Mumps: Questions and Answers Q&A Information About the Disease and Vaccines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Communicable Disease Chart
COMMON INFECTIOUS ILLNESSES From birth to age 18 Disease, illness or organism Incubation period How is it spread? When is a child most contagious? When can a child return to the Report to county How to prevent spreading infection (management of conditions)*** (How long after childcare center or school? health department* contact does illness develop?) To prevent the spread of organisms associated with common infections, practice frequent hand hygiene, cover mouth and nose when coughing and sneezing, and stay up to date with immunizations. Bronchiolitis, bronchitis, Variable Contact with droplets from nose, eyes or Variable, often from the day before No restriction unless child has fever, NO common cold, croup, mouth of infected person; some viruses can symptoms begin to 5 days after onset or is too uncomfortable, fatigued ear infection, pneumonia, live on surfaces (toys, tissues, doorknobs) or ill to participate in activities sinus infection and most for several hours (center unable to accommodate sore throats (respiratory diseases child’s increased need for comfort caused by many different viruses and rest) and occasionally bacteria) Cold sore 2 days to 2 weeks Direct contact with infected lesions or oral While lesions are present When active lesions are no longer NO Avoid kissing and sharing drinks or utensils. (Herpes simplex virus) secretions (drooling, kissing, thumb sucking) present in children who do not have control of oral secretions (drooling); no exclusions for other children Conjunctivitis Variable, usually 24 to Highly contagious; -

Juvenile Recurrent Parotitis and Sialolithiasis: an Noteworthy Co-Existence
Otolaryngology Open Access Journal ISSN: 2476-2490 Juvenile Recurrent Parotitis and Sialolithiasis: An Noteworthy Co-Existence Venkata NR* and Sanjay H Case Report Department of ENT and Head & Neck Surgery, Kohinoor Hospital, India Volume 3 Issue 1 Received Date: April 20, 2018 *Corresponding author: Nataraj Rajanala Venkata, Department of ENT and Head & Published Date: May 21, 2018 Neck Surgery, Kohinoor Hospital, Kurla (W), Mumbai, India, Tel: +918691085580; DOI: 10.23880/ooaj-16000168 Email: [email protected] Abstract Juvenile Recurrent Parotitis is a relatively rare condition. Sialolithiasis co-existing along with Juvenile Recurrent Parotitis is an even rarer occurrence. We present a case of Juvenile Recurrent Parotitis and Sialolithiasis in a 6 years old male child and how we managed it. Keywords: Juvenile Recurrent Parotitis; Parotid gland; Swelling; Sialolithiasis Introduction child. Tuberculosis was suspected but the tests yielded no results. Even MRI of the parotid gland failed to reveal any Juvenile Recurrent Parotitis is characterized by cause. Then the patient was referred to us for definitive recurring episodes of swelling usually accompanied by management. Taking the history into consideration, a pain in the parotid gland. Associated symptoms usually probable diagnosis of Juvenile Recurrent Parotitis due to include fever and malaise. It is most commonly seen in sialectasis was considered. CT Sialography revealed children, but may persist into adulthood. Unlike parotitis, dilatation of the main duct and the ductules with which is caused by infection or obstructive causes like collection of the dye at the termination of the terminal calculi, fibromucinous plugs, duct stenosis and foreign ductules, in the left parotid gland. -

Mumps Virus Pathogenesis Clinical Features
Mumps Mumps Mumps is an acute viral illness. Parotitis and orchitis were described by Hippocrates in the 5th century BCE. In 1934, Johnson and Goodpasture showed that mumps could be transmitted from infected patients to rhesus monkeys and demonstrated that mumps was caused by a filterable agent present in saliva. This agent was later shown to be a virus. Mumps was a frequent cause of outbreaks among military personnel in the prevaccine era, and was one of the most common causes of aseptic meningitis and sensorineural deafness in childhood. During World War I, only influenza and gonorrhea were more common causes of hospitalization among soldiers. Outbreaks of mumps have been reported among military personnel as recently as 1986. Mumps Virus Mumps virus is a paramyxovirus in the same group as parainfluenza and Newcastle disease virus. Parainfluenza and Newcastle disease viruses produce antibodies that cross- 11 react with mumps virus. The virus has a single-stranded RNA genome. The virus can be isolated or propagated in cultures of various human and monkey tissues and in embryonated eggs. It has been recovered from the saliva, cerebrospinal fluid, urine, blood, milk, and infected tissues of patients with mumps. Mumps virus is rapidly inactivated by formalin, ether, chloroform, heat, and ultraviolet light. Pathogenesis The virus is acquired by respiratory droplets. It replicates in the nasopharynx and regional lymph nodes. After 12–25 days a viremia occurs, which lasts from 3 to 5 days. During the viremia, the virus spreads to multiple tissues, including the meninges, and glands such as the salivary, pancreas, testes, and ovaries. -

Orofacial Manifestations of COVID-19: a Brief Review of the Published Literature
CRITICAL REVIEW Oral Pathology Orofacial manifestations of COVID-19: a brief review of the published literature Esam HALBOUB(a) Abstract: Coronavirus disease 2019 (COVID-19) has spread Sadeq Ali AL-MAWERI(b) exponentially across the world. The typical manifestations of Rawan Hejji ALANAZI(c) COVID-19 include fever, dry cough, headache and fatigue. However, Nashwan Mohammed QAID(d) atypical presentations of COVID-19 are being increasingly reported. Saleem ABDULRAB(e) Recently, a number of studies have recognized various mucocutaneous manifestations associated with COVID-19. This study sought to (a) Jazan University, College of Dentistry, summarize the available literature and provide an overview of the Department of Maxillofacial Surgery and potential orofacial manifestations of COVID-19. An online literature Diagnostic Sciences, Jazan, Saudi Arabia. search in the PubMed and Scopus databases was conducted to retrieve (b) AlFarabi College of Dentistry and Nursing, the relevant studies published up to July 2020. Original studies Department of Oral Medicine and published in English that reported orofacial manifestations in patients Diagnostic Sciences, Riyadh, Saudi Arabia. with laboratory-confirmed COVID-19 were included; this yielded 16 (c) AlFarabi College of Dentistry and Nursing, articles involving 25 COVID-19-positive patients. The results showed a Department of Oral Medicine and Diagnostic Sciences, Riyadh, Saudi Arabia. marked heterogeneity in COVID-19-associated orofacial manifestations. The most common orofacial manifestations were ulcerative lesions, (d) AlFarabi College of Dentistry and Nursing, Department of Restorative Dental Sciences, vesiculobullous/macular lesions, and acute sialadentitis of the parotid Riyadh, Saudi Arabia. gland (parotitis). In four cases, oral manifestations were the first signs of (e) Primary Health Care Corporation, Madinat COVID-19. -

Oral Manifestations of Systemic Disease Their Clinical Practice
ARTICLE Oral manifestations of systemic disease ©corbac40/iStock/Getty Plus Images S. R. Porter,1 V. Mercadente2 and S. Fedele3 provide a succinct review of oral mucosal and salivary gland disorders that may arise as a consequence of systemic disease. While the majority of disorders of the mouth are centred upon the focus of therapy; and/or 3) the dominant cause of a lessening of the direct action of plaque, the oral tissues can be subject to change affected person’s quality of life. The oral features that an oral healthcare or damage as a consequence of disease that predominantly affects provider may witness will often be dependent upon the nature of other body systems. Such oral manifestations of systemic disease their clinical practice. For example, specialists of paediatric dentistry can be highly variable in both frequency and presentation. As and orthodontics are likely to encounter the oral features of patients lifespan increases and medical care becomes ever more complex with congenital disease while those specialties allied to disease of and effective it is likely that the numbers of individuals with adulthood may see manifestations of infectious, immunologically- oral manifestations of systemic disease will continue to rise. mediated or malignant disease. The present article aims to provide This article provides a succinct review of oral manifestations a succinct review of the oral manifestations of systemic disease of of systemic disease. It focuses upon oral mucosal and salivary patients likely to attend oral medicine services. The review will focus gland disorders that may arise as a consequence of systemic upon disorders affecting the oral mucosa and salivary glands – as disease. -

ADVERSE FACTORS THAT CAN AFFECT on the COURSE of CHRONIC PARENCHIMATIC PAROTITIS in CHILDREN DOI: 10.36740/Wlek202006118
© Aluna Publishing Wiadomości Lekarskie, VOLUME LXXIII, ISSUE 6, JUNE 2020 ORIGINAL ARTICLE ADVERSE FACTORS THAT CAN AFFECT ON THE COURSE OF CHRONIC PARENCHIMATIC PAROTITIS IN CHILDREN DOI: 10.36740/WLek202006118 Pavlo I. Tkachenko, Serhii O. Bilokon, Yuliia V. Popelo, Nataliia M. Lokhmatova, Olha B. Dolenko, Nataliia M. Korotych UKRAINIAN MEDICAL STOMATOLOGICAL ACADEMY, POLTAVA, UKRAINE ABSTRACT The aim: The study of the presence of disorders in the ante- and postnatal periods of development of children from 2 months to 15 years with chronic parenchimatic parotitis, which may affect its course. Materials and methods: It has been examined and treated 88 children, aged from 2 months to 15 years with chronic parenchimatic parotitis, and their mothers were interviewed, who indicated the pathological course of pregnancy, childbirth and indicated the type of breastfeeding babbies. The scope of the survey included general, additional methods, consultations by related specialists and statistical processing of results. Results: 88 children with the exacerbation of chronic parenchimatic parotitis were examined (42 – (47%) with active course and 46 – (53%) with inactive). The exacerbation occurred on the background of acute infectious processes or coincided with the exacerbation of one of the chronic diseases. The first manifestations occurred in spring (55%) and autumn (36%) periods, 44% of children were hospitalized with other diagnoses. The presence of pathological conditions during pregnancy and birth defects in their mothers were recorded more often 3,5 and 3,3 times, respectively, compared with control. 70% of children received mixed and artificial feeding and were more likely to become ill. Conclusions: The severity of clinical manifestations of inflammation and disorders of the general condition depended on the activity of the course of chronic parenchimatic parotitis and were more pronounced when active. -

Measles, Mumps, and Rubella
Measles, Mumps, and Rubella Developed by Vini Vijayan, MD, in collaboration with the ANGELS Team. Last reviewed by Vini Vijayan, MD, January 24, 2017. Because measles, mumps, and rubella can be prevented by a combination vaccine, all 3 of these illnesses are discussed in this Guideline. The following vaccines are available in the United States: Live measles, mumps, and rubella virus vaccine (MMR) Live measles, mumps, rubella, and varicella virus vaccine (MMRV) MEASLES (RUBEOLA) Key Points Measles, also called rubeola or red measles, is a highly contagious viral illness characterized by fever, malaise, rash, cough, coryza (runny nose), and conjunctivitis. Measles is a leading cause of morbidity and mortality in developing countries. Over the past decade measles has been making a resurgence in the United States. Vaccination with MMR or MMRV is highly effective in preventing the disease. Introduction The Virus The measles virus is a single-stranded, enveloped ribonucleic acid (RNA) virus of the genus Morbillivirus within the family Paramyxoviridae. 1 The virus enters the respiratory epithelium of the nasopharynx and regional lymph nodes resulting in viremia and dissemination to the skin, respiratory tract, and other organs. The peak incidence of measles in temperate areas is late winter and early spring. Transmission Measles is a highly contagious virus with an estimated 90% secondary infection rate in susceptible domestic contacts. Measles is spread by droplets from respiratory secretions and close personal contact or direct contact with infected nasal or throat secretions. Measles virus can be transmitted by an infected person from 4 days prior to the onset of the rash to 4 days after the rash erupts. -

Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases
Journal of Clinical Medicine Review Oral Complications of ICU Patients with COVID-19: Case-Series and Review of Two Hundred Ten Cases Barbora Hocková 1,2,†, Abanoub Riad 3,4,*,† , Jozef Valky 5, Zuzana Šulajová 5, Adam Stebel 1, Rastislav Slávik 1, Zuzana Beˇcková 6,7, Andrea Pokorná 3,8 , Jitka Klugarová 3,4 and Miloslav Klugar 3,4 1 Department of Maxillofacial Surgery, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] (B.H.); [email protected] (A.S.); [email protected] (R.S.) 2 Department of Prosthetic Dentistry, Faculty of Medicine and Dentistry, Palacky University, 775 15 Olomouc, Czech Republic 3 Czech National Centre for Evidence-Based Healthcare and Knowledge Translation (Cochrane Czech Republic, Czech EBHC: JBI Centre of Excellence, Masaryk University GRADE Centre), Institute of Biostatistics and Analyses, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic; [email protected] (A.P.); [email protected] (J.K.); [email protected] (M.K.) 4 Department of Public Health, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic 5 Department of Anaesthesiology, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] (J.V.); [email protected] (Z.Š.) 6 Department of Clinical Microbiology, F. D. Roosevelt University Hospital, 975 17 Banska Bystrica, Slovakia; [email protected] 7 St. Elizabeth University of Health and Social Work, 812 50 Bratislava, Slovakia 8 Department of Nursing and Midwifery, Faculty of Medicine, Masaryk University, 625 00 Brno, Czech Republic * Correspondence: [email protected]; Tel.: +420-721-046-024 † These authors contributed equally to this work. -

Measles, Mumps and Rubella Gone but Not Forgotten
Measles, mumps and rubella Gone but not forgotten David Isaacs Measles z Highly infectious human disease z 1 in 15 cases develop complications – otitis me dia, pneumoni a, encephalitis, SSPE z Pre vaccine epidemiology – 2 - 5 year cycle of epidemics – most common in 5 - 9 year olds – world wide 7 - 8 million deaths annually Measles z 99.9% of unimmunised children get measles z 1 in 5,000 to 10,000 cases die z Mortality : 888,000 deaths in 1998 (more than breast cancer, violence) z Morbidity : encephalitis (0.1%), convulsions ((%),p0.5%), pneumonia (1-7%), otitis media (5-9%) Measles: a global perspective z Vaccine available for over 40 years z Still caused 197,000 estimated deaths in 2007 – leading vaccine preventable killer of children z Highest disease incidence in Africa z Most deaths (98%) are in poorest countries – low vaccination coverage, high case fatality ratio Measles in Australia 1200 Notifications 60 Hospitalisations 50 1000 40 2001 – young 30 adults program Number 20 800 10 rr 0 Jan Jan Jan Jan Jan Jan Jan Jan Jan 600 2000 2001 2002 2003 2004 2005 2006 2007 2008 Month Numbe 400 200 0 Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan Jan 1993 1994 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 Month Nov 1993 – 2nd dose Jul 1998 – 2nd dose moved to 4-5 yo introduced for 10-16 yo Measles Control Campaign conducted Measles elimination in Australia: 1 The Meas les Con tro l campa ign (MCC) – July-December 1998 – mass vaccination 1.7 million primary school children (96% vaccinated) – reminder letter -
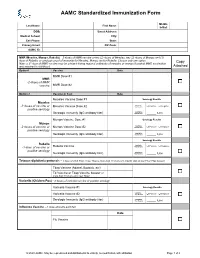
AAMC Standardized Immunization Form
AAMC Standardized Immunization Form Middle Last Name: First Name: Initial: DOB: Street Address: Medical School: City: Cell Phone: State: Primary Email: ZIP Code: AAMC ID: MMR (Measles, Mumps, Rubella) – 2 doses of MMR vaccine or two (2) doses of Measles, two (2) doses of Mumps and (1) dose of Rubella; or serologic proof of immunity for Measles, Mumps and/or Rubella. Choose only one option. Copy Note: a 3rd dose of MMR vaccine may be advised during regional outbreaks of measles or mumps if original MMR vaccination was received in childhood. Attached Option1 Vaccine Date MMR Dose #1 MMR -2 doses of MMR vaccine MMR Dose #2 Option 2 Vaccine or Test Date Measles Vaccine Dose #1 Serology Results Measles Qualitative -2 doses of vaccine or Measles Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Mumps Vaccine Dose #1 Serology Results Mumps Qualitative -2 doses of vaccine or Mumps Vaccine Dose #2 Titer Results: Positive Negative positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Serology Results Rubella Qualitative Positive Negative -1 dose of vaccine or Rubella Vaccine Titer Results: positive serology Quantitative Serologic Immunity (IgG antibody titer) Titer Results: _____ IU/ml Tetanus-diphtheria-pertussis – 1 dose of adult Tdap; if last Tdap is more than 10 years old, provide date of last Td or Tdap booster Tdap Vaccine (Adacel, Boostrix, etc) Td Vaccine or Tdap Vaccine booster (if more than 10 years since last Tdap) Varicella (Chicken Pox) - 2 doses of varicella vaccine or positive serology Varicella Vaccine #1 Serology Results Qualitative Varicella Vaccine #2 Titer Results: Positive Negative Serologic Immunity (IgG antibody titer) Quantitative Titer Results: _____ IU/ml Influenza Vaccine --1 dose annually each fall Date Flu Vaccine © 2020 AAMC. -
Viruses in Transplantation - Not Always Enemies
Viruses in transplantation - not always enemies Virome and transplantation ECCMID 2018 - Madrid Prof. Laurent Kaiser Head Division of Infectious Diseases Laboratory of Virology Geneva Center for Emerging Viral Diseases University Hospital of Geneva ESCMID eLibrary © by author Conflict of interest None ESCMID eLibrary © by author The human virome: definition? Repertoire of viruses found on the surface of/inside any body fluid/tissue • Eukaryotic DNA and RNA viruses • Prokaryotic DNA and RNA viruses (phages) 25 • The “main” viral community (up to 10 bacteriophages in humans) Haynes M. 2011, Metagenomic of the human body • Endogenous viral elements integrated into host chromosomes (8% of the human genome) • NGS is shaping the definition Rascovan N et al. Annu Rev Microbiol 2016;70:125-41 Popgeorgiev N et al. Intervirology 2013;56:395-412 Norman JM et al. Cell 2015;160:447-60 ESCMID eLibraryFoxman EF et al. Nat Rev Microbiol 2011;9:254-64 © by author Viruses routinely known to cause diseases (non exhaustive) Upper resp./oropharyngeal HSV 1 Influenza CNS Mumps virus Rhinovirus JC virus RSV Eye Herpes viruses Parainfluenza HSV Measles Coronavirus Adenovirus LCM virus Cytomegalovirus Flaviviruses Rabies HHV6 Poliovirus Heart Lower respiratory HTLV-1 Coxsackie B virus Rhinoviruses Parainfluenza virus HIV Coronaviruses Respiratory syncytial virus Parainfluenza virus Adenovirus Respiratory syncytial virus Coronaviruses Gastro-intestinal Influenza virus type A and B Human Bocavirus 1 Adenovirus Hepatitis virus type A, B, C, D, E Those that cause -

Infection Prevention News & Updates
APRIL 2018 INFECTION PREVENTION NEWS & UPDATES FAST FACTS HEPATITIS A Hepatitis A outbreaks continue to occur as the global prevalence appears Severity to be rapidly increasing. Victoria Australia is seeing its outbreak grow with MULTI-COUNTRY OUTBREAK 58 confirmed cases, 7 probably cases, 16 cases under early investigation, and one death. Being homeless or an IV drug user is associated with a higher probability of becoming infected. The initial laboratory analysis suggests the strain is similar to a strain circulating in Europe, suggesting Transmission CONTACT there is a travel associated case linking the outbreaks. The outbreak in Kentucky in the US is continuing to grow with 150 cases, 124 of which are in the greater Louisville area. As with other outbreaks, the homeless and IV drug users are at a higher risk of getting disease. The Utah outbreak has 217 confirmed cases. Genetic sequencing of the virus has shown that the Arizona and California outbreaks reported previously are tied to these outbreaks as well. Location AUSTRALIA, USA Hepatitis A is an infection that causes an inflammation of the liver. There are a number of viruses that can cause Hepatitis including Hepatitis A, Hepatitis B, and Hepatitis C, with vaccinations available for Hepatitis A and Hepatitis B. Hepatitis A is passed to other people through contact with infected feces, or if an infected person touches objects after using the toilet and not washing their hands, including contaminating food or drink from contact with contaminated hands, so handwashing and surface disinfection are important interventions to prevent the spread of the virus. It can also be spread by sexual contact.