Innate Host Resistance
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Influence of Infection and Inflammation on Biomarkers of Nutritional Status
A2.4 INFLUENCE OF INFECTION AND INFLAMMATION ON BIOMARKERS OF NUTRITIONAL STATUS A2.4 Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron David I. Thurnham1 and George P. McCabe2 1 Northern Ireland Centre for Food and Health, University of Ulster, Coleraine, United Kingdom of Great Britain and Northern Ireland 2 Statistics Department, Purdue University, West Lafayette, Indiana, United States of America Corresponding author: David I. Thurnham; [email protected] Suggested citation: Thurnham DI, McCabe GP. Influence of infection and inflammation on biomarkers of nutritional status with an emphasis on vitamin A and iron. In: World Health Organization. Report: Priorities in the assessment of vitamin A and iron status in populations, Panama City, Panama, 15–17 September 2010. Geneva, World Health Organization, 2012. Abstract n Many plasma nutrients are influenced by infection or tissue damage. These effects may be passive and the result of changes in blood volume and capillary permeability. They may also be the direct effect of metabolic alterations that depress or increase the concentration of a nutrient or metabolite in the plasma. Where the nutrient or metabolite is a nutritional biomarker as in the case of plasma retinol, a depression in retinol concentrations will result in an overestimate of vitamin A deficiency. In contrast, where the biomarker is increased due to infection as in the case of plasma ferritin concentrations, inflammation will result in an underestimate of iron deficiency. Infection and tissue damage can be recognized by their clinical effects on the body but, unfortunately, subclinical infection or inflammation can only be recognized by measur- ing inflammation biomarkers in the blood. -

The Gut Microbiota and Inflammation
International Journal of Environmental Research and Public Health Review The Gut Microbiota and Inflammation: An Overview 1, 2 1, 1, , Zahraa Al Bander *, Marloes Dekker Nitert , Aya Mousa y and Negar Naderpoor * y 1 Monash Centre for Health Research and Implementation, School of Public Health and Preventive Medicine, Monash University, Melbourne 3168, Australia; [email protected] 2 School of Chemistry and Molecular Biosciences, The University of Queensland, Brisbane 4072, Australia; [email protected] * Correspondence: [email protected] (Z.A.B.); [email protected] (N.N.); Tel.: +61-38-572-2896 (N.N.) These authors contributed equally to this work. y Received: 10 September 2020; Accepted: 15 October 2020; Published: 19 October 2020 Abstract: The gut microbiota encompasses a diverse community of bacteria that carry out various functions influencing the overall health of the host. These comprise nutrient metabolism, immune system regulation and natural defence against infection. The presence of certain bacteria is associated with inflammatory molecules that may bring about inflammation in various body tissues. Inflammation underlies many chronic multisystem conditions including obesity, atherosclerosis, type 2 diabetes mellitus and inflammatory bowel disease. Inflammation may be triggered by structural components of the bacteria which can result in a cascade of inflammatory pathways involving interleukins and other cytokines. Similarly, by-products of metabolic processes in bacteria, including some short-chain fatty acids, can play a role in inhibiting inflammatory processes. In this review, we aimed to provide an overview of the relationship between the gut microbiota and inflammatory molecules and to highlight relevant knowledge gaps in this field. -

Regulation of Macrophage Development and Function in Peripheral Tissues
REVIEWS Regulation of macrophage development and function in peripheral tissues Yonit Lavin, Arthur Mortha, Adeeb Rahman and Miriam Merad Abstract | Macrophages are immune cells of haematopoietic origin that provide crucial innate immune defence and have tissue-specific functions in the regulation and maintenance of organ homeostasis. Recent studies of macrophage ontogeny, as well as transcriptional and epigenetic identity, have started to reveal the decisive role of the tissue stroma in the regulation of macrophage function. These findings suggest that most macrophages seed the tissues during embryonic development and functionally specialize in response to cytokines and metabolites that are released by the stroma and drive the expression of unique transcription factors. In this Review, we discuss how recent insights into macrophage ontogeny and macrophage–stroma interactions contribute to our understanding of the crosstalk that shapes macrophage function and the maintenance of organ integrity. Mononuclear phagocyte Macrophages are key components of the innate immune characterized the transcriptional and epigenetic pro- system system that reside in tissues, where they function as grammes of tissue-resident macrophages and revealed (MPS). A group of bone immune sentinels. They are uniquely equipped to sense the extent of diversity in these populations1,8. In addi- marrow-derived cells and respond to tissue invasion by infectious microorgan- tion to differences in ontogeny, locally derived tissue (monocytes, macrophages and isms and tissue -

A Single Wave of Monocytes Is Sufficient to Replenish the Long-Term
bioRxiv preprint doi: https://doi.org/10.1101/617514; this version posted April 24, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. A single wave of monocytes is sufficient to replenish the long-term Langerhans cell network after immune injury Ivana R. Ferrer1,2,a, Heather C. West1,2,a, Stephen Henderson2, Dmitry S. Ushakov3, Pedro Santos e Sousa1,2, Jessica Strid4, Ronjon Chakraverty1,2, Andrew J. Yates5, and Clare L. Bennett1,2 1Institute of Immunity and Transplantation, Division of Infection and Immunity, University College London, London NW3 2PF, UK 2Haematology, Division of Cancer Studies, University College London, London WC1E 6DD, UK. 3Peter Gorer Department of Immunobiology, School of Immunology and Microbial Sciences, King’s College London, New Hunt’s House, Newcomen St, London SE1 1UL, UK 4Division of Immunology and Inflammation, Imperial College London, Hammersmith campus, London W12 0NN, UK. 5Department of Pathology and Cell Biology, Columbia University Medical Center, New York, NY10032, USA. aThese authors contributed equally to this work Abstract • Immune injury and inefficient repopulation by Embryo-derived Langerhans cells (eLC) are maintained within monocyte-derived cells lead to a permanently altered the sealed epidermis without contribution from circulating cells. LC niche. When the network is perturbed by transient exposure to ultra- violet light, short-term LC are temporarily reconstituted from an initial wave of monocytes, but thought to be superseded by more permanent repopulation with undefined LC precur- sors. However, the extent to which this mechanism is relevant to immune-pathological processes that damage LC population integrity is not known. -

Progress in Understanding the Pathogenesis of Langerhans Cell Histiocytosis: Back to Histiocytosis X?
review Progress in understanding the pathogenesis of Langerhans cell histiocytosis: back to Histiocytosis X? Marie-Luise Berres,1,2,3,4 Miriam Merad1,2,3 and Carl E. Allen5,6 1Department of Oncological Sciences, Mount Sinai School of Medicine, 2Tisch Cancer Institute, Mount Sinai School of Medicine, 3Immunology Institute, Mount Sinai School of Medicine, New York, NY, USA, 4Department of Internal Medicine III, University Hospital, RWTH Aachen, Aachen, Germany, 5Texas Children’s Cancer Center, and 6Baylor College of Medicine, Houston, TX, USA Summary Langerhans cell histiocytosis (LCH) is the most common his- tiocytic disorder, arising in approximately five children per Langerhans cell histiocytosis (LCH), the most common million, similar in frequency to paediatric Hodgkin lym- histiocytic disorder, is characterized by the accumulation of phoma and acute myeloid leukaemia (AML) (Guyot-Goubin CD1A+/CD207+ mononuclear phagocytes within granuloma- et al, 2008; Stalemark et al, 2008; Salotti et al, 2009). The tous lesions that can affect nearly all organ systems. Histori- median age of presentation is 30 months, though LCH is cally, LCH has been presumed to arise from transformed or reported in adults in approximately one adult per million, pathologically activated epidermal dendritic cells called Lan- both as unrecognized chronic paediatric disease and de novo gerhans cells. However, new evidence supports a model in disease (Baumgartner et al, 1997). There are occasional which LCH occurs as a consequence of a misguided differen- reports of affected non-twin siblings and multiple cases in tiation programme of myeloid dendritic cell precursors. one family, though it is not clear if this is significantly more Genetic, molecular and functional data implicate activation frequent than one would expect by chance (Arico et al, of the ERK signalling pathway at critical stages in myeloid 2005). -

Innate Immunity and Inflammation
ISBTc ‐ Primer on Tumor Immunology and Biological Therapy of Cancer InnateInnate ImmunityImmunity andand InflammationInflammation WillemWillem Overwijk,Overwijk, Ph.D.Ph.D. MDMD AndersonAnderson CancerCancer CenterCenter CenterCenter forfor CancerCancer ImmunologyImmunology ResearchResearch Houston,Houston, TXTX www.allthingsbeautiful.com InnateInnate ImmunityImmunity andand InflammationInflammation • Definitions • Cells and Molecules • Innate Immunity and Inflammation in Cancer • Bad Inflammation • Good Inflammation • Therapeutic Implications InnateInnate ImmunityImmunity andand InflammationInflammation • Definitions • Cells and Molecules • Innate Immunity and Inflammation in Cancer • Bad Inflammation • Good Inflammation • Therapeutic Implications • Innate Immunity: Immunity that is naturally present and is not due to prior sensitization to an antigen; generally nonspecific. It is in contrast to acquired/adaptive immunity. Adapted from Merriam‐Webster Medical Dictionary • Innate Immunity: Immunity that is naturally present and is not due to prior sensitization to an antigen; generally nonspecific. It is in contrast to acquired/adaptive immunity. • Inflammation: a local response to tissue injury – Rubor (redness) – Calor (heat) – Dolor (pain) – Tumor (swelling) Adapted from Merriam‐Webster Medical Dictionary ““InnateInnate ImmunityImmunity”” andand ““InflammationInflammation”” areare vaguevague termsterms •• SpecificSpecific cellcell typestypes andand moleculesmolecules orchestrateorchestrate specificspecific typestypes ofof inflammationinflammation -

Epidermal Macrophage Induction, and Langerhans Cell Depletion (Photoimmunology/Ozone Depletion/Contact Sensitivity/T Lymphocytes/Antigen Presenting Cells) K
Proc. Nati. Acad. Sci. USA Vol. 89, pp. 8497-8501, September 1992 Immunology UV exposure reduces immunization rates and promotes tolerance to epicutaneous antigens in humans: Relationship to dose, CDla-DR+ epidermal macrophage induction, and Langerhans cell depletion (photoimmunology/ozone depletion/contact sensitivity/T lymphocytes/antigen presenting cells) K. D. COOPER*t*, L. OBERHELMAN*, T. A. HAMILTON*, 0. BAADSGAARD*§, M. TERHUNE*, G. LEVEE*, T. ANDERSON*t, AND H. KOREN¶ *Immunodermatology Unit, Department of Dermatology, University of Michigan, Ann Arbor, MI 48109; tVeterans Administration Hospital, Ann Arbor, MI 48105; and 'Health Effects Research Labs, Environmental Protection Agency, Chapel Hill, NC 27711 Communicated by Thomas M. Donahue, May 1, 1992 ABSTRACT Increasing UVB radiation at the earth's sur- tibility of UV-exposed mice and the unresponsiveness of face might have adverse effects on in vivo immunologic responses UV-exposed mice to contact allergens were found to be due in humans. We prospectively randomized subjects to test to antigen-specific suppressor T lymphocytes (12, 13). whether epicutaneous immunization is altered by prior admin- UV regulation of murine contact sensitivity has held up istration of biologically equalized doses of UV radiation. Mul- well as a model of immunologic events occurring in photo- tiple doses of antigens on upper inner arm skin (UV protected) carcinogenesis. Epidermal Langerhans cells, an antigen pre- were used to elicit contact sensitivity responses, which were senting population of dendritic cell lineage present in the quantitated by measuring increases in skin thickness. If a dose epidermis (14), have a potent capacity to initiate contact of UVB sufficient to induce redness (erythemagenic) was ad- sensitivity reactions (15, 16), as well as tumor rejection (17). -

Langerhans Cell Langhans Cell
1 Q Ocular-Surface Immunology The names of these two cell types are easily confused—what are they? This one is: --A type of dendritic cell residing in the ocular surface epithelium --An antigen-presenting cell (APC) --Described as the ‘immune sentinels of the ocular surface’ Langerhans cell This one is: --A type of giant cell found in granulomas --Associated with TB --Horseshoe-like arrangement of nuclei Langhans cell 2 A Ocular-Surface Immunology The names of these two cell types are easily confused—what are they? This one is: --A type of dendritic cell residing in the ocular surface epithelium --An antigen-presenting cell (APC) --Described as the ‘immune sentinels of the ocular surface’ Langerhans cell This one is: --A type of giant cell found in granulomas --Associated with TB --Horseshoe-like arrangement of nuclei Langhans cell 3 Ocular-Surface Immunology The names of these two cell types are easily confused—what are they? This one is: --A type of dendritic cell residing in the ocular surface epithelium --An antigen-presenting cell (APC) --Described as the ‘immune sentinels of the ocular surface’ Langerhans cell The … This one is: ER --A type of giant cell found in granulomas --Associated with TB --Horseshoe-like arrangement of nuclei Langhans cell 4 Ocular-Surface Immunology The names of these two cell types are easily confused—what are they? This one is: --A type of dendritic cell residing in the ocular surface epithelium --An antigen-presenting cell (APC) --Described as the ‘immune sentinels of the ocular surface’ Langerhans cell -

Effect of Exercise Intensity on Cell-Mediated Immunity
sports Perspective Effect of Exercise Intensity on Cell-Mediated Immunity Katsuhiko Suzuki 1,* and Harumi Hayashida 2 1 Faculty of Sport Sciences, Waseda University, 2-579-15 Mikajima, Tokorozawa 359-1192, Japan 2 Faculty of Culture and Sport Policy, Toin University of Yokohama, 1614 Kurogane-cho, Aoba-ku, Yokohama 225-8503, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-4-2947-6898 Abstract: Moderate-intensity exercise is considered to enhance immune function and to be useful for preventing acute upper respiratory infections and similar conditions. Many people practice low- intensity short-duration exercise with the expectation of a beneficial effect on immunocompetency. However, it is difficult to affirm the existence of definite evidence of such a benefit. In this article, we discuss the effects of low-intensity short-duration exercise on cell-mediated immunity, and contrast them to the effects of high-intensity and long-duration exercise. Whereas high-intensity exercise induces inflammation and reduces cell-mediated immune system function, low-intensity exercise does not appear to have a large effect on either inflammation or cell-mediated immune function. Low-intensity exercises such as walking and yoga, which are helpful to relieve stress, cannot be considered as harmful to the immune system. Although yoga was shown to impose fewer restrictions on breathing and physical strain, the evidence that yoga enhances cell-mediated immunity remains insufficient. Therefore, further studies are needed to examine the exercise mode that may be most effective for improvement of immune functions. Keywords: exercise; walking; yoga; cellular immune system; cytokines; inflammation 1. -

An EANM Procedural Guideline
European Journal of Nuclear Medicine and Molecular Imaging https://doi.org/10.1007/s00259-018-4052-x GUIDELINES Clinical indications, image acquisition and data interpretation for white blood cells and anti-granulocyte monoclonal antibody scintigraphy: an EANM procedural guideline A. Signore1 & F. Jamar2 & O. Israel3 & J. Buscombe4 & J. Martin-Comin5 & E. Lazzeri6 Received: 27 April 2018 /Accepted: 6 May 2018 # The Author(s) 2018 Abstract Introduction Radiolabelled autologous white blood cells (WBC) scintigraphy is being standardized all over the world to ensure high quality, specificity and reproducibility. Similarly, in many European countries radiolabelled anti-granulocyte antibodies (anti-G-mAb) are used instead of WBC with high diagnostic accuracy. The EANM Inflammation & Infection Committee is deeply involved in this process of standardization as a primary goal of the group. Aim The main aim of this guideline is to support and promote good clinical practice despite the complex environment of a national health care system with its ethical, economic and legal aspects that must also be taken into consideration. Method After the standardization of the WBC labelling procedure (already published), a group of experts from the EANM Infection & Inflammation Committee developed and validated these guidelines based on published evidences. Results Here we describe image acquisition protocols, image display procedures and image analyses as well as image interpre- tation criteria for the use of radiolabelled WBC and monoclonal antigranulocyte antibodies. Clinical application for WBC and anti-G-mAb scintigraphy is also described. Conclusions These guidelines should be applied by all nuclear medicine centers in favor of a highly reproducible standardized practice. Keywords Infection . -
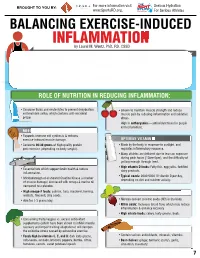
INFLAMMATION MICRONUTRIENTS SOURCES FUNCTION by Laurel M
For more information visit Serious Hydration For more information visit Serious Hydration BROUGHT TO YOU BY: BROUGHT TO YOU BY: For more information visit Serious Hydration www.SportsRD.org. For Serious Athletes www.SportsRD.org. For Serious Athletes www.SportsRD.org. NASA DEVELOPED For Serious Athletes NUTRITIONAL SUPPORT FOR INJURY BALANCING EXERCISE-INDUCED RECOVERY AND RETURN-TO-PLAY INFLAMMATION MICRONUTRIENTS SOURCES FUNCTION by Laurel M. Wentz, PhD, RD, CSSD Vitamin C Citrus fruit, red and green peppers, Antioxidant, wound healing, tissue repair, EXERCISE-INDUCED INFLAMMATION IS THE BODY’S RESPONSE TO INJURY DUE TO INTENSE PHYSICAL ACTIVITY cantaloupe immune function • The immune system response causes redness, swelling, pain. Vitamin A Sweet potato, spinach, carrots, Cell growth and development, • Acute inflammation is a normal response to high-intensity exercise, but prolonged (chronic) tomatoes immune function inflammation is a sustained response that affects the entire body. Vitamin D Sun exposure, oily fish, Promotes calcium absorption and bone health • Prolonged Inflammation: dairy products, fortified foods 1. Causes fatigue, muscle damage and soreness. 2. Limits muscle growth and training progression and increases muscle loss. Calcium Low-fat milk, fortified non-dairy milk, Supports skeletal structure and function 3. Modulating prolonged inflammation may enhance recovery & reduce soreness. low-fat Greek yogurt, cheese, broccoli, kale, fortified orange juice Magnesium Almonds, sesame and sunflower Nucleic acid and protein -

A Role of Inflammation and Immunity in Essential Hypertension—Modeled and Analyzed Using Petri Nets
International Journal of Molecular Sciences Article A Role of Inflammation and Immunity in Essential Hypertension—Modeled and Analyzed Using Petri Nets Dorota Formanowicz 1 , Agnieszka Rybarczyk 2,3 , Marcin Radom 2,3 and Piotr Formanowicz 2,3,* 1 Department of Clinical Biochemistry and Laboratory Medicine, Poznan University of Medical Sciences, 60-806 Poznan, Poland; [email protected] 2 Institute of Computing Science, Poznan University of Technology, 60-965 Poznan, Poland; [email protected] (A.R.); [email protected] (M.R.) 3 Institute of Bioorganic Chemistry, Polish Academy of Sciences, 61-704 Poznan, Poland * Correspondence: [email protected] Received: 15 April 2020; Accepted: 5 May 2020; Published: 9 May 2020 Abstract: Recent studies have shown that the innate and adaptive immune system, together with low-grade inflammation, may play an important role in essential hypertension. In this work, to verify the importance of selected factors for the development of essential hypertension, we created a Petri net-based model and analyzed it. The analysis was based mainly on t-invariants, knockouts of selected fragments of the net and its simulations. The blockade of the renin-angiotensin (RAA) system revealed that the most significant effect on the emergence of essential hypertension has RAA activation. This blockade affects: (1) the formation of angiotensin II, (2) inflammatory process (by influencing C-reactive protein (CRP)), (3) the initiation of blood coagulation, (4) bradykinin generation via the kallikrein-kinin system, (5) activation of lymphocytes in hypertension, (6) the participation of TNF alpha in the activation of the acute phase response, and (7) activation of NADPH oxidase—a key enzyme of oxidative stress.