A Dissertation Entitled Optimally Locating Level I Trauma Centers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Best Hospitals and Practices Own the Bone
OUTSTANDING HOSPITALS DON’T SIMPLY TREAT FRAGILITY FRACTURES – THEY PREVENT FRACTURES FROM RECURRING THE BEST HOSPITALS AND PRACTICES OWN THE BONE The American Orthopaedic Association applauds the following institutions for their achievements and participation in the Own the Bone® quality improvement program: Institutions are recognized for at least 75% compliance on at least 5 of the 10 STAR PERFORMERS recommended secondary fracture prevention measures over the last year. AdventHealth Orlando - Winter Park, FL Lahey Hospital and Medical Center - ^Prisma Health - Upstate - Greenville, SC Allegheny Health Network (AHN) - Burlington, MA ProMedica Toledo Hospital - Toledo, OH Jefferson Hospital - Pittsburgh, PA LewisGale Medical Center - Salem, VA Regions Hospital - Minneapolis, MN Anne Arundel Medical Group Orthopedics and MaineGeneral Orthopaedics - Augusta, ME ^Sanford Medical Center - Fargo - Fargo, ND Sports Medicine Specialists - Annapolis, MD Marshfield Clinic Health System - Marshfield, WI SIH Herrin Hospital - Herrin, IL Ascension Sacred Heart - Pensacola, FL Medical City Healthcare at Arlington - South Texas Fracture Prevention Clinic - Baptist Orthopedic Hospital at Mission Trail - Arlington, TX San Antonio, TX San Antonio, TX Medical University of South Carolina - Southeast Georgia Health System - Berkshire Medical Center - Pittsfield, MA Charleston, SC Brunswick, GA Blue Mountain Hospital - Blanding, UT Memorial Regional Hospital - Hollywood, FL St. Luke's Health System Osteoporosis and Bryan Medical Center - Lincoln, NE Mendelson -

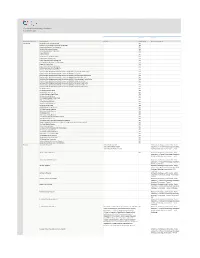
Trauma Centers
Updated: 5/5/2021 TRAUMA CENTERS Location Level EMS Adult Pediatric HOSPITAL CITY COUNTY Status Expires Visit Date Region Level Level Akron Children's Hospital Akron Summit 5 ACS 9/10/2022 2 Atrium Medical Center Franklin Butler 6 ACS 11/6/2022 3 Aultman Hospital Canton Stark 5 ACS 10/24/2021 6/4/2021 V 2 Bethesda North Cincinnati Hamilton 6 ACS 6/9/2022 3 Blanchard Valley Hospital Findlay Hancock 1 ACS 1/15/2024 3 Cincinnati Children's Hospital Medical Center Cincinnati Hamilton 6 ACS 1/23/2022 1 Cleveland Clinic Akron General Akron Summit 5 ACS 4/17/2022 1 Cleveland Clinic Fairview Hospital Cleveland Cuyahoga 2 ACS 3/9/2022 2 Cleveland Clinic Hillcrest Hospital Mayfield Heights Cuyahoga 2 ACS 12/9/2021 2 Dayton Children's Hospital Dayton Montgomery 3 ACS 2/12/2024 1 Firelands Regional Medical Center Sandusky Erie 1 ACS 2/23/2023 3 Fisher-Titus Medical Center Norwalk Huron 1 ACS 11/23/2022 3 Genesis HealthCare System Zanesville Muskingum 8 ACS 10/6/2024 3 Grandview Medical Center Dayton Montgomery 3 ACS 10/26/2022 3 Kettering Health Network Fort Hamilton Hospital Hamilton Butler 6 Ohio-18 8/24/2022 *3* Kettering Health Network Soin Medical Center Beavercreek Greene 3 ACS 11/13/2023 3 Kettering Medical Center Kettering Montgomery 3 ACS 1/11/2023 2 Lima Memorial Hospital Lima Allen 1 ACS 5/13/2021 5/4-5/2021 V 2 Marietta Memorial Hospital Marietta Washington 8 ACS 11/20/2022 3 Mercy Health St. Charles Hospital Toledo Lucas 1 ACS 12/8/2022 3 Mercy Health St. -

An Access to Care Guide in the CASE of ILLNESS OR INJURY
An Access to Care Guide IN THE CASE OF ILLNESS OR INJURY Regardless of your concern, OhioHealth has you covered with the following healthcare options: don’t have Select Find a Doctor at ohiohealth.com or call (614) 4-HEALTH (443.2584) a pcp? to find a primary care physician. It’s the first step to your best health. For allergies, sinus infections, cold and cough, sore throat, earaches, fever, flu-like symptoms, urgent care rashes, and minor burns and other non-life-threatening needs. 1 OHIOHEALTH URGENT CARE — DUBLIN 4 OHIOHEALTH URGENT CARE — GROVE CITY 7 OHIOHEALTH URGENT CARE — 6905 Hospital Drive, Suite 130 2030 Stringtown Road POLARIS (614) 923.0300 (614) 883.0160 1120 Polaris Parkway 9 a.m. – 9 p.m., 7 days a week 9 a.m. – Midnight, 7 days a week (614) 847.1120 9 a.m. – 9 p.m., 7 days a week 2 OHIOHEALTH URGENT CARE — 5 OHIOHEALTH URGENT CARE — HILLIARD GAHANNA/NEW ALBANY 4343 All Seasons Drive, Suite 160 8 OHIOHEALTH URGENT CARE — 5610 Hamilton Road (614) 541.2676 REYNOLDSBURG (614) 775.9870 9 a.m. – 7 p.m., 7 days a week 2014 Baltimore-Reynoldsburg Road 8 a.m. – 8 p.m., 7 days a week (614) 522.6900 OHIOHEALTH URGENT CARE — 6 9 a.m. – 7 p.m., 7 days a week 3 OHIOHEALTH URGENT CARE — LEWIS CENTER GRANDVIEW 24 Hidden Ravines Drive 895 West 3rd Avenue (740) 549.2700 (614) 437.0278 9 a.m. – 7 p.m., 7 days a week 9 a.m. – 7 p.m., 7 days a week For life-threatening conditions such as heart attack and stroke, chest pain, difficulty emergency services breathing, severe bleeding, head injury, loss of consciousness, or other major trauma. -

Ohio PPO 5-13.Indd
HealthLink PPO Hospital Locations – Ohio Participating Hospitals Lake Ashtabula Fulton Toledo Akron General Medical Center (Summit County) Williams Lucas Ottawa Cleveland Arthur James Cancer Institute (Franklin County) Geauga Bay Park Community Hospital (Lucas County) Erie Defiance Wood Sandusky Cuyahoga Bethesda Hospital Inc. (Butler County) Henry Lorain Trumbull Bethesda Hospital Inc. (Hamilton County) Medina Huron Portage Youngstown Children’s Hospital Medical Center (Hamilton County) Paulding Seneca Akron Putnam Children’s Medical Center (Montgomery County) Hancock Summit Cleveland Clinic (Cuyahoga County) Mahoning Van Wert Wyandot Crawford Cleveland Clinic (Summit County) Richland Ashland Wayne Stark Allen Columbiana Deaconess Health Campus (Hamilton County) Hardin Defiance Hospital Regional Medical Center Marion Carroll Auglaize Holmes (Defiance County) Mercer Morrow Tuscarawas Diley Ridge Medical Center (Franklin County) Knox Logan Jefferson Doctors Hospital (Franklin County) Shelby Union Coshocton Harrison Doctors Hospital Of Nelsonville (Athens County) Delaware Dublin Methodist Hospital (Franklin County) Champaign Darke Licking Miami Guernsey Edwin Shaw Rehab (Summit County) Belmont Euclid Hospital (Cuyahoga County) Columbus Muskingum Clark Fairview General Hospital (Cuyahoga County) Madison Montgomery Franklin Firelands Regional Medical Center (Erie County) Preble Fairfield Noble Dayton Perry Monroe Flower Memorial Hospital (Lucas County) Greene Pickaway Morgan Fostoria Community Hospital (Seneca County) Fayette Galion Community -

100 Years. 100 Facts
100 Years. 100 Facts. Celebrating 100 Years as the United Voice of Ohio Hospitals 1819 Daniel Drake obtains a charter for the Medical 001 College of Ohio, the forerunner of the University of Cincinnati College of Medicine. 100 Years. 100 Facts. | 3 1823 Ohio’s first hospital, the Cincinnati Commercial 002 Hospital and Lunatic Asylum, opens. 4 | Ohio Hospital Association 100 Years. 100 Facts. | 5 Starling Medical Center College/Saint 003 Francis Hospital is established on the 1849 present site of Grant Medical Center in Columbus as the first teaching hospital in the U.S. It is the forerunner for the College of Medicine at Ohio State University. 6 | Ohio Hospital Association Charity Hospital Medical Center, now 004 St. Vincent Charity Hospital, opens 1873 Cleveland’s first amphitheater for demonstration of surgery and clinical procedures. 100 Years. 100 Facts. | 7 8 | Ohio Hospital Association 1886 Mother M. Angela and Sister M. Rufina Dunn, of the 005 Congregation of the Sisters of the Holy Cross of Notre Dame, Indiana, convert a sturdy four-story red brick building to two wards, 18 private rooms and an operating room with an amphitheater. The facility is called Hawkes Hospital of Mount Carmel and eventually becomes Mount Carmel West. 100 Years. 100 Facts. | 9 A 10-bed Christ Hospital opens in 006 Cincinnati after a group of local 1889 businessmen led by James Gamble (whose prospering soap business eventually became Procter & Gamble) invited Isabella Thornburg to the city in 1888 to train deaconesses and missionaries. She soon expands beyond training to open a hospital in the west end of the city. -
Clinisync Contributing Members As of December 2020
CliniSync Contributing Members As of December 2020 Accounts Accounts Account Record Type Account Name Facilities CCD Publish Descrete Data (HL7) Community Allwell Behavioral Health Services YES Blanchard Valley Medical Associates Inc (BVMA) YES Central Ohio Primary Care Physicians YES Coleman Professional Services YES Comprehensive Internal Medicine YES Crystal Clinic Inc YES Crystal Clinic Inc. YES Health Partners of Western Ohio YES Lake County Family Practice YES Legacy Health Services-Parkside Villa YES Local Public Health Services Collaborative YES Logan Elm Health Care YES Lower Light Christian Health Center YES Medical Associates of Cambridge Inc. YES National Youth Advocate Program YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Collinwood Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Corporate YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - East Cleveland Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Hough Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Miles Broadway Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Mobile Dental Unit YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Norwood Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Southeast Health Center YES NorthEast Ohio Neighborhood Health Services Inc (NEON) - Superior Health Center YES The Buckeye Ranch YES UH Amherst Primary Care YES UH Ashtabula Primary Care YES UH Avon Women's Health Care -

Residency Appointments – July 2005 by Hospital/Specialty
Residency Appointments – July 2005 By Hospital/Specialty Anesthesiology Albany Medical Center Hospital – Albany, NY Boston University Medical Center – Boston, MA Brookdale Hospital Medical Center – Brooklyn, NY George Washington University Medical Center – Washington, D.C. John H. Stroger Hospital of Cook County – Chicago, IL Maimonides Medical Center – Brooklyn, NY Medical College of Georgia – Augusta, GA The Ohio State University – Columbus, OH Pennsylvania State University/Milton S. Hershey Medical Center – Hershey, PA St. Vincent’s Hospital – New York, NY State University of New York Health Science Center, Downstate – Brooklyn, NY State University of New York, Upstate Medical Center – Syracuse, NY University Hospital – Cincinnati, OH University of Kansas School of Medicine – Wichita, KS University of Kentucky Medical Center – Lexington, KY Wake Forest Baptist Medical Center – Winston-Salem, NC Wayne State University/Detroit Medical Center – Detroit, MI West Virginia University Health Sciences Center School of Medicine – Morgantown, WV Emergency Medicine Duke University Medical Center – Durham, NC Louisiana State University Health Sciences Center – Shreveport, LA Pitt County Memorial Hospital/Brody School of Medicine – Greenville, NC Wayne State University/Detroit Medical Center – Detroit, MI Wayne State University/ Sinai-Grace Hospital – Detroit, MI University Hospital, Jackson – Jackson, MS University of Louisville School of Medicine – Louisville, KY University of Medicine and Dentistry of New Jersey – Newark, NJ University of Puerto -

Designated Hospitals and Outpatient Surgery Centers
Ohio and Northern Kentucky UnitedHealthcare Directory of Designated Hospitals and Outpatient Surgery Centers With Choice Plus Advanced with Hospital Tiering, UnitedHealthcare encourages members to make well-informed decisions about who to see and where to go for quality, cost-efficient care through the UnitedHealth Premium® designation program, Place of Service and Hospital Tiering. This directory is a listing of the Designated hospitals and Outpatient Surgery Centers that offer services to UnitedHealthcare members enrolled in our Choice Plus Advanced with Hospital Tiering health plans in Ohio and Northern Kentucky. Members may pay lower co-payments and co-insurance amounts for services provided by Designated hospitals and surgery centers. The providers on this list may change. The Ohio Designated Hospitals and Outpatient Surgery Centers Allen: Belmont: Springfield Regional Cleveland Association Digestive Health Endoscopy Digestive Health Complex Medical Center* 5106 Wilson Mills Rd 375 N Eastown Rd 300 W Main St 100 Medical Center Drive Richmond Heights, OH 44143 Springfield, OH 45504 Lima, OH 45807 Saint Clairsville, OH 43950 Cleveland Center For Digestive Endoscopy Center Valley Endoscopy Center Mercy Memorial Hospital* Health & Endoscopy Of West Central Ohio 68377 STEwart Dr STE 202 904 Scioto St 3700 Park East Dr STE 100A 2793 Shawnee Rd Saint Clairsville, OH 43950 Urbana, OH 43078 Beachwood, OH 44122 Lima, OH 45806 Cleveland Eye/Laser Butler: Clermont: Endoscopy Center Surgery Center GI Endoscopy Center Midwest Eye Surgery Center -

Ohiohealth Grant Medical Center Community Health Needs Assessment June 2019 Ohiohealth Grant Medical Center
OhioHealth Grant Medical Center Community Health Needs Assessment June 2019 OhioHealth Grant Medical Center Nationally Recognized for Specialized Trauma Care and Surgical Excellence OhioHealth Grant Medical Center is the only adult hospital in downtown Columbus that offers a full range of adult medical services and specialties. We offer easy access with free valet parking to our patients and visitors. We provide the highest standard of quality care for every patient. Our physicians, nurses, support staff and volunteers are committed to making your visit at Grant the best possible experience. Stacey K. Armstrong, President 111 South Grant Avenue Columbus, Ohio 43215 Board approval of CHNA Report: 06/18/2019 Initial Web posting of CHNA Report: 06/26/2019 Tax identification number: 31-4394942 OhioHealth Grant Medical Center I Table of Contents Introduction .............................................................................................................................................................. 1 A. Definition of the Community Served by the Hospital Facility and How the Community Served Was Determined .................................................................................................................................................... 4 B. Demographics of the Community .......................................................................................................................... 5 C. Existing Healthcare Facilities and Resources within the Community that are Available to Respond to the Health Needs -

Table S1. Participating Centers Huntsville Hospital Alabama Baptist Medical Center East Alabama St. Vincent Birmingham Alabama T
Table S1. Participating Centers Huntsville Hospital Alabama Baptist Medical Center East Alabama St. Vincent Birmingham Alabama The Children's Hospital at Providence, Alaska Alaska St. Joseph's Hospital and Medical Center Arizona Cardon Children's Medical Center Arizona Banner Thunderbird Medical Center Arizona Banner Estrella Medical Center Arizona Abrazo Arrowhead Campus Arizona Arizona Children's Center Maricopa Integrated Health Arizona Flagstaff Medical Center Arizona Willow Creek Women's Hospital Arkansas University of Arkansas for Medical Sciences Arkansas Mercy Hospital Fort Smith Arkansas Providence Tarzana Medical Center California Providence Little Company of Mary Medical Center California Rocky Mountain Hospital for Children at Presbyterian/Saint Luke’s Colorado St. Mary's Hospital and Medical Center Colorado Swedish Medical Center Colorado Poudre Valley Hospital Colorado Good Samaritan Medical Center Colorado Denver Health Medical Center Colorado Stamford Hospital Connecticut Danbury Hospital Connecticut Yale-New Haven Children's Hospital Connecticut Connecticut Children's NICU at UCONN Health Center Connecticut Norwalk Hospital Connecticut The Hospital of Central Connecticut Connecticut Greenwich Hospital Connecticut Washington Hospital Center District of Columbia Joe DiMaggio Children's Hospital Florida Florida Hospital for Children Florida Sacred Heart Health System Florida Baptist Children's Hospital Florida St. Joseph's Children's Hospital Florida Women's Center at Florida Hospital - Tampa Florida UF Shands Hospital Gainesville Florida UF Health Jacksonville Florida North Florida Regional Medical Center, Inc. Florida Gwinnett Hospital System Georgia The Medical Center at Columbus Regional Georgia Piedmont Rockdale Hospital Georgia Hamilton Medical Center Georgia Floyd Medical Center Georgia Kapiolani Medical Center for Women & Children Hawaii St. Luke's Regional Medical Center Idaho St. -

La Leche League: Websites Books
Central Ohio La Leche Websites Central Ohio Hospitals Breastfeeding www.breastfeedingonline.com Mom Group Meetings League: www.kellymom.com Support www.BFAR.org International Organization Grant Medical Center Mount Carmel East Mount Carmel West www.askdrsears.com Breastfeeding Moms Group Breastfeeding Moms Group that Provides Mothers with www.infantrisk.com Breastfeeding Moms Group Breastfeeding Education www.lowmilksupply.org When: Every Tuesday When: Every Tuesday When: Every Friday 11:00 a.m.—12:00 p.m. www.health.state.mn.us/divs/fh/wic 2:00 p.m.—3:00 p.m. 2:00 p.m.—3:00 p.m. For contact information and (Spanish. Somali) monthly meeting dates/times, www.nlm.nih.gov/medlineplus/ Where: Where: breastfeeding.html (English and Spanish) Grant Medical Center, 4th floor classroom Where: Community Health please visit www.llli.org. www.womenshealth.gov: 1-800-994-9662 4th Floor Mother Infant Resource Center (English and Spanish) Lounge La Leche League of Gahanna www.womenshealth.gov/ItsOnlyNatural/ Gahanna Library index.html 310 Granville Rd. Gahanna, OH 43230 (614) 566-9008 (614) 234-MILK (614) 234-MILK La Leche League of Hilliard Scioto Ridge United Methodist Church 4343 Dublin Rd. Books Hilliard, OH 43026 “The Womanly Art of Breastfeeding” by La Leche League Riverside Methodist Hospital Mount Carmel St. Ann’s La Leche League of “The Nursing Mother’s Companion” Breastfeeding Moms Group Hospital Breastfeeding Moms Reynoldsburg Group by Kathleen Huggins When: Every Thursday Reynoldsburg United “Mothering Multiples” by Karen Gromada 1:30 p.m.—2:30 p.m. When: Every Wednesday Methodist Church 1636 Graham Rd. -
![Pageflex Server [Document: PF2025696 00001]](https://docslib.b-cdn.net/cover/0763/pageflex-server-document-pf2025696-00001-3140763.webp)
Pageflex Server [Document: PF2025696 00001]
Need a 2021 Medicare Advantage hospital that's close to you? Anthem Blue Cross and Blue Shield gives you choices. A strong hospital network with quality providers is an important thing to consider when you're shopping for a health care plan. That's why Anthem Blue Cross and Blue Shield is happy to offer this extensive list of Ohio hospitals included in our 2021 Medicare Advantage networks.* We're committed to helping you stay healthy. With our networks, you'll have easy access to the care you need, right when you need it. To learn more, please talk to your sales agent or licensed independent broker today! Akron and NE OH - excludes Cuyahoga Affinity Medical Center (HMO, PPO, SNP) St Elizabeth Health Center (HMO, PPO, SNP) Akron Childrens Hospital (HMO, PPO, SNP) St Joseph Health Center (HMO, PPO, SNP) Akron General Medical Center (HMO, PPO, SEL, SNP) Stark County Emergency Physicians, Inc (HMO, PPO, Alliance Community Hospital (HMO, PPO, SNP) SNP) Ashtabula County Medical Center (HMO, PPO, SEL, Summa Health System (HMO, PPO, SNP) SNP) Surgical Hospital at Southwoods (HMO, PPO, SNP) Aultman Hospital (HMO, PPO, SNP) Tripoint Medical Center (HMO, PPO, SNP) Crystal Clinic Orthopaedic Center LLC (HMO, PPO, Trumbull Memorial Hospital (HMO, PPO, SNP) SNP) UH Portage Medical Center (HMO, PPO, SNP) East Liverpool City Hospital (HMO, PPO, SNP) University Hospital Geauga Medical Center (HMO, Lake Hospital System (HMO, PPO, SNP) PPO, SNP) Lake West (HMO, PPO, SNP) University Hospital Geneva Medical Center (HMO, Mercy Medical Center (HMO, PPO, SNP)