Obstructive Sialoadenitis Role of Interventional Sialography
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Argon Medical Devices Products Catalogue
ARGON PRODUCTS CATALOGUE Argon Medical Devices Products Catalogue WWW.ARGONMEDICAL.EU.COM www.argonmedical.eu.com[ 1 ] ARGON PRODUCTS CATALOGUE WWW.ARGONMEDICAL.EU.COM [ 2 ] [ 3 ] ARGON PRODUCTS CATALOGUE Table of Contents Thrombus Management .....................................................5 Endomyocardial Biopsy ................................................... 63 • Option™ELITE Inferior Vena Cava Filter System ....................6 • Jawz™ Endomyocardial Biopsy (EMB) Forceps ................... 64 • Atrieve™ Vascular Snare Kit ����������������������������������������������������8 • Endomyocardial Biopsy Accessories ���������������������������������� 65 • V+Pad™ Hemostasis Pads ......................................................9 • CLEANERXT™ & CLEANER15™ Rotational Thrombectomy System ................................................................................. 10 Bone & Bone Marrow Biopsy .......................................... 67 • T-Lok™ Bone Marrow Biopsy Needles ................................. 68 • Bone Marrow Aspiration Needles....................................... 68 Drainage ............................................................................13 • Bone Marrow Harvest Needles .......................................... 69 • SKATER™ Single Step Drainage Catheters ......................... 15 • Pediatric Bone Marrow Access Needles ............................ 69 • SKATER™ Drainage Catheters ............................................. 16 • Osty-Core™ Bone Biopsy Needles ...................................... -

Contemporary Methods for the Treatment of Pulmonary Embolism — Is It Prime-Time for Percutaneous Interventions?
Kardiologia Polska 2017; 75, 11: 1161–1170; DOI: 10.5603/KP.a2017.0125 ISSN 0022–9032 ARTYKUŁ SPECJALNY / STATE-OF-THE-ART REVIEW Contemporary methods for the treatment of pulmonary embolism — is it prime-time for percutaneous interventions? Marcin Kurzyna1, Arkadiusz Pietrasik2, Grzegorz Opolski2, Adam Torbicki1 1Department of Pulmonary Circulation, Thromboembolic Diseases and Cardiology, European Health Centre Otwock, Centre of Postgraduate Medical Education, Otwock, Poland 2Department and Faculty of Cardiology, Medical University of Warsaw, Warsaw, Poland Marcin Kurzyna, MD, PhD. Since 1998 he has been a physician in the Intensive Care Unit, and since 2003 the Head of the Haemodynamic Lab in the National Institute for Lung Diseases. Cur- rently he is Deputy Head of the Department of Pulmonary Circulation, Thromboembolic Diseases, and Cardiology and an associate professor in the Centre of Postgraduate Medical Education in Warsaw. He was a Chairman of Working Group on Pulmonary Circulation of Polish Cardiac Society (2013–2015). He is a specialist in internal medicine and cardiology and has a PhD in respiratory medicine. His research interests are currently related to the role of invasive procedures in the diagnosis and treatment of pulmonary vascular diseases. Arkadiusz Pietrasik, MD, PhD is an assistant in the First Chair and Department of Cardiology, Medical University of Warsaw. He is an independent operator certified by the Association of Car- diovascular Interventions (AISN) of the Polish Cardiac Society. His research interests cover structural heart diseases, coronary artery diseases, intravascular visualisation techniques, and chronic throm- boembolic pulmonary hypertension. He is a coordinator of the Pulmonary Embolism Response Team (CELZAT) at the Central Clinical Hospital of the Medical University of Warsaw. -

Stock Available with Stock Position
scode generic measurement Formulation Stock Available [Customer Demand Annualy] Annual Consumption A003 ACETYLSALICYLIC ACID 300MG TABLET 3,170 12,240 4,177 A017 ANTACID CHEWABLE TABLETS TABLET CHEWABLE 221,950 646,560 386,286 A022 BACLOFEN 10MG TABLET 64,848 483,732 319,924 A038 CALCIUM LACTATE 300MG TABLET 266,000 1,797,612 1,172,351 A042 CARBIDOPA|LEVODOPA 10MG|100MG TABLET 145,200 1,661,940 1,560,315 A043 CARBIDOPA|LEVODOPA 25MG|250MG TABLET 2,850 A062 CLOMIPRAMINE HYDROCHLORIDE 25MG TABLET 320,000 1,731,612 976,556 A063 COLCHICINE 500µ TABLET 49,254 314,412 171,971 A073 DAPSONE 50MG TABLET 13,552 22,668 12,395 A077 DIGOXIN 0.0625MG TABLET 313,936 1,313,736 827,752 A089 DYDROGESTERONE 10MG TABLET 2,520 7,128 2,234 A094 ETHAMBUTOL HYDROCHLORIDE 400MG TABLET 3,864 15,012 9,882 A112 FRUSEMIDE 40MG TABLET 175,700 872,880 479,257 A113 FUSIDATE SODIUM 250MG TABLET 2,300 9,888 5,318 A115 GLYCERYL TRINITRATE 500µ TABLET 36,340 578,364 324,289 A119 HALOPERIDOL 0.5MG CAPSULE 49,448 363,552 429,849 A137 ISOSORBIDE DINITRATE 10MG TABLET 338,080 1,005,972 386,600 A149 LOPERAMIDE HYDROCHLORIDE 2MG CAPSULE 19,900 229,284 116,993 A154 MEDROXYPROGESTERONE ACETATE 5MG TABLET 1,000 5,592 3,626 A155 MEDROXYPROGESTERONE ACETATE 100MG TABLET 4,200 24,456 13,295 A172 MEXILETINE HCL 200MG CAPSULES 1,680 2,296 A176 METOCLOPRAMIDE 10MG TABLET 59,892 167,208 72,894 A179 NAPROXEN 250MG TABLET 56,636 158,316 26,261 A184 NITROFURANTOIN 50MG CAPSULE 11,220 77,112 37,419 A188 OESTROGENS CONJUGATED 0.625MG TABLET 1,764 9,696 7,716 A202 PHENOXYMETHYLPENICILLIN 250MG -

Fluoroscopy in Research Fact Sheet
Fluoroscopy in FactSheet Research luoroscopy is an imaging procedure that uses a continuous x-ray beam to create real-time images viewed on a monitor. It enables physicians to view internal organs and vessels in motion and can be used in both F diagnostic and therapeutic procedures. The long term risk associated with fluoroscopy is cancer, What I need to know... however, more immediate risks of skin injury due to high doses are possible. The typical fluoroscopic entrance Dose Reduction Techniques exposure rate for a medium-sized adult is approximately 30 mGy/min (3 rad/min), but is typically higher in image- • Use ultrasound imaging when possible. recording modes. Table 1 on the next page illustrates skin • Position the image intensifier as close to the injury per fluoroscopy dose and time of onset. patient as practicable. • Maximize the distance from the radiation For physicians/researchers, it is not often clear when the source. use of fluoroscopy is considered Standard of Care versus research. • Remove Grids. Grids improve the image quality, however, they increase the dose to the Standard of Care (SOC) is about clinical judgement, patient and staff by a factor of two or more. decision flexibility, whereas research needs to adhere • Use pulsed rather than continuous fluoroscopy strictly to protocols. The following assessments assist when possible, and with as low a pulse as the physician/researcher in determining whether use of possible. fluoroscopy is for research purposes: • Would the subject receive this care absent of the clinical trial? • Can you back yourself up in the literature? • Does local SOC differ from national standards/ guidelines? • Are protocol deviations documented? For any “NO” answer to the above, use of fluoroscopy may be for research purposes. -
Annual Meeting Delegate Handbook
BSIR 2016 ANNUAL MEETING DELEGATE HANDBOOK 1 5TH-1 7TH NOVEMBER 2016 MANCHESTER CENTRAL MANCHESTER 1 MAJOR SPONSORS 2 CONTENTS PAGE CONTENTS 4 Welcome to BSIR 2016 5 Speaker Instructions 6-7 General Information & Social Events WEDNESDAY 4TH NOVEMBER 2015 9 Programme Day 1 10 Scientific Sessions 1 & 2 11 The Graham Plant Proessorship 2016 12 SIRNR Programme 13 Industry Showcases 14 Masterclasses & Workshops THURSDAY 5TH NOVEMBER 2015 15 Programme Day 2 16 Scientific Sessions 3 & 4 17 OOH Intervention Snapshot Survey 18 Masterclasses & Workshops 19 Industry Showcases FRIDAY 6TH NOVEMBER 2015 20 Programme Day 3 21 Scientific Sessions 5 & 6 22 BSIR/BSIRT Trainee Day Programme 24 BSIR Honorary Fellowships: Professor Mike Dake & Dr Giles Maskell 25 BSIR Gold Medal: Professor Anthony Watkinson 26 Wattie Fletcher Lecture: Dr Richard McWilliams 27 Graham Plant Lecturer 28-29 Faculty Biographies 30-31 Faculty Lists 32-33 Exhibition Plan 34 List of Exhibitors 36-46 Exhibitor Bios 48-49 SIRNR Section 50 BSIR AGM 53-61 BSIR Committee Reports 62 BSIR Membership Form 64-69 BSIR/BSIRT Trainee Day Essay Scholars 70-75 BSIR Abstract & Case Study Review 76 VASBI 2017 - Trainee Day Meeting Announcement 77-100 BSIR Abstracts - Scientific Sessions 1-6 101 VASBI 2017 - Meeting Announcement 102-107 BSIR Scientific & Educational Posters 108 The U Foundation 109 BSIR 2017 - Meeting Announcement 110 BSIR IOUK 2017 - Meeting Announcement 3 WELCOME TO BSIR 2016 Dear Colleagues, The theme of this year scientific program continues from the last year’s one which entails covering the widest possible aspects of interventional radiology within the limited conference time. -

Upper Gastrointestinal Series
Fluoroscopy-Upper Gastrointestinal (UGI) To Schedule: (319) 861-7778 Questions about Procedure: (319) 398-6050 What is an Upper Gastrointestinal (UGI) Series? A upper gastrointestinal (UGI) series refers to a x-ray of the upper digestive tract. This includes the esophagus and stomach and may include the small bowel, if requested by your physician. In order to visualize the upper digestive tract, you will be asked to swallow gas-producing granules. You will also be asked to drink some barium, and the radiologist or radiologist assistant will take images as the barium moves through your system. The esophagus or stomach procedures usually take about 30 minutes. If a small bowel study is also requested, the exam may take 2-4 hours with the extra time necessary to follow the barium through the small intestine. Preparation: Day 1 – Day Before Exam 1. You may eat or drink anything the day before the study until 10:00 pm. You are encouraged to drink plenty of fluids. 2. After 12:00 a.m. (midnight) do not eat or drink anything until your exam has been completed on the following day. 3. After 12:00 a.m. (midnight) do not smoke or chew gum until your exam has been completed on the following day. Day 2 – Day of Exam 1. No breakfast, do not eat or drink until after the test. 2. Take NO medications. PLEASE BRING THE FOLLOWING TO YOUR APPOINTMENT: A PHOTO ID TO VERIFY YOUR IDENTITY A LIST OF CURRENT MEDICATIONS YOU ARE TAKING Procedure: 1. You will be asked to drink a small glass of barium and to swallow some bubble-forming granules. -
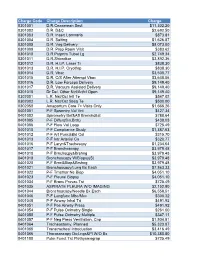
NUMC-CDM-Jan2019.Pdf
Charge Code Charge Description Charge 0301001 D.R.Ceaserean Sect $11,302.20 0301002 D.R. D&C $2,692.50 0301003 D.R. Insert Lamnaria $873.81 0301004 D.R. Salting $1,626.87 0301005 D.R. Vag Delivery $8,073.00 0301009 D.R. Prep Room Visit $383.62 0301010 D.R.Pstprtm Tubal Lg $2,749.34 0301011 D.R.Shirodkar $3,892.36 0301012 D.R. H.I.P. Laser Tr $838.30 0301013 D.R. H.I.P. Cryothrp $838.30 0301014 D.R. Vbac $3,500.77 0301015 D.R. C/S After Attempt Vbac $3,648.06 0301016 D.R. Low Forceps Delivery $9,149.40 0301017 D.R. Vacuum Assisted Delivery $9,149.40 0301018 Dr Del. Other Ntrl/Artfcl Open $9,149.40 0302001 L.R. Nst/Oct Intl Te $547.02 0302002 L.R. Nst/Oct Sbsq Te $500.00 0302050 Antepartum Care 7> Visits Only $1,666.26 0401001 P-F Spromtry Vol Vnt $427.34 0401002 Spirometry Bef&Aft Bronchdilat $788.64 0401005 P-F Diffus(Sin.Brth) $438.03 0401006 P-F Flow Vol Loop $725.49 0401010 P-F Compliance Study $1,387.63 0401012 P-F Art Punc&Bld Col $315.70 0401013 P-F Intr Arterial Ca $320.77 0401016 P-F Laryn&Trachescpy $1,234.64 0401017 P-F Bronchoscopy $3,979.48 0401018 P-F Brnchscpy&Brshng $3,979.48 0401019 Bronchoscopy W/Biopsy(S) $3,979.48 0401020 P-F Brnc&Biop&Brshng $3,979.48 0401021 Bronchoscopy/Lung Bx Each $7,863.33 0401022 P-F Trnsthor Ne Biop $4,051.10 0401023 P-F Pleural Biopsy $4,051.10 0401034 P-F Bronc Provac Tst $725.49 0401035 ASPIRATE PLEURA W/O IMAGING $2,152.80 0401044 Bronchoscopy/Needle Bx Each $6,558.51 0401046 P-F Lungfunc Mbc/Mvv $300.32 0401048 P-F Airway Inhal Trt $491.92 0401051 P-F Pos Airway Press $491.92 0401054 P-F -

Interventional Fluoroscopy Reducing Radiation Risks for Patients and Staff
NATIONAL CANCER INSTITUTE THE SOCIETY OF INTERVENTIONAL RADIOLOGY Interventional Fluoroscopy Reducing Radiation Risks for Patients and Staff Introduction CONTENTS Interventional fluoroscopy uses ionizing radiation to guide small instruments such as catheters through blood vessels or other pathways in the body. Interventional fluoroscopy represents a Introduction 1 tremendous advantage over invasive surgical procedures, because Increasing use and it requires only a very small incision, substantially reduces the complexity of risk of infection and allows for shorter recovery time compared interventional fluoroscopy 1 to surgical procedures. These interventions are used by a rapidly expanding number of health care providers in a wide range of Determinants of radiation medical specialties. However, many of these specialists have little dose from interventional fluoroscopy 2 training in radiation science or protection measures. The growing use and increasing complexity of these procedures Radiation risks from interventional fluoroscopy 3 have been accompanied by public health concerns resulting from the increasing radiation exposure to both patients and health care Strategies to optimize personnel. The rise in reported serious skin injuries and the radiation exposure from expected increase in late effects such as lens injuries and interventional fluoroscopy 4 cataracts, and possibly cancer, make clear the need for informa- Physician-patient tion on radiation risks and on strategies to control radiation communication before and exposures to patients and health care providers. This guide after interventional fluoroscopy 4 discusses the value of these interventions, the associated radiation risk and the importance of optimizing radiation dose. Dosimetry records and follow up 4 Education and training 5 Increasing use and complexity of interventional Conclusion 5 fluoroscopy Reference list 5 In 2002, an estimated 657,000 percutaneous transluminal coronary angioplasty (PTCA) procedures were performed in adults in the United States. -

Pediatric Upper Gastrointestinal (GI) Series
Pediatric Upper Gastrointestinal (GI) Series An upper gastrointestinal (GI) series is an x-ray exam of the upper digestive tract. This includes the mouth, esophagus, stomach, and duodenum (first part of the small intestine). The exam is used to detect problems such as strictures (narrowing), or ulcers (sores in the lining of the GI tract). Barium contrast or another kind of contrast material is used during the exam. This is a liquid that makes organs show more clearly on x-rays. During an upper GI series with small bowel follow-through, the doctor also checks the small intestine. An upper GI series takes about 60 minutes. An upper GI series with small bowel follow-through takes about 3 hours. Before the Exam Don’t give your child anything to eat or drink 4–6 hours before the exam. Follow all other instructions given by the doctor. Let the Technologist Know For your child’s safety, let the technologist know if your child: Has allergies. Has any health problems. Has had surgery. Is taking any medications. During an upper GI series, your child is given liquid barium contrast to drink. During the Exam An upper GI series is performed by a radiologist. This is a doctor trained to use x-rays to test or treat patients. A radiology technologist may also assist with the exam. You can stay with your child in the x-ray room. You’ll be given a lead apron to wear for your safety. Your child stands against the x-ray table during the first part of the exam. -
IDEAS 2015 Pocket Guide General Information
Interdisciplinary Endovascular Aortic Symposium IDEAS 2015 September 27-29 Lisbon/Portugal Interdisciplinary Endovascular Aortic Symopsium POCKET GUIDE POCKET GUIDE POCKET 2015 EAS INNOVATION | EDUCATION | INTERVENTION Cardiovascular and Interventional Radiological Society of Europe ID Scientific & Educational Programme * Corporate Activities 4 General Information from A to Z 10 Session Types Sunday - Scientific Programme 11 SUN Monday - Scientific Programme 14 MON Tuesday - Scientific Programme 17 TUE 19 Corporate Activities 22 Satellite Symposia 39 Learning Centres 48 Technical Exhibition 48 Alphabetical & Numerical List 54 Technical Exhibitors Guide 110 Radiation Protection Pavilion 124 Floor Plans * advertisement-free section in accordance with the document UEMS 2012/30 – the Accreditation of Live Educational Events of the EACCME® (article 33/34) Cardiovascular and Interventional Radiological Society of Europe Welcome Address Welcome to the inaugural IDEAS symposium! Keep an eye out for the Endovascular aortic therapies have long been of interest to in- CIRSE Society app update terventional radiologists, vascular surgeons and cardiologists alike – the option to treat the aorta in a minimally invasive New features and design in time for CIRSE 2015! way opens exciting therapeutic possibilities, but realising this dream has been anything but straightforward. Install the CIRSE 2015 event to ensure your access to the best toolkit for the Annual Meeting in Lisbon: Recent technological advances have brought with them fresh enthusiasm for minimally invasive repair of aortic aneurysms – a complex category of interventions that rely heavily on the skills of a well-trained multidisciplinary medical team. • New! paperless session evaluation The various professionals involved in this team all bring their • e-voting own essential skills to the table. -

Diagnostic and Nuclear Medical Physics Residency Program Summary of Rotation Presentation Topics
Diagnostic and Nuclear Medical Physics Residency Program Summary of Rotation Presentation Topics Last updated: 11/17/2020 Radiography (2020) Advanced image processing in digital radiography (2020) Dual energy x-ray absorptiometry (DXA) (2019) EOS scoliosis imaging system (2019) Dental radiographic technologies (2018) Radiographic techniques for scoliosis patients (2018) Exposure index in digital radiography (2017) Heel effect and how to mitigate it in clinical procedures, physics testing and image processing (2017) AAPM TG 151: ongoing quality control in digital radiography (2016) Routine applications, special procedures, and QC for projection radiography Fluoroscopy (2020) Fluoroscopy-guided trans-catheter aortic valve replacement (TAVR) (2020) The process of estimating peak skin dose (PSD) in fluoroscopy (2019) My clinical observations of non-interventional fluoroscopy procedures (2019) Medical physics guide to calculating peak skin dose from RDSR data (2018) My shadowing experience in non-interventional fluoroscopy (2018) Interventional fluoroscopy in cardiology (2017) Patient skin dose estimation in fluoroscopic procedures (2017) TheraSphere® Yttrium-90 microsphere therapy (2016) Clinical applications and methods to monitor and reduce patient dose in fluoroscopy Mammography (2020) Mammography screening recommendations and data (2020) Medical physicist’s tests in the 2018 ACR digital mammography QC manual (2019) Contrast-enhanced digital mammography and tomosynthesis-guided biopsies (2019) Technology improvements -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular