第 T6 號提交反對通知。(例如,若果公布日期爲 2003年4月4 日,則該三個月的最後一日爲 2003 年 7 月 3 日。)反對通知須載有反對理由的陳述及《商標規則》第 16(2)條所提述的事宜。反對人須在提交反對通知的同時,將該通知的副本送交有關申請人。 有關商標註冊處處長根據商標條例(第 43 章)第 13 條/商標條例(第 559 章)附表 5 第 10 條所接納的註冊申 請,請到 http://www.info.gov.hk/pd/egazette/檢視電子憲報。 ACCEPTANCE FOR REGISTRATION (FULL VERSION) The Registrar of Trade Marks has accepted the following trade marks for registration under section 42 of the Trade Marks Ordinance (Cap. 559). Under section 43 of the Tr ade Marks Ordinance and rule 15 of the Trade Marks Rules (Cap. 559 sub. leg.), the particulars of the applications are published. Under section 44 of the Trade Marks Ordinance and rule 16 of the Trade Marks Rules, any person who wishes to oppose the registration of any of these marks shall, w ithin the 3-month period beginning on the date of this publication, file a notice of opposition on For m T6. (For example, if the publication date is 4 April 2003, the last day of the 3-month period is 3 July 2003.) The notice of opposition shall include a statement of the grounds of opposition and the matters referred to in rule 16(2). -

WO 2007/027926 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (43) International Publication Date (10) International Publication Number 8 March 2007 (08.03.2007) PCT WO 2007/027926 Al (51) International Patent Classification: (72) Inventor; and A23C 19/032 (2006 01) (75) Inventor/Applicant (for US only): BARBANO, David M. [US/US], 54 W Main St , Dryden, New York 13053 (21) International Application Number: (US) PCT/US2006/034081 (74) Agents: CLISE, Timothy B. et al , Schwegman Lundberg (22) International Filing Date: 30 August 2006 (30 08 2006) Woessner & Kluth, PA, P O Box 2938, Minneapolis, MN 55402 (US) (25) Filing Language: English (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, (26) Publication Language: English AT,AU, AZ, BA, BB, BG, BR, BW, BY, BZ, CA, CH, CN, CO, CR, CU, CZ, DE, DK, DM, DZ, EC, EE, EG, ES, FI, (30) Priority Data: GB, GD, GE, GH, GM, HN, HR, HU, ID, IL, IN, IS, JP, 60/712,621 30 August 2005 (30 08 2005) US KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, 60/775,049 20 February 2006 (20 02 2006) US LU, LV,LY,MA, MD, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PG, PH, PL, PT, RO, RS, RU, (71) Applicant (for all designated States except US): COR¬ SC, SD, SE, SG, SK, SL, SM, SV, SY, TJ, TM, TN, TR, NELL RESEARCH FOUNDATION, INC. [US/US], 20 TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW Thornwood Dπve, Suite 105, Ithaca, NY 14850 (US) (84) Designated States -

Marks Published for Opposition
MARKS PUBLISHED FOR OPPOSITION The following marks are published in compliance with section 12(a) of the Trademark Act of 1946. Applications for the registration of marks in more than one class have been filed as provided in section 30 of said act as amended by Public Law 772, 87th Congress, approved Oct. 9, 1962, 76 Stat. 769. Opposition under section 13 may be filed within thirty days of the date of this publication. See rules 2.101 to 2.105. A separate fee of two hundred dollars for opposing each mark in each class must accompany the opposition. SECTION 1.— INTERNATIONAL CLASSIFICATION The short titles associated below with the international class numbers are terms designed merely for quick identification and are not an official part of the international classification. The full names of international classes are given in section 6.1 of the trademark rules of practice. The designation ‘‘U.S. Cl.’’ appearing in this section refers to the U.S. class in effect prior to Sep. 1, 1973 rather than the international class which applies to applications filed on or after that date. For adoption of international classification see notice in the OFFICIAL GAZETTE of Jun. 26, 1973 (911 O.G. TM 210). Application in more than one class SN 75-033,008. ONTARIO PAINT & WALLPAPER LIMITED, CLASS 9—ELECTRICAL AND SCIENTIFIC CONCORD, ONTARIO, L4K 3S8, CANADA, FILED 12-15- 1995. APPARATUS FOR PUMPS, POWER GENERATORS, GEARS, PISTON RINGS, COMPRESSORS, CONDENSERS, CLUTCHES, BALL BEARINGS, BEARING BLOCKS, PUMP DIA- PHRAGMS, ALL FOR GAS, AIR AND FLUID MEASUR- ING INSTRUMENTS FOR MEASURING AND/OR EPISODES ANALYZING PHYSICAL AND/OR CHEMICAL QUAN- TITIES, NAMELY, LIGHT, PRESSURE, SPEED, FLOW- THROUGH, ACCELERATION, TEMPERATURE, MOIST- URE, GASES, GAS CONCENTRATIONS AND GAS COMPOSITIONS, SENSORS FOR DETECTING AND/OR ANALYZING PHYSICAL AND/OR CHEMICAL QUAN- PRIORITY CLAIMED UNDER SEC. -

Smit-Prelims 1..4
Index @RISK 120, 121–4 bacteria abnormal milk 283–4 ADMI turbidimetric test 220 Accelase 424 adsorption 374 acceleration of cheese ripening 419–47 adulteration see authenticity testing adjunct cultures 431–3 AEDA technique 142–3 elevated temperature 421–2 affinity chromatography 374 EMCs as flavouring 437–40 aflatoxins 293, 294–9, 300 exogenous enzymes or attenuated aflatoxin B1 294–5 starters 422–31 aflatoxin M1 293, 295–9, 300 future trends 440–1 agglomeration 341–4, 345, 351–3 genetic modification of starter bacteria aggregation 188 433–4 albumins 19 high pressure 322–4, 434–6 see also -lactalbumin acetaldehyde 142, 144, 503 alcohols 494, 496, 497 acetate 461 aldehydes 132, 140, 494, 496, 497, 502 acetic acid 10 alkaline phosphatase (AP) 86, 115–16, acid-curd cheeses 470, 471, 472, 473, 122, 315 475, 489 safety of milk 293, 301–2 cultures for 484–7 test for pasteurisation 110 surface microflora 476, 477 1-acid glycoprotein 26, 32 acid phosphatase 33 -keto acids 496, 497, 501–3 acidification 188 -lactalbumin ( -La) 19, 20, 21, 22, 367 acidity/pH 143, 317–18, 398–9 effects of high pressure 312–13, 317 Actimel 235 separation 379–81 added-value products 233 yoghurt 163–4 adhesion Amadori compounds 301, 305–6 prevention of adhesion of pathogens amino acid catabolic enzymes 434 247–8 amino acids 384, 421 of probiotics to epithelial cell lines degradation of proteins 132–3 249–50 flavour formation in cheese 492–511 adjunct cultures see non-starter lactic acid biosynthesis and requirements 495–6 Index 533 branched-chain and aromatic amino bacteria