Framework for the Implementation of the Ouagadougou Declaration on Primary Health Care and Health Systems in Africa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Meta-Analysis of Travel of the Poor in West and Southern African Cities Roger Behrens, Lourdes Diaz Olvera, Didier Plat, Pascal Pochet
Meta-analysis of travel of the poor in West and Southern african cities Roger Behrens, Lourdes Diaz Olvera, Didier Plat, Pascal Pochet To cite this version: Roger Behrens, Lourdes Diaz Olvera, Didier Plat, Pascal Pochet. Meta-analysis of travel of the poor in West and Southern african cities. WCTRS, ITU. 10th World Conference on Transport Research - WCTR’04, 4-8 juillet 2004, Istanbul, Turkey, 2004, Lyon, France. pp.19 P. halshs-00087977 HAL Id: halshs-00087977 https://halshs.archives-ouvertes.fr/halshs-00087977 Submitted on 8 Oct 2007 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. 10th World Conference on Transport Research, Istanbul, 4-8 July 2004 META-ANALYSIS OF TRAVEL OF THE POOR IN WEST AND SOUTHERN AFRICAN CITIES Dr. Roger Behrens*, Dr. Lourdes Diaz-Olvera (corresponding author)**, Dr. Didier Plat**and Dr. Pascal Pochet** * Department of Civil Engineering, University of Cape Town, Private Bag, Rondebosch, 7701, South Africa. Email: [email protected] ** Laboratoire d'Economie des Transports, ENTPE-Université Lumière Lyon 2-CNRS, rue Maurice Audin, 69518, Vaulx-en-Velin Cedex, France. Email: [email protected]; [email protected]; [email protected] ABSTRACT There have been few attempts in the past to compare travel survey findings in francophone and anglophone African countries. -

“Flooding Our Eyes with Rubbish”: Urban Waste Management in Maputo, Mozambique
780090EAU Environment and Urbanization “Flooding our eyes with rubbish”: urban waste management in Maputo, Mozambique INGE TVEDTEN AND SARA CANDIRACCI Inge Tvedten is a ABSTRACT Critical voices on urban management tend to portray conflicting senior researcher and governmentalities, with Western “top-down” municipal development models anthropologist at Chr. on the one hand, and the everyday practices and diffuse forms of power of the Michelsen Institute, with poor majority on the other. This paper takes solid waste (lixo) management in expertise in urban and rural poverty monitoring Mozambique’s capital city, Maputo, and its informal settlements as an entry point and analysis; public service for assessing the relationship between these two urban development perspectives. delivery; gender and It shows that while the municipality considers itself to be working actively through women’s empowerment; public–private partnerships to handle the complex issue of waste management in and development the informal areas, people in these informal settlements, despite paying a regular cooperation/institutional fee for waste removal, continue to experience lixo as a serious problem and see its development. persistent presence as a symbol of spatial and social inequalities and injustice. The Address: Chr. Michelsen paper is formulated as a conversation between city planning and management and Institute, Jekteviksbakken the community side of the equation – leading to a joint set of proposals for how 31 P.O. Box 6033, Bergen best to manage such a contentious part of African urban life. 5892, Norway; e-mail: Inge. [email protected] KEYWORDS citizen–state relations / divided city / informal settlements / Maputo Sara Candiracci is an urban planner with experience / urban poverty / urban sanitation / waste management from urban development programmes in Africa, Asia and Latin America. -

1 Environmental Factors and Childhood Fever in Areas of the Ouagadougou
Environmental factors and childhood fever in areas of the Ouagadougou – Health and Demographic Surveillance System – Burkina Faso Franklin Bouba Djourdebbé1, Stéphanie Dos Santos2, Thomas LeGrand3 and Abdramane Soura4 1 PhD Candidate in Demography, University of Montreal, Email: [email protected] 2 Stéphanie Dos Santos, PhD, Researcher IRD/ISSP-Ouagadougou (Burkina Faso). Email: [email protected] 3 Thomas LeGrand, PhD, Director of the Department of Demography, University of Montreal (Canada). Email: [email protected] 4 Abdramane Soura, PhD, Researcher ISSP-Ouagadougou (Burkina Faso). Email: [email protected] Problem and objectives Unhealthy environments are responsible for a significant proportion of morbidity and mortality worldwide.1, 2 The World Health Organization estimates that the global burden of disease from environmental factors is 24%, and these factors are responsible for 23% of all deaths each year. Preventing environmental risks could reduce the number of child deaths by nearly 4 million every year, mostly in developing countries.1 In African cities, infectious diseases like malaria, acute respiratory infections and diarrheal diseases contribute to a longstanding critical health situation.3 The growth of African cities in the last three decades as also led to profound changes in the local environmental context. Rapid population growth, combined with a lack of access to basic sanitation services (access to clean water, management of household waste and water, etc.) and poor housing conditions, have had a harmful effect on the health and wellbeing of urban populations.4 Understanding the links between environmental risk factors and public health is essential for the development of effective policies and programs, and ultimately to the future wellbeing of West African urban populations. -

Adolescent Fertility Is Lower Than Expected in Rural Areas: Results from African HDSS
REPORT Adolescent Fertility Is Lower than Expected in Rural Areas: Results from African HDSS Clémentine Rossier, Bruno Schoumaker, Valérie Delaunay, Donatien Beguy, Aparna Jain, Martin Bangha, Alemseged Aregay, Baptiste Beck, Karim Derra, Modeste Millogo, Albert Nkhata Dube, Kone Siaka, Marylene Wamukoya, and Pascal Zabre The adolescent birth rate (ABR) is an important indicator of maternal health, adolescent sexual health, and gender equity; it remains high in sub-Saharan Africa. While Demographic and Health Surveys (DHS) are the main source of ABR estimates, Health and Demographic Surveillance Systems (HDSS) also produce ABRs. Studies are lacking, however, to assess the ease of access and ac- curacy of HDSS ABR measures. In this paper, we use birth and exposure data from HDSS in six African countries to compute local ABRs and compare these rates to DHS regional rates where the HDSS sites are located, standardiz- ing by education and place of residence. In rural HDSS sites, the ABR measure is on average percent lower than the DHS measure, after controlling for ed- ucation and place of residence. Strong temporary migration of childless young women out of rural areas and different capacities in capturing temporarily ab- sent women in the DHS and HDSS could explain this discrepancy. Further comparisons based on more strictly similar populations and measures seem warranted. Clémentine Rossier, University of Geneva, Geneva, Switzerland and Institut National d’Etudes Démo- graphiques, Paris, France. E-mail: [email protected]. Bruno Schoumaker, Université Catholique de Louvain, Louvain-la-Neuve, Belgium. Valérie Delaunay, Institut de Recherche pour le Développe- ment, Marseille, France. Donatien Beguy, African Population and Health Research Center, Nairobi, Kenya. -

African Union (AU) Commission Campaign Against Trafficking in Persons
MEDIA ADVISORY Consultative Workshop on Operationalizing the Ouagadougou Action Plan to Combat Trafficking in Human Beings & Launching of the African Union (AU) Commission Campaign against trafficking in persons INVITATION TO REPRESENTATIVES OF THE MEDIA TO COVER THE WORKSHOP AND TO ATTEND THE OPENING CEREMONY AND PRESS BRIEFING WHAT: Two-day consultative workshop on operationalising the Ouagadougou Action Plan to Combat Trafficking In Human Beings Especially Women and Children & Launching of The AU Commission Initiative Against Trafficking In Persons (AU.COMMIT) Campaign With The Regional Economic Communities. WHO: Advocate Bience Gawanas, Commissioner for Social Affairs of the AU Mr Mandiaye Niang, United Nations Office on Drugs and Crime (UNODC) Regional Representative for Southern Africa Mr. Bernardo Mariano-Joaquim, International Organization for Migration (IOM) Regional Director for East and Southern Africa WHEN: Opening Ceremony starts on 29 November 2011, 09:00-10:00 am followed by a press briefing at 10:00 WHERE: Johannesburg, Republic of South Africa, Kopanong Hotel, Tel: +27 (11) 749-0000, Fax: +27 (11) 967-1389, 243 Glen Gory Road, Norton Estate, Benoni, South Africa, http://www.kopanong.co.za. OBJECTIVES: The consultative workshop will foster effective ways of networking, coordination and cooperation among Member States and partners to address trafficking in persons in Southern Africa in a more strategic and programmatic manner. The objective will also be to sensitise SADC member states on the operationalisation of the Ouagadougou Action Plan to Combat Trafficking in Human Beings, Especially Women and Children, and on the regional launching of the AU. COMMIT campaign. The AU.COMMIT Campaign endeavours to raise awareness of the AU’s continued commitment towards addressing the problem of trafficking in human beings throughout the continent. -

Policies for Sustainable Mobility and Accessibility in Cities of Burkina Faso
Page 1 Policies for sustainable mobility and accessibility in cities of Burkina Faso Page 2 ¾ SSATP – Burkina Faso - Policies for Sustainable Mobility and Accessibility in Cities – October 2019 Page 3 ¾ SSATP – Burkina Faso - Policies for Sustainable Mobility and Accessibility in Cities – October 2019 Policies for sustainable mobility and accessibility in cities of Burkina Faso An international partnership supported by: Page 4 ¾ SSATP – Burkina Faso - Policies for Sustainable Mobility and Accessibility in Cities – October 2019 The SSATP is an international partnership to facilitate policy development and related capacity building in the transport sector in Africa. Sound policies lead to safe, reliable, and cost-effective transport, freeing people to lift themselves out of poverty and helping countries to compete internationally. * * * * * * * The SSATP is a partnership of 42 African countries: Angola, Benin, Burkina Faso, Burundi, Cameroon, Cape Verde, Central African Republic, Chad, Comoros, Congo, Democratic Republic of the Congo, Côte d'Ivoire, Djibouti, Eswatini, Ethiopia, Gabon, The Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Madagascar, Malawi, Mali, Mauritania, Morocco, Mozambique, Namibia, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, South Sudan, Tanzania, Togo, Tunisia, Uganda, Zambia, Zimbabwe; 8 Regional Economic Communities (RECs); 2 African institutions: African Union Commission (AUC) and United Nations Economic Commission for Africa (UNECA); Financing partners for the Third Development Plan: European -

September 11Th, 2018 Fertility Transition in Dakar, Nairobi And
September 11th, 2018 Fertility transition in Dakar, Nairobi and Ouagadougou since the 1970s: a similar decline at all ages? Roch Millogo and Clementine Rossier Short abstract (n=156) The pattern of the African fertility decline remains in debate: while some researchers expect a transition similar to the declines in Europe, Latin America and Asia, where limitation practices and long- acting methods played a major role, others believe that the African transition will be different. This paper places itself in this debate: it aims to test Caldwell's prediction that African fertility declines will occur similarly at all ages, by the adoption of modern contraceptives also at all ages. We look at Dakar, Nairobi and Ouagadougou, three African urban contexts of relatively low fertility, where women have around three children in 2010-2015, using data available for these cities since the early 1970s. Caldwell et al.’s hypothesis that African fertility transitions will be characterized by similar fertility reductions at all ages is confirmed for these three cities, but contraception has not been the main strategy to expand the avoidance of childbearing in all cities and at all ages. Introduction While all other regions have already completed their fertility transition, SSA is the only part of the world that continues its transition at a slow pace: the average number of children remains high (5.1 2010-2015) (Casterline, 2001; Bongaarts et Casterline, 2013; UN, 2015). However, there is a wide disparity across the continent, with the decline being closely linked to wealth, urban residence, and especially high levels of education (Kravdal, 2002; Bongaarts, 2003; Gurmu and Macer, 2008; Shapiro and Gebreselassie, 2009; Assefa and Semahegn, 2016, National Academies of Sciences, Engeneering, and Medicine, 2016). -

An Estimated Dynamic Model of African Agricultural Storage and Trade
High Trade Costs and Their Consequences: An Estimated Dynamic Model of African Agricultural Storage and Trade Obie Porteous Online Appendix A1 Data: Market Selection Table A1, which begins on the next page, includes two lists of markets by country and town population (in thousands). Population data is from the most recent available national censuses as reported in various online databases (e.g. citypopulation.de) and should be taken as approximate as census years vary by country. The \ideal" list starts with the 178 towns with a population of at least 100,000 that are at least 200 kilometers apart1 (plain font). When two towns of over 100,000 population are closer than 200 kilometers the larger is chosen. An additional 85 towns (italics) on this list are either located at important transport hubs (road junctions or ports) or are additional major towns in countries with high initial population-to-market ratios. The \actual" list is my final network of 230 markets. This includes 218 of the 263 markets on my ideal list for which I was able to obtain price data (plain font) as well as an additional 12 markets with price data which are located close to 12 of the missing markets and which I therefore use as substitutes (italics). Table A2, which follows table A1, shows the population-to-market ratios by country for the two sets of markets. In the ideal list of markets, only Nigeria and Ethiopia | the two most populous countries | have population-to-market ratios above 4 million. In the final network, the three countries with more than two missing markets (Angola, Cameroon, and Uganda) are the only ones besides Nigeria and Ethiopia that are significantly above this threshold. -

The Ouagadougou Declaration and Plan of Action on Accelerating Prisons’ and Penal Reforms in Africa
The Ouagadougou Declaration and Plan of Action on Accelerating Prisons’ and Penal Reforms in Africa Recognising that there has been progress in raising general prison standards in Africa as recommended by the Kampala Declaration on Prison Conditions 1996 Recognising also the specific standards on alternatives to imprisonment contained in the Kadoma Declaration on Community Service Orders in Africa 1997; and on good prison administration set out in the Arusha Declaration on Good Prison Practice 1999 Noting the recognition given to these African standards by the United Nations as complementary to the United Nations Standard Minimum Rules for the Treatment of Prisoners, the Declaration on the Basic Rights of Prisoners and the United Nations Standard Minimum Rules for non-custodial measures (the 'Tokyo Rules') Mindful of the key role played by Africans in formulating an agenda for penal reform through the 1999 Egham Conference on 'A New Approach for Penal Reform in a New Century' Noting with satisfaction the important practical steps that have been taken to implement these standards at an African level through the activities of the African Commission on Human and Peoples' Rights and its Special Rapporteur on Prisons and Conditions of Detention Commending the practical measures that have been taken by prison authorities in African countries to apply these standards in their national jurisdictions Recognising that notwithstanding these measures there are still considerable shortcomings in the treatment of prisoners, which are aggravated by shortages of facilities and resources Welcoming the growing partnerships between Governments, non governmental organizations and civil society in the process of implementing these standards Emphasising the importance of a criminal justice policy that controls the growth of the prison population and encourages the use of alternatives to imprisonment The participants at the second pan-African Conference on Prison and Penal Reform in Africa, held in Ouagadougou, Burkina Faso between 18-20 September 2002, recommend: 1. -
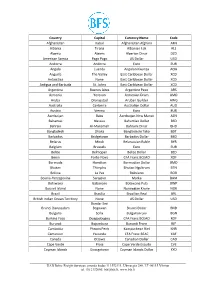
International Currency Codes
Country Capital Currency Name Code Afghanistan Kabul Afghanistan Afghani AFN Albania Tirana Albanian Lek ALL Algeria Algiers Algerian Dinar DZD American Samoa Pago Pago US Dollar USD Andorra Andorra Euro EUR Angola Luanda Angolan Kwanza AOA Anguilla The Valley East Caribbean Dollar XCD Antarctica None East Caribbean Dollar XCD Antigua and Barbuda St. Johns East Caribbean Dollar XCD Argentina Buenos Aires Argentine Peso ARS Armenia Yerevan Armenian Dram AMD Aruba Oranjestad Aruban Guilder AWG Australia Canberra Australian Dollar AUD Austria Vienna Euro EUR Azerbaijan Baku Azerbaijan New Manat AZN Bahamas Nassau Bahamian Dollar BSD Bahrain Al-Manamah Bahraini Dinar BHD Bangladesh Dhaka Bangladeshi Taka BDT Barbados Bridgetown Barbados Dollar BBD Belarus Minsk Belarussian Ruble BYR Belgium Brussels Euro EUR Belize Belmopan Belize Dollar BZD Benin Porto-Novo CFA Franc BCEAO XOF Bermuda Hamilton Bermudian Dollar BMD Bhutan Thimphu Bhutan Ngultrum BTN Bolivia La Paz Boliviano BOB Bosnia-Herzegovina Sarajevo Marka BAM Botswana Gaborone Botswana Pula BWP Bouvet Island None Norwegian Krone NOK Brazil Brasilia Brazilian Real BRL British Indian Ocean Territory None US Dollar USD Bandar Seri Brunei Darussalam Begawan Brunei Dollar BND Bulgaria Sofia Bulgarian Lev BGN Burkina Faso Ouagadougou CFA Franc BCEAO XOF Burundi Bujumbura Burundi Franc BIF Cambodia Phnom Penh Kampuchean Riel KHR Cameroon Yaounde CFA Franc BEAC XAF Canada Ottawa Canadian Dollar CAD Cape Verde Praia Cape Verde Escudo CVE Cayman Islands Georgetown Cayman Islands Dollar KYD _____________________________________________________________________________________________ -

The Meningitis Vaccine Project Closure Conference Addis Ababa
The Meningitis Vaccine Project Closure Conference Addis Ababa, Ethiopia: 22-25 February 2016 Meningitis surveillance in the African meningitis belt Dr André Bita, Clément Lingani, Olivier Ronveaux WHO ISTWA, HQ Outline 1. Background 2. Objectives of meningitis surveillance 3. Epidemiological situation of meningitis in Africa 4. Performance analysis of meningitis surveillance 5. Lessons learned 6. Summary 7. Way forward Annexes :Definition case; Operational thresholds; Performance indicators of surveillance 2 | Epidemic meningitis in Africa: Disease burden Reported cases 200,000 188,345 170,000 140,000 92,347 100,000 88,939 88,199 80,743 80,000 68,089 60,000 40,000 27,3011 20,000 0 Years 3 | Background -1 l Meningitis remains a major public health problem in Africa especially in the 26 countries of the meningitis belt. l The bacterial status changed since the introduction of MenAfriVac in Africa in 2010. Previously, NmA that was predominant. Thus, from 2010 to now, S.Pn, NmW, and NmC are predominant l The 3-pillar strategy to eliminate meningitis in Africa; Surveillance; case management; and vaccination l In order to improve the detection of meningitis case and assess the impact of introduction of MenAfriVac, Enhance surveillance (ES) and case based surveillance (CBS) have been introduced respectively in 2003 and 2010 4 | Background -2 l 2003 - 2015: introduction of ES in 19 countries of meningitis belt l 2010-2015: introduction of CBS; currently 13 countries are experiencing CBS l Initiated in 2010 in BFA, Mali, and Niger l 2014: Improvement of CBS in BFA, Mali, Niger, Togo, and (Ethiopia & Chad are in the process) through the MenAfriNet project conducted by CDC with the partnership of WHO, AMP & MoH countries concerned 5 | Background -3 Main differences between ES & CBS Elements ES CBS Lumbar puncture and CSF analysis for suspected meningitis cases >= 80% >= 90% Case investigation form filled for suspected meningitis cases >=80% 100% epidemiological data followed by lab data Routine reporting, management, and analysis of case-level data. -

BURKINA FASO Gb 06
Burkina Faso Ouagadougou key figures • Land area, thousands of km2 274 • Population, thousands (2005) 13 228 • GDP per capita, $ PPP valuation (2005) 1 085 • Life expectancy (2000-2005) 47.4 • Illiteracy rate (2005) 71.5 African Economic Outlook 2005-2006 www.oecd.org/dev/publications/africanoutlook All tables and graphs in this section are available in Excel format at: http://dx.doi.org/10.1787/830215840706 Burkina Faso town > l million inhabitants main airport 500 000 - 1 000 000 secondary airport 100 000 - 500 000 commercial port petroleum port fishing port THE COUNTRY HAD A VERY MIXED YEAR in 2005. The very high 2005/06 food-crop harvest, Between January and September a shortfall in the implementation of certain structural reforms and 2004/05 food-crop harvests created a sub-regional food completion of key infrastructural work (road repairs, crisis and a return of inflation. The economic climate electricity link-ups and new dams) in this landlocked was also affected by the delayed impact of the Ivorian country promised more sustained growth in the next crisis on transport costs (and thus supply of raw materials few years. Greater The respectable economic for industry) and by the sustained increase in oil prices. competition in the banking performance of 2005 But these problems remained under control. The public sector, with new banks and cannot hide the vulnerability adapted to higher fuel prices and the excellent 2004/05 creation of the Banque underlined by the food crisis cotton harvest (640 000 tonnes, up from 480 000 in régionale de solidarité at the beginning of the year.