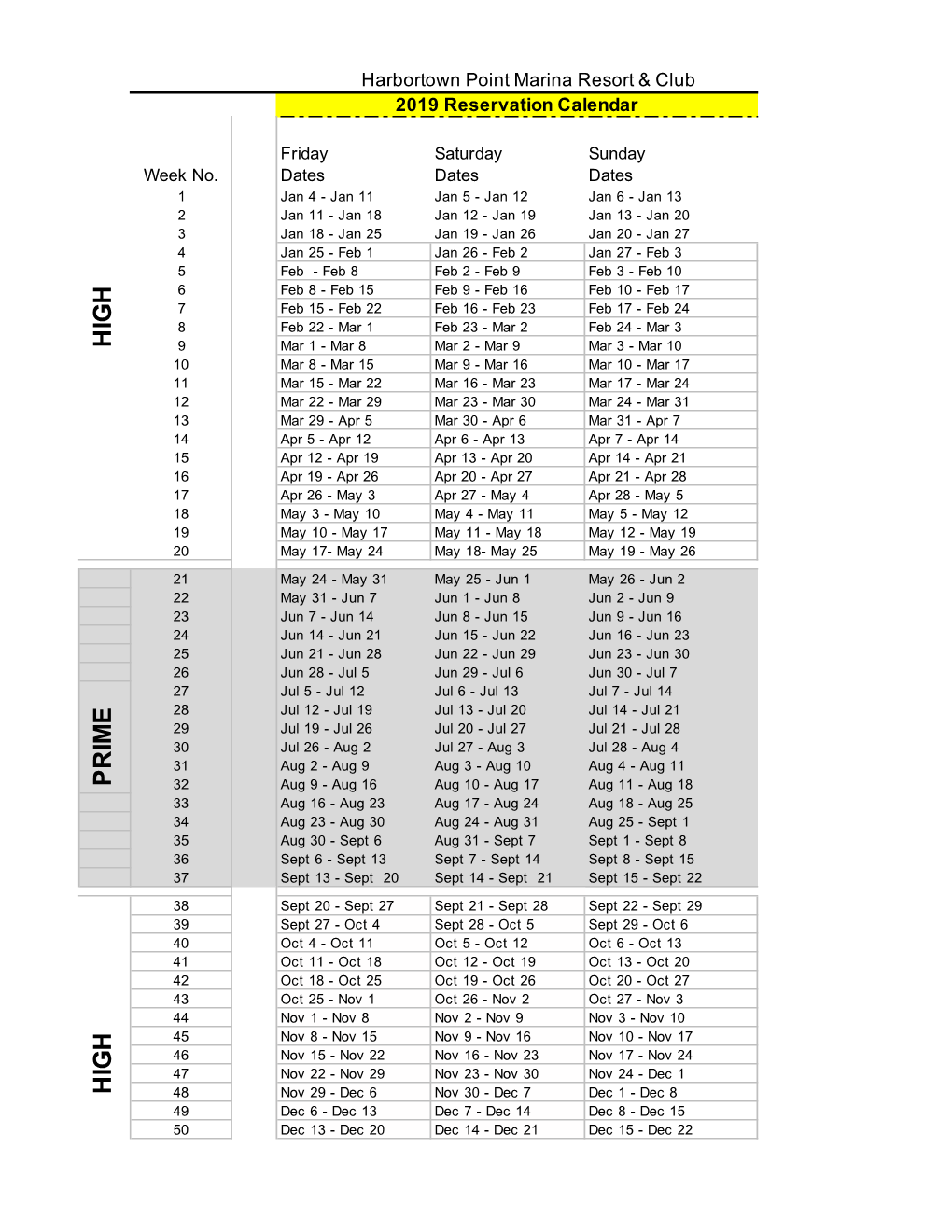
Hig H Hig H Pr Im E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thursday Calendar 20142018
THURSDAY Five-Year Calendar Unit 2014 20152016 2017 2018 Week # 1 Jan. 2 - Jan. 9 Jan. 1 - Jan. 8 Jan. 7 - Jan. 14 Jan. 5 - Jan. 12 Jan. 4 - Jan. 11 2 Jan. 9 - Jan. 16 Jan. 8 - Jan. 15 Jan. 14 - Jan. 21 Jan. 12 - Jan. 19 Jan. 11 - Jan. 18 3 Jan. 16 - Jan. 23 Jan. 15 - Jan. 22 Jan. 21 - Jan 28 Jan. 19 - Jan. 26 Jan. 18 - Jan. 25 4 Jan. 23 - Jan. 30 Jan. 22 - Jan. 29 Jan. 28 - Feb. 4 Jan. 26 - Feb. 2 Jan. 25 - Feb. 1 5 Jan. 30 - Feb. 6 Jan. 29 - Feb. 5 Feb. 4 - Feb. 11 Feb. 2- Feb. 9 Feb. 1 - Feb. 8 6 Feb. 6 - Feb. 13 Feb. 5 - Feb. 12 Feb. 11 - Feb. 18 Feb. 9 - Feb. 16 Feb. 8 - Feb. 15 7 Feb. 13 - Feb. 20 Feb. 12 - Feb. 19 Feb. 18 - Feb. 25 Feb. 16 - Feb. 23 Feb. 15 - Feb. 22 8 Feb. 20 - Feb. 27 Feb. 19 - Feb. 26 Feb. 25 - Mar. 3 Feb. 23 - Mar. 2 Feb. 22 - Mar. 1 9 Feb. 27 - Mar. 6 Feb. 26 - Mar. 5 Mar. 3 - Mar. 10 Mar. 2 - Mar. 9 Mar. 1 - Mar. 8 10 Mar. 6 - Mar. 13 Mar. 5 - Mar. 12 Mar. 10 - Mar. 17 Mar. 9 - Mar. 16 Mar. 5 - Mar. 15 11 Mar. 13 - Mar. 20 Mar. 12 - Mar. 19 Mar. 17 - Mar. 24 Mar. 16 - Mar. 23 Mar. 15 - Mar. 22 12 Mar. 20 - Mar. 27 Mar. 19 - Mar. 26 Mar. 24 - Mar. 31 Mar. 23 - Mar. 30 Mar. 22 - Mar. -

Spring Semester 2022
Student Application/Processing Calendar – Academic Year 2021-2022 Includes thesis and dissertation submission deadlines University Academic Calendar - Spring Semester 2022 (Actual Class Days: 14 Mondays, 15 Tuesdays, 14 Wednesdays, 14 Thursdays, 13 Fridays; Effective Class Days: 14 Mondays, 14 Tuesdays, 14 Wednesdays, 14 Thursdays, 14 Fridays) November 5, Friday Early registration for special populations begins at 1:00 pm. November 8, Monday Registration for Spring Semester 2022 begins. January 7, Friday Advising, registration and schedule adjustments January 10, Monday Classes begin; schedule adjustments. January 14, Friday Last day for registration and schedule adjustments (drop / add) by 5:00 pm January 17, Monday State Holiday (no classes) January 24, Monday Census Day (Official enrollment count taken at 5:00 pm.) March 6 - 13, Spring Break -- Classes resume at 8:00 am Monday, March 14. Sunday - Sunday March 14 - 18, Advising for Summer Sessions and Fall Semester 2022 Monday - Friday March 24, Thursday Last day for undergraduate and graduate students to withdraw from term- length courses or withdraw from school without grades, by 5:00 pm; block courses may be dropped only during the first 60% of their regularly scheduled class meetings. March 25, Friday Early registration for special populations begins at 1:00 pm. March 28, Monday Registration for Summer Sessions and Fall Semester 2022 begins. April 13, Wednesday Survey of Student Opinion of Instruction (SSOI) becomes available. April 14, Thursday Last day for undergraduate students to submit work for removal of incompletes given during Fall 2021 April 15 - 16, State Holiday (no classes) Friday - Saturday April 26, Tuesday Last day for graduate students to submit work for removal of incompletes given during Spring Semester 2021 April 26, Tuesday State holiday makeup day; classes which would have met on Friday, April 15 will meet on this day so there will be effectively the same number of Fridays and Tuesdays as every other weekday during the semester. -

INVESTMENT COMPANY ACT of 1940 Release No
SECURITIES AND EXCHANGE COMMISSION INVESTMENT COMPANY ACT OF 1940 Release No. 33817 / March 13, 2020 ORDER UNDER SECTION 6(c) AND SECTION 38(a) OF THE INVESTMENT COMPANY ACT OF 1940 GRANTING EXEMPTIONS FROM SPECIFIED PROVISIONS OF THE INVESTMENT COMPANY ACT AND CERTAIN RULES THEREUNDER; COMMISSION STATEMENT REGARDING PROSPECTUS DELIVERY The current outbreak of coronavirus disease 2019 (COVID-19) was first reported on December 31, 2019. The disease has led to disruptions to transportation, including buses, subways, trains and airplanes, and the imposition of quarantines around the world. The Commission has heard from industry representatives that COVID-19 may present challenges for boards of directors of registered management investment companies and business development companies (“BDCs”) to travel in order to meet the in-person voting requirements under the Investment Company Act of 1940 (the “Investment Company Act” or “the Act”) and rules thereunder. In addition, we recognize that registered management investment companies and unit investment trusts (together, “registered funds”) may face challenges if, as a result of COVID-19, personnel of registered fund managers or other third-party service providers that are necessary to prepare these reports become unavailable, or only available on a limited basis, in: (i) preparing or transmitting annual and semi-annual shareholder reports; and/or (ii) timely filing Forms N-CEN and N-PORT. We also understand that due to recent market movements certain registered closed-end funds (“closed-end funds”) and BDCs may seek to call or redeem securities and may face challenges in providing the advance notice required under Rule 23c-2. Finally, we appreciate that there may be difficulties in the timely delivery of registered fund prospectuses. -
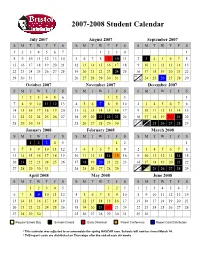
Approved Student Calendar
2007-2008 Student Calendar July 2007 August 2007 September 2007 SMTWT F S SMTWT F S SMTWT F S 1234567 1234 1 8910111213145678910 11 2 3 45678 15 16 17 18 19 20 21 12 13 14 15 16 17 18 9 10 11 12 13 14 15 22 23 24 25 26 27 28 19 20 21 22 23 24 25 16 17 18 19 20 21 22 23 29 30 31 26 27 28 29 30 31 30 24 25 26 27 28 29 October 2007 November 2007 December 2007 SMTWT F S SMTWT F S SMTWT F S 123456 123 1 7891011 12 134567 89102345678 14 15 16 17 18 19 20 11 12 13 14 15 16 17 9 10 11 12 13 14 15 21 22 23 24 25 26 27 18 19 20 21 22 23 24 16 17 18 19 20 21 22 23 24 28 29 30 31 25 26 27 28 29 30 30 31 25 26 27 28 29 January 2008 February 2008 March 2008 SMTWT F S SMTWT F S SMTWT F S 12345 12 1 67891011123456789 2345678 13 14 15 16 17 18 19 10 11 12 13 14 1516 9 1011121314 15 20 21 22 23 24 25 26 17 18 19 20 21 22 23 16 17 18 19 20 21 22 23 24 27 28 29 30 31 24 25 26 27 28 29 30 31 25 26 27 28 29 April 2008 May 2008 June 2008 SMTWT F S SMTWT F S SMTWT F S 12345 123 1234567 6789 10111245678910891011121314 13 14 15 16 17 18 19 11 12 13 14 15 16 17 15 16 17 18 19 20 21 20 21 22 23 24 25 26 18 19 20 21 22 23 24 22 23 24 25 26 27 28 27 28 29 30 25 26 27 28 29 30 31 29 30 Regular School Day Schools Closed Early Dismissal Parent Conference Report Card Distribution * This calendar was adjusted to accommodate the spring NASCAR race. -

FHA INFO #21-61 July 23, 2021 FHA Establishes New, Streamlined
FHA Establ ishes New, Str eam lined COVID- 19 Recover y Loss M itigat ion O pt ions FHA INFO #21-61 July 23, 2021 FHA Establishes New, Streamlined COVID-19 Recovery Loss Mitigation Options Today, the Federal Housing Administration (FHA) published Mortgagee Letter (ML) 2021-18, COVID-19 Recovery Loss Mitigation Options. This ML reinforces FHA’s commitment to helping homeowners who have been financially impacted by the COVID-19 pandemic to remain in their homes with new, streamlined loss mitigation options. Read today’s Press Release. This ML amends FHA’s COVID-19 Loss Mitigation policies for borrowers with FHA-insured forward mortgages, as found in Section III.A.2.o., Presidentially-Declared COVID-19 National Emergency, of the Single Family Housing Policy Handbook 4000.1 (Handbook 4000.1). It establishes the COVID-19 Recovery Loss Mitigation Options (COVID-19 Recovery Options) “waterfall” that streamlines and revises FHA’s previous options for struggling homeowners, reduces documentation requirements, and provides greater payment reduction options for eligible homeowners with FHA-insured Single Family Title II forward mortgages. The simple two-step waterfall options intended for properties that are occupied as the homeowner’s primary residence are: 1. COVID-19 Recovery Standalone Partial Claim: for homeowners who can resume making their current monthly mortgage payments, the COVID-19 Recovery Standalone Partial Claim allows mortgage payment arrearages to be placed in a zero-interest subordinate lien against the property that is repaid when the mortgage terminates, usually when the homeowner refinances or sells the home. 2. COVID-19 Recovery Modification: for homeowners who cannot resume making their current monthly mortgage payments, the COVID-19 Recovery Modification extends the term of the mortgage to 360 months at a fixed rate and targets reducing the borrower’s monthly principal and interest portion of their monthly mortgage payment. -

Texas Register July 23, 2021 Issue
Office of the Attorney General Austin Kinghorn General Counsel Notice of Settlement of a Recovery Action for Natural Office of the Attorney General Resource Damages Filed: July 13, 2021 The State of Texas gives notice of the following proposed resolution of an action to recover damages for injury to, destruction of, loss of, or loss ♦ ♦ ♦ of use of natural resources under the federal Oil Pollution Act. Before Texas Water Code and Texas Health and Safety Code the State may enter into a voluntary settlement agreement, pursuant to Settlement Notice section 7.110 of the Texas Water Code, the State shall permit the public to comment in writing. The Attorney General will consider any writ- Notice is hereby given by the State of Texas of the following proposed ten comments and may withdraw or withhold consent to the proposed resolution of an environmental enforcement action under the Texas Wa- agreement if the comments disclose facts or considerations indicating ter Code and the Texas Health and Safety Code. Before the State may that consent is inappropriate, improper, inadequate or inconsistent with enter into a voluntary settlement agreement, pursuant to section 7.110 the requirements of the law. of the Texas Water Code, the State shall permit the public to comment in writing on the proposed judgment. The Attorney General will con- Case Title: United States of America and the State of Texas v. Kirby In- sider any written comments and may withdraw or withhold consent to land Marine, LP; Case No. 3:21-CV-00180, in the U.S. District Court the proposed agreed judgment if the comments disclose facts or consid- for the Southern District of Texas. -
May 3, 2021, HBR Alert
May 3, 2021, HBR Alert New COBRA Subsidies under the American Rescue Plan Act On March 23 the State Health Plan released an HBR Alert highlighting the new COBRA subsidies included in the American Rescue Plan Act of 2021. On April 20, the Plan provided additional guidance around notification and attestation. Guidance related to employer reimbursement for the subsidies is still forthcoming. With this update, the Plan intends to address how and who the Plan will communicate with at the employing unit about ongoing individual eligibility, reporting and reimbursements. Ongoing Communications about Eligible Members, Reporting & Plan Reimbursement While the programs are not identical by any means, the processes to support this initiative are somewhat similar to what is needed to meet the federal government’s 1095 reporting requirements; therefore, the Plan is going to build the ongoing communication plan around the employing unit contacts currently established for the 1095 process. For those employing units that do not utilize any of the Plan’s 1095 solutions, the Plan intends to contact the employing units’ Dependent Eligibility Verification Audit (DEVA) contact. The Office of State Controller will be the primary contact for all state agencies. If an employing unit would prefer to establish a new contact for the Plan to work with to support ongoing eligibility, reporting and reimbursement for the COBRA subsidies included in the American Rescue Plan Act of 2021, the employing unit should email contact information to [email protected]. Still to Come The Plan still has a lot of details to refine so there will be more information coming about the initial notice and validation process. -

Pricing*, Pool and Payment** Due Dates January - December 2021 Mideast Marketing Area Federal Order No
Pricing*, Pool and Payment** Due Dates January - December 2021 Mideast Marketing Area Federal Order No. 33 Class & Market Administrator Payment Dates for Producer Milk Component Final Pool Producer Advance Prices Payment Dates Final Payment Due Partial Payment Due Pool Month Prices Release Date Payrolls Due & Pricing Factors PSF, Admin., MS Cooperative Nonmember Cooperative Nonmember January February 3 * February 13 February 22 December 23, 2020 February 16 ** February 16 February 17 Janaury 25 January 26 February March 3 * March 13 March 22 January 21 * March 15 March 16 March 17 February 25 February 26 March March 31 * April 13 April 22 February 18 * April 15 April 16 April 19 ** March 25 March 26 April May 5 May 13 May 22 March 17 * May 17 ** May 17 ** May 17 April 26 ** April 26 May June 3 * June 13 June 22 April 21 * June 15 June 16 June 17 May 25 May 26 June June 30 * July 13 July 22 May 19 * July 15 July 16 July 19 ** June 25 June 28 ** July August 4 * August 13 August 22 June 23 August 16 ** August 16 August 17 July 26 ** July 26 August September 1 * September 13 September 22 July 21 * September 15 September 16 September 17 August 25 August 26 September September 29 * October 13 October 22 August 18 * October 15 October 18 ** October 18 ** September 27 ** September 27 ** October November 3 * November 13 November 22 September 22 * November 15 November 16 November 17 October 25 October 26 November December 1 * December 13 December 22 October 20 * December 15 December 16 December 17 November 26 ** November 26 December January 5, 2022 January 13, 2022 January 22, 2022 November 17 * January 18, 2022 ** January 18, 2022 ** January 18, 2022 ** December 27 ** December 27 ** * If the release date does not fall on the 5th (Class & Component Prices) or 23rd (Advance Prices & Pricing Factors), the most current release preceding will be used in the price calculation. -

March 13, 2020 Disaster Proclamation
GOVERNOR GREG ABBOTT March 13, 2020 FILED IN THE OFFCE OF THE SECRETARY OF STATE IhZo M”O’CL0CK The Honorable Ruth R. Hughs 470 Secretary of State State Capitol Room YE.8 Se re ry of State Austin, Texas 78701 Dear Secretary Hughs: Pursuant to his powers as Governor of the State of Texas, Greg Abbott has issued the following: A proclamation certifying that COVID-1 9 poses an imminent threat of disaster in the state and declaring a state of disaster for all counties in Texas. The original proclamation is attached to this letter of transmittal. Governor GSD/gsd Attachment Posi OFFICE Box 12428 AUSTIN, TEXAS 78711 512-463-2000 (VoicE) DIAL 7-1-1 foR RELAY SERVICES PROCLAMATION BY THE (!i1nrtwr uftiittfr ufxuz TO ALL TO WHOM THESE PRESENTS SHALL COME: WHEREAS, the novel coronavirus (COVID-19) has been recognized globally as a contagious respiratory virus; and WHEREAS, as of March 13, 2020, there are more than 30 confirmed cases of COVID-l 9 located in multiple Texas counties; and WHEREAS, there are more than 50 Texans with pending tests for COVID-19 in Texas; and WHEREAS, some schools, universities, and other governmental entities are beginning to alter their schedules, and some venues are beginning to temporarily close, as precautionary responses to the increasing presence of COVID- 19 in Texas; and WHEREAS, costs incurred to prepare for and respond to COVID-19 are beginning to mount at the state and local levels; and WHEREAS, the State of Texas has already taken numerous steps to prepare for COVID 19, such as increasing laboratory testing capacity, coordinating preparedness efforts across state agencies, and working with local partners to promote appropriate mitigation efforts; and WHEREAS, it is critical to take additional steps to prepare for, respond to, and mitigate the spread of COVID-19 to protect the health and welfare of Texans; and WHEREAS, declaring a state of disaster will facilitate and expedite the use and deployment of resources to enhance preparedness and response. -

Early Dance Division Calendar 17-18
Early Dance Division 2017-2018 Session 1 September 9 – November 3 Monday Classes Tuesday Classes September 11 Class September 12 Class September 18 Class September 19 Class September 25 Class September 26 Class October 2 Class October 3 Class October 9 Class October 10 Class October 16 Class October 17 Class October 23 Class October 24 Class October 30 Last Class October 31 Last Class Wednesday Classes Thursday Classes September 13 Class September 14 Class September 20 Class September 21* Class September 27 Class September 28 Class October 4 Class October 5 Class October 11 Class October 12 Class October 18 Class October 19 Class October 25 Class October 26 Class November 1 Last Class November 2 Last Class Saturday Classes Sunday Classes September 9 Class September 10 Class September 16 Class September 17 Class September 23 Class September 24 Class September 30* Class October 1 Class October 7 Class October 8 Class October 14 Class October 15 Class October 21 Class October 22 Class October 28 Last Class October 29 Last Class *Absences due to the holiday will be granted an additional make-up class. Early Dance Division 2017-2018 Session 2 November 4 – January 22 Monday Classes Tuesday Classes November 6 Class November 7 Class November 13 Class November 14 Class November 20 No Class November 21 No Class November 27 Class November 28 Class December 4 Class December 5 Class December 11 Class December 12 Class December 18 Class December 19 Class December 25 No Class December 26 No Class January 1 No Class January 2 No Class January 8 Class -

2021 Calandar
Harbortown Point Marina Resort & Club 2021 Reservation Calendar Written request can be taken at dates indicated Please note: you can only book in Prime season if you own in Prime Season and only below. The dates inform book in High Season if you own in High Season you when the 2021 weeks to the left Friday Saturday Sunday become abailable to Week No. Dates Dates Dates reserve. 1 Jan 1 - Jan 8 Jan 2 - Jan 9 Jan 3 - Jan 10 October 22, 2019 2 Jan 8 - Jan 15 Jan 9 - Jan 16 Jan 10 - Jan 17 October 29, 2019 3 Jan 15 - Jan 22 Jan 16 - Jan 23 Jan 17 - Jan 24 November 5, 2019 4 Jan 22 - Jan 29 Jan 23 - Jan 30 Jan 24 - Jan 31 November 12, 2019 5 Jan 29 - Feb 5 Jan 30 - Feb 6 Jan 31 - Feb 7 November 19, 2019 6 Feb 5 - Feb 12 Feb 6- Feb 13 Feb 7 - Feb 14 November 26, 2019 7 Feb 12 - Feb 19 Feb 13 - Feb 20 Feb 14 - Feb 21 December 3, 2019 8 Feb 19 - Feb 26 Feb 20 - Feb 27 Feb 21 - Feb 28 December 10, 2019 9 Feb 26 - Mar 5 Feb 27 - Mar 6 Feb 28 - Mar 7 December 18, 2018 HIGH 10 Mar 5 - Mar 12 Mar 6 - Mar 13 Mar 7 - Mar 14 December 17, 2019 11 Mar 12 - Mar 19 Mar 13 - Mar 20 Mar 14 - Mar21 December 24, 2019 12 Mar 19 - Mar 26 Mar 20 - Mar 27 Mar 21 - Mar 28 December 31, 2019 13 Mar 26 - Apr 2 Mar 27 - Apr 3 Mar 28 - Apr 4 January 7, 2020 14 April 2 - April 9 April 3 - April 10 April 4 - April 11 January 14, 2020 15 April 9 - April 16 Apr 10 - Apr 17 Apr 11 - Apr 18 January 21, 2020 16 April 16 - April 23 Apr 17 - Apr 24 Apr 18 - Apr 25 January 28, 2020 17 April 23 - April 30 Apr 24 - May 1 Apr 25 - May 2 February 4, 2020 18 Apr 30 - May 7 May 1 - May -

2021-2022 Custom & Standard Information Due Dates
2021-2022 CUSTOM & STANDARD INFORMATION DUE DATES Desired Cover All Desired Cover All Delivery Date Info. Due Text Due Delivery Date Info. Due Text Due May 31 No Deliveries No Deliveries July 19 April 12 May 10 June 1 February 23 March 23 July 20 April 13 May 11 June 2 February 24 March 24 July 21 April 14 May 12 June 3 February 25 March 25 July 22 April 15 May 13 June 4 February 26 March 26 July 23 April 16 May 14 June 7 March 1 March 29 July 26 April 19 May 17 June 8 March 2 March 30 July 27 April 20 May 18 June 9 March 3 March 31 July 28 April 21 May 19 June 10 March 4 April 1 July 29 April 22 May 20 June 11 March 5 April 2 July 30 April 23 May 21 June 14 March 8 April 5 August 2 April 26 May 24 June 15 March 9 April 6 August 3 April 27 May 25 June 16 March 10 April 7 August 4 April 28 May 26 June 17 March 11 April 8 August 5 April 29 May 27 June 18 March 12 April 9 August 6 April 30 May 28 June 21 March 15 April 12 August 9 May 3 May 28 June 22 March 16 April 13 August 10 May 4 June 1 June 23 March 17 April 14 August 11 May 5 June 2 June 24 March 18 April 15 August 12 May 6 June 3 June 25 March 19 April 16 August 13 May 7 June 4 June 28 March 22 April 19 August 16 May 10 June 7 June 29 March 23 April 20 August 17 May 11 June 8 June 30 March 24 April 21 August 18 May 12 June 9 July 1 March 25 April 22 August 19 May 13 June 10 July 2 March 26 April 23 August 20 May 14 June 11 July 5 March 29 April 26 August 23 May 17 June 14 July 6 March 30 April 27 August 24 May 18 June 15 July 7 March 31 April 28 August 25 May 19 June 16 July 8 April 1 April 29 August 26 May 20 June 17 July 9 April 2 April 30 August 27 May 21 June 18 July 12 April 5 May 3 August 30 May 24 June 21 July 13 April 6 May 4 August 31 May 25 June 22 July 14 April 7 May 5 September 1 May 26 June 23 July 15 April 8 May 6 September 2 May 27 June 24 July 16 April 9 May 7 September 3 May 28 June 25.