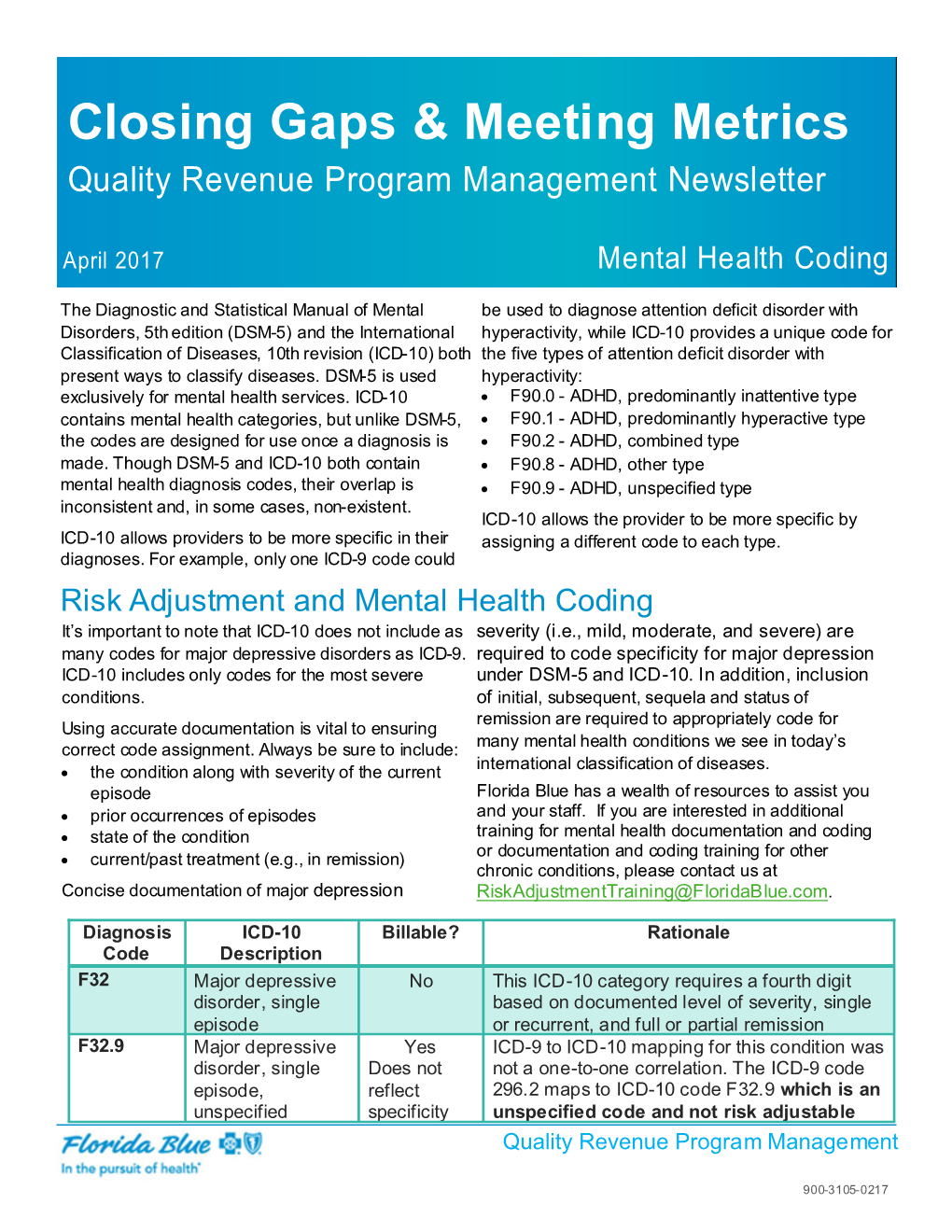
Mental Health Coding
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Healthcare System in Saudi Arabia and Its Challenges: the Case of Diabetes Care Pathway
Journal of Health Informatics in Developing Countries www.jhidc.org Vol. 10 No. 1, 2016 Submitted: October 6, 2015 Accepted: January 17, 2016 The Healthcare System in Saudi Arabia and its Challenges: The Case of Diabetes Care Pathway Sarah Hamad ALKADI King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia Abstract. The advances of Information Technology (IT) play an important role globally in improving quality and capacity of healthcare sector. IT helps the health professions in managing resources and increasing productivity effectively. Although the conversion from paper to electronic patient records (EPR) conveys many benefits for both caregivers and caretakers, but also has brought many challenges in different aspects. Hospitals have implemented EPR to different degrees. They have used a set of standards in order to insure that data is accurately and consistently processed. Even though, the standardization of how data are captured, exchanged and used includes a set of complications that should be discovered to provide better health data quality for patients with multiple healthcare providers. Therefore, through an analysis of the EPR systems utilization in Saudi Arabia and the diabetes care pathway, three factors have been determined. These factors affect the workflow of the implementation and utilization of health information system (HIS) in terms of capturing, sharing and using its data efficiently. Keywords. HIS, EPR, information sharing, social factors, standards, health information management, diabetes care pathway, health informatics, data capturing, data sharing, Saudi Arabia. 1. Introduction The technology investment in health sector has importance in the management of healthcare services delivery in the developing countries. It is necessary to enhance the utilization as well as the implementation of HIS through standardizing the medical data in order to have a better data quality and more reliable system. -

What Is Medical Coding? What Is Medical Coding? Medical Coding Professionals Provide a Key Step in the Medical Billing Process
Training Certification Continuing Education ICD-10 Jobs Networking Resources Store Log In / Join Certification Overview Medical Coding Certification Medical Billing Certification Medical Auditing Certification Medical Compliance Certification Practice Manager Certification Locate Exam Prepare for Exam Exam Tips Credential Verification FAQ Home > Medical Coding > What is Medical Coding? What is Medical Coding? Medical coding professionals provide a key step in the medical billing process. Every time a patient receives professional health care in a physician’s office, hospital outpatient facility or ambulatory surgical center (ASC), the provider must document the services provided. The medical coder will abstract the information from the documentation, assign the appropriate codes, and create a claim to be paid, whether by a commercial payer, the patient, or CMS. Prepare for certification and a career in medical coding Validate your knowledge, skills, and expertise with medical coding certification Is Medical Coding the same as Medical Billing? No. While the medical coder and medical biller may be the same person or may work closely together to make sure all invoices are paid properly, the medical coder is primarily responsible for abstracting and assigning the appropriate coding on the claims. In order to accomplish this, the coder checks a variety of sources within the patient’s medical record, (i.e. the transcription of the doctor’s notes, ordered laboratory tests, requested imaging studies and other sources) to verify the work that was done. Then the coder must assign CPT® codes, ICD-9 codes and HCPCS codes to both report the procedures that were performed and to provide the medical biller with the information necessary to process a claim for reimbursement by the appropriate insurance agency. -

ICD-10 Faqs FAQ Review
Welcome to ICD-10 FAQ REVIEW Topics for Discussion . ICD-10 Overview . About ICD-10 . Why ICD-10 Matters ICD-10 . General ICD-10 FAQs FAQ Review . Split Claims FAQs . WV ICD-10 Provider Testing FAQs . Resources . Contact 1 ICD-10 Overview . World Health Organization developed ICD-10 in 1994 . Later adopted by Health and Human Services (HHS) and Centers for Disease Control and Prevention (CDC). ICD-10 is a provision of Health Insurance Portability and Accountability Act (HIPAA) regulations. HIPAA covers entities that include health care providers, payers, clearinghouses, billing services and others that must transition to ICD-10. Moving from ICD-9 to ICD-10 – U.S. is the last industrialized nation to adopt ICD-10 . ICD-9 is outdated - limited capacity, capability and unable to serve future needs . ICD-10-CM and ICD-10-PCS code sets . ICD-10-CM replaces ICD-9-CM (Volumes 1 and 2) . ICD-10-PCS replaces ICD-9-CM (Volume 3) . ICD-10 has no direct impact on Current Procedural Terminology (CPT) codes and Healthcare Common Procedure Coding System (HCPCS) 2 ICD-10 Overview (Cont.) . For services rendered on or after October 1, 2015 . All claims must use ICD-10 codes . Claims using ICD-9 codes for services rendered on or after October 1, 2015 will NOT be accepted . For services rendered before October 1, 2015 . All claims must use ICD-9 codes . Systems must accommodate BOTH ICD-9 and ICD-10 codes . Effective with the October 1, 2015 compliance date . Significant code increase from ICD-9 to ICD-10 . Increasing from 14,000 to approximately 69,000 ICD-10-CM codes . -

1 the Business of Medicine
Chapter 1 The Business of Medicine Coding as a Profession language, a patient’s condition, or the care provided can change code selection completely. Each time you receive health care, a record is maintained of the resulting observations, medical or surgical inter- Technicians who specialize in coding are medical coders ventions, and treatment outcomes. This medical record or coding specialists. Medical coders assign a code to includes information concerning your symptoms and each diagnosis, service/procedure, and (when applicable) medical history, the results of examinations, reports of supply, using classification systems. The classification X-rays and laboratory tests, diagnoses, and treatment system determines the amount health care providers plans. will be reimbursed if the patient is covered by Medi- care, Medicaid, or other insurance programs using the At its most basic, coding is the process of translating system. this written or dictated medical record into a series of numeric or alpha-numeric codes. There are sepa- If the medical record is inaccurate or incomplete, it rate code sets to describe diagnoses, medical and will not translate properly to the language of codes and surgical services/procedures, and supplies. These reimbursement for services may be lost. The coder must code sets serve as a common “shorthand” language to evaluate the medical record for completeness and accu- ease data collection (for example, to track disease), to racy and communicate regularly with physicians and evaluate the quality of care, and to determine costs and other health care professionals to clarify diagnoses or reimbursement. to obtain additional patient information. Coders may use computer programs to tabulate and analyze data to Coders may use several coding systems, such as those improve patient care, better control cost, provide docu- required for ambulatory settings, physician offices, mentation for use in legal actions, or use in research or long-term care. -

Psychologycoding.Com 1 10/28/2015 Psychologycoding.Com 2
Disclaimer The information contained in this extended presentation is not intended to The Changing Face of Healthcare: reflect AMA, APA, CMS (Medicare), any division of APA, NAN, NAP, NCPA (or any state psychological association), state Medicaid and/or any private third The Interface Between CPT & ICD party carrier policy. Further, this information is intended to be informative and does not supersede APA or state/provincial licensing boards’ ethical guidelines and/or local, state, provincial or national regulations and/or laws. Further, Local Coverage Determination and specific health care contracts supersede the information presented. The information contained herein is meant to provide practitioners as well as health care institutions (e.g., insurance companies) involved in psychological services with the latest ANTONIO E. PUENTE information available to the author regarding the issues addressed. This is a living document that can and will be revised as additional information UNIVERSITY OF NORTH CAROLINA WILMINGTON becomes available. The ultimate responsibility of the validity, utility and application of the information contained herein lies with the individual and/or institution using this information and not with any supporting organization and/or the author of this presentation. Suggestions or changes should be directly addressed to the author. Note that whenever possible, references are provided. Finally, note that the CPT system is copyrighted and the information contained should be treated as such. CPT information is provided -
ICD-10-CM Specialized Coding Workbook with Answers
DPH ICD-10 IMPLEMENTATION PROJECT ICD-10-CM SPECIALIZED CODING TRAINING WORKBOOK FOR LOCAL HEALTH DEPARTMENTS AND RURAL HEALTH CLINICS (WITH ANSWERS) WBS 2.5 Version 1.1 This Page Was Intentionally Left Blank 2 DPH ICD-10 Implementation Project WBS 2.5 – Training Materials ICD-10-CM Specialized Coding Training Workbook – With Answers Change History Version Number & Date Version Description Version Author Modifications made to coincide with Sarah Brooks revisions made in training materials wherein training was broken into Units. V1.0 – February 24, 2015 Instead of separate workbooks for each Specialized course, a single workbook is developed for the Specialized courses. V1.1 – February 26, 2015 Minor changes – final product Sarah Brooks 3 DPH ICD-10 Implementation Project WBS 2.5 – Training Materials ICD-10-CM Specialized Coding Training Workbook – With Answers Table of Contents 1. ICD-10-CM: THE CHAPTERS ........................................................................................................................... 9 2. ICD-10-CM: THE CHAPTER BLOCKS .......................................................................................................... 10 2.1 CHAPTER 1 - CERTAIN INFECTIOUS AND PARASITIC DISEASES (A00-B99) ...................................................... 10 2.2 CHAPTER 2 - NEOPLASMS (C00-D49) ............................................................................................................ 11 2.3 CHAPTER 3 - DISEASES OF THE BLOOD AND BLOOD-FORMING ORGANS AND CERTAIN DISORDERS INVOLVING THE -

Buyer's Guide
July 2008 Left to right: Dorraine Edwards, CPC Christy Christensen, CPC RoseMarie Smith, CPC JoAnne Stephens, CPC Buyer’s Guide Chris Martinelli, CPC, CPC-H, CPC-P Including: CodeRyte HealthcareBusinessOffice, LLC Ingenix Practice Management Information Corp CodingWebU Coding Metrix/Coding Strategies, Inc MC Strategies Physician Chart Auditor Z Publishing Medical Compliance Training Cengage Learning Doctors Management Elsevier Healthcare Compliance Resources 3M American Hospital Association Plus: Art of Negotiating • Resources to Buy • Coding Complacency • Hiring a Consultant Good News! You’ve known us as The Medical Management Institute. Get to know us as Contexo Media. Tools and Training for Healthcare Professionals Since 1986, we’ve known the value of providing coding products and education to medical professionals. More than 260,000 customers and students, 22 years and one name change later, we still do. So, what’s new? Over the last year, we established the industry’s rst Peer Review Editorial Board, dramatically upgraded the quality of all of our publications, created dozens of new products, and partnered with the American Medical Association to bring you the rst regional CPT® Changes seminars. Our instructors have been busy, too, training over 6,000 medical professionals last year. Their source material? Our coding, billing, reimbursement and compliance publications. No other company puts their products in the hands of more instructors or workshop attendees than us. P.O. Box 25128 | Salt Lake City, Utah 84125-0128 This eld-testing, and the guidance of the industry’s only Peer Review Editorial Board and internal experts, helps 800.334.5724 | Fax 801.365.0710 us ensure our publications and educational oerings meet vigorous expectations – yours. -

Medicare Claims Processing Manual Chapter 32 – Billing Requirements for Special Services
Medicare Claims Processing Manual Chapter 32 – Billing Requirements for Special Services Table of Contents (Rev. 10891, 07-20-21) Transmittals for Chapter 32 10- Diagnostic Blood Pressure Monitoring 10.1 - Ambulatory Blood Pressure Monitoring (ABPM) Billing Requirements 11 - Wound Treatments 11.1 – Electrical Stimulation 11.2 – Electromagnetic Therapy 11.3 – Autologous Platelet-Rich Plasma (PRP) for Chronic Non-Healing Wounds 11.3.1 – Policy 11.3.2 – Healthcare Common Procedure Coding System (HCPCS) Codes and Diagnosis Coding 11.3.3 – Types of Bill (TOB) 11.3.5 - Place of Service (POS) for Professional Claims 11.3.6 – Medicare Summary Notices (MSNs), Remittance Advice Remark Codes (RARCs), Claim Adjustment Reason Codes (CARCs) and Group Codes 12 - Counseling to Prevent Tobacco Use 12.1 - Counseling to Prevent Tobacco Use HCPCS and Diagnosis Coding 12.2 - Counseling to Prevent Tobacco Use A/B MAC (B) Billing Requirements 12.3 - A/B MAC (A) Billing Requirements 12.4 - Remittance Advice (RA) Notices 12.5 - Medicare Summary Notices (MSNs) 12.6 - Post-Payment Review for Counseling To Prevent Tobacco Use Services 12.7 - Common Working File (CWF) Inquiry 12.8 - Provider Access to Counseling To Prevent Tobacco Use Services Eligibility Data 20 – Billing Requirements for Coverage of Kidney Disease Patient Education Services 20.1 – Additional Billing Requirements Applicable to Claims Submitted to Fiscal Intermediaries (FIs) 20.2 - Healthcare Common Procedure Coding System (HCPCS) Procedure Codes and Applicable Diagnosis Codes 20.3 - Medicare Summary -

Initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid (Medicaid Adult Core Set)
1 Initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid (Medicaid Adult Core Set) Technical Specifications and Resource Manual for Federal Fiscal Year 2013 February 2013 Center for Medicaid and CHIP Services Centers for Medicare & Medicaid Services 2 For NCQA measures in the Initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid: © 1994-2013 by the National Committee for Quality Assurance (NCQA) 1100 13th Street, NW, Suite 1000 Washington, D.C. 20005 All rights reserved. Reprinted with the permission of NCQA. Inclusion of NCQA performance measures in any commercial product require permission of NCQA and is subject to a license at the discretion of NCQA. NCQA performance measures are not clinical guidelines and do not establish a standard of medical care. NCQA makes no representations, warranties or endorsement about the quality of any organization or physician that uses or reports performance measures and NCQA has no liability to anyone who relies on such measures. 3 CONTENTS I. The Initial Core Set of Health Care Quality Measures for Adults Enrolled in Medicaid ........................................................................................................... 5 Background ...................................................................................................... 5 How the Medicaid Adult Core Set Will Be Used ............................................. 10 II. Data Collection and Reporting of the Medicaid Adult Core Set ................................. 11 Data Collection -
Guidance on Terminology Standards for Ireland
GUIDANCE ON TERMINOLOGY STANDARDS FOR IRELAND HEALTH INFORMATION AND QUALITY AUTHORITY Guidance on Terminology Standards for Ireland July 2017 Safer Better Care 1 GUIDANCE ON TERMINOLOGY STANDARDS FOR IRELAND HEALTH INFORMATION AND QUALITY AUTHORITY Version Control Date Version Change December 2013 1.0 Published as Guidance on Classification and Terminology Standards for Ireland. July 2017 2.0 Updated to reflect revisions to international standards and other relevant changes. 2 GUIDANCE ON TERMINOLOGY STANDARDS FOR IRELAND HEALTH INFORMATION AND QUALITY AUTHORITY About the Health Information and Quality Authority The Health Information and Quality Authority (HIQA) is an independent authority established to drive high-quality and safe care for people using our health and social care services in Ireland. HIQA’s 0role is to develop standards, inspect and review health and social care services and support informed decisions on how services are delivered. HIQA’s ultimate aim is to safeguard people using services and improve the safety and quality of health and social care services across its full range of functions. HIQA’s mandate to date extends across a specified range of public, private and voluntary sector services. Reporting to the Minister for Health and the Minister for Children and Youth Affairs, HIQA has statutory responsibility for: . Setting Standards for Health and Social Services — Developing person-centred standards, based on evidence and best international practice, for health and social care services in Ireland. Regulation — Registering and inspecting designated centres. Monitoring Children’s Services — Monitoring and inspecting children’s social services. Monitoring Healthcare Safety and Quality — Monitoring the safety and quality of health services and investigating as necessary serious concerns about the health and welfare of people who use these services. -

Viii 2019 CPB™ Certification Study Guide CPT® Copyright 2018 American Medical Association
2019 MEDICAL BILLING TRAINING TM CERTIFIEDCPB PROFESSIONAL BILLER STUDY GUIDE 2019 CPB™ Certification Study Guide Disclaimer This course was current when it was published. Every reasonable effort has been made to assure the accuracy of the information within these pages. The ultimate responsibility lies with readers to ensure they are using the codes, and following applicable guidelines, correctly. AAPC employees, agents, and staff make no representation, warranty, or guarantee that this compilation of information is error-free, and will bear no responsibility or liability for the results or consequences of the use of this course. This guide is a general summary that explains guidelines and principles in profitable, efficient healthcare organizations. US Government Rights This product includes CPT®, which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable, which was developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/ or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2) (November 1995), as applicable, for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/ or subject to the restricted rights provision of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements. -
The International Classification of Diseases Version 10 (ICD-10)
The International Classification of Diseases Version 10 (ICD-10) What you need to know before the end of February, 2014 Gary W. Williams, MD, PhD, FACR 1.8.2014 Objectives: 1. Review the history of the International List of Causes of Death and its relation to the International Classification of Disease 2. Recognize ICD-9 as inadequate to classify diseases 3. Identify how ICD-10 assists coding 4. Examine why ICD-11 is needed (and on its way) 5. Recognize the role of: 1. Code Sets, 2. Reference Terminologies, and 3. Interface Terminologies in Electronic Health Records; 6. Describe Allscripts’ MAPPING of ICD-9 codes to ICD-10 7. Demonstrate Allscripts functionality in CONVERTING ICD-9 codes to ICD-10 Death Registration • The beginnings of death registration can be found in mid-15th century Italy • A death certificate was required before a burial certificate could be issued • By the 16th Century, Boards of Health were established in France, Switzerland and the Netherlands • Used to monitor epidemics in various cities Bills of Mortality • 1532 – England began a systematic collection of data on causes of death, the Bills of Mortality. • 1837 – The Registration Act was passed in England with provisions for inquiry into causes of death in the population. • 1842 – The first State Registration law in the US was enacted by Massachusetts in 1842. American Medical Association • 1855 – The American Medical Association (AMA) adopted a resolution urging its members to take “immediate and concerted action in petitioning legislative bodies to establish offices for the registration of vital events”. • 1900 – Ten states and the District of Columbia had met the requirements of the U.S.