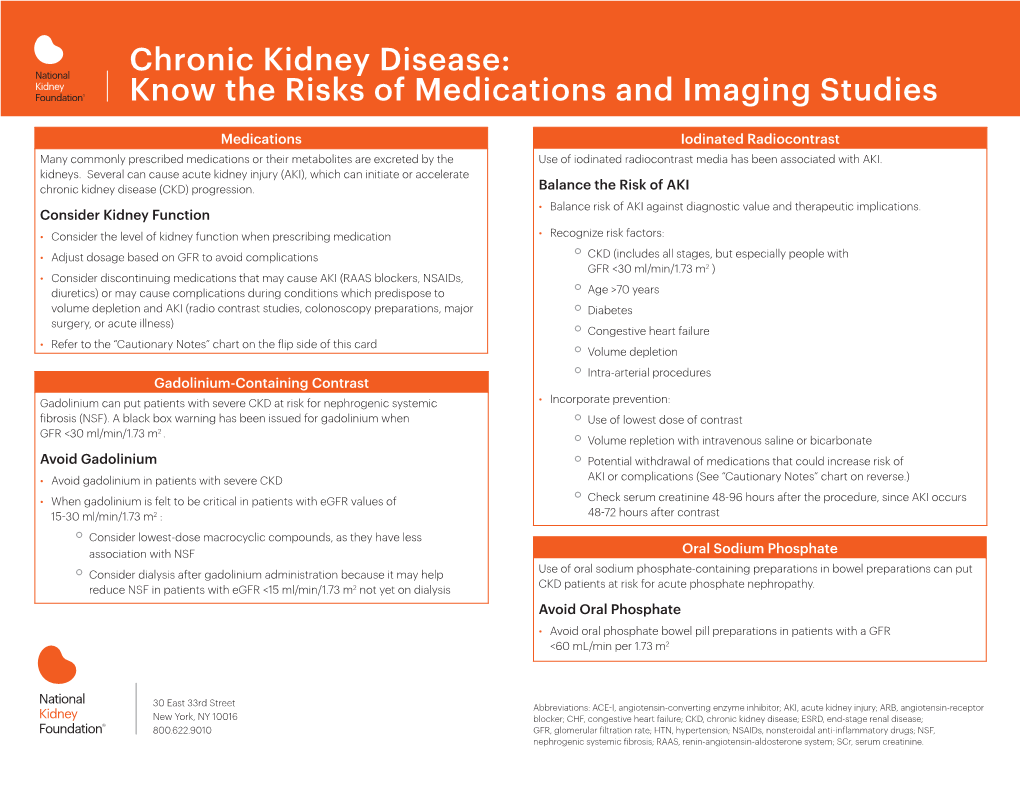
Chronic Kidney Disease: Know the Risks of Medications and Imaging Studies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Acute Phosphate Nephropathy Alexander K
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector http://www.kidney-international.org the renal consult & 2009 International Society of Nephrology Acute phosphate nephropathy Alexander K. Rocuts1, Sushrut S. Waikar1, Mariam P. Alexander1,2, Helmut G. Rennke2 and Ajay K. Singh1 1Renal Division, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA and 2Department of Pathology, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA minute. The rest of the examination was unremarkable. CASE PRESENTATION HerlaboratorydataissummarizedinTable1. A 60-year-old white Latino female with a clinical diagnosis A postoperative kidney ultrasound showed no of diabetes mellitus (diagnosed in 1993) and hypertension hydronephrosis. was referred to the chronic kidney disease clinic at The etiology of the acute kidney injury was unclear. Brigham and Women’s Hospital for the evaluation of acute Progressive diabetic nephropathy exacerbated by other kidney injury; serum creatinine had increased from a contributory factors, such as exposure to lisinopril, baseline of 0.9 to 1.5 mg/dl in a 11-week period. She was acetylsalicylic acid, or naproxen, was regarded as the most asymptomatic at the time of presentation. Her past plausible explanation. Despite discontinuation of these medical history included a total abdominal hysterectomy medications, kidney function did not improve; it worsened with bilateral salpingo oophorectomy and upper in a 4-week period after presentation. Hence, a kidney vaginectomy for high-grade squamous intraepithelial biopsy was performed. lesion of the cervix, 11 weeks prior to presentation. Three weeks prior to presentation (8 weeks after surgery) and within a week of each other, she was evaluated for two consecutive episodes of acute onset of chest pain with pulmonary edema in the setting of severe hypertension. -

Update in Acute Kidney Injury
UPDATE IN ACUTE KIDNEY INJURY Emily Robinson, MD, MPH Instructor in Medicine, HMS Renal Division, BWH October 1, 2020 Disclosures ■ Nothing to disclose Case: Etiology of obstruction ■ 35 yo male with a congenital solitary kidney ■ Baseline Cr 1.2mg/dl ■ Presents to ER in severe pain ■ Ultrasound shows hydronephrosis ■ Labs show a creatinine increase to 2.7mg/dl *Based on his age alone, what is the most likely etiology of the obstruction? ■ A. Kidney stone ■ B. Prostatic obstruction ■ C. Retroperitoneal neoplastic disease ■ D. Anatomic abnormality Based on his age alone, what is the most likely etiology of the obstruction? ■ A. Kidney stone ■ B. Prostatic obstruction ■ C. Retroperitoneal neoplastic disease ■ D. Anatomic abnormality Most Common Causes of Obstruction by Age ■ Children – Anatomic abnormalities ■ Young Adults – Kidney stones ■ Older Adults – Prostatic obstruction – Retroperitoneal or pelvic neoplasms – Kidney stones Case: The “Negative” Urinalysis ■ 65 yo female presents to her PCP feeling “unwell” for 3 weeks with poor PO intake ■ Labs checked and Cr 3.7 ■ She is referred to the ER and admitted for AKI, started on IV fluids ■ Amongst other workup, a urinalysis is performed and the dipstick is reported as “negative” with no blood, protein, leukocytes, or nitrites *Which of the following is NOT in your differential given this urinalysis? ■ A. Myeloma cast nephropathy ■ B. Dehydration due to poor PO intake ■ C. Tumor lysis syndrome from a new lymphoma ■ D. Rhabdomyolysis Which of the following is NOT in your differential given this urinalysis? ■ A. Myeloma cast nephropathy ■ B. Dehydration due to poor PO intake ■ C. Tumor lysis syndrome from a new lymphoma ■ D. -
2012 CKD Guideline
OFFICIAL JOURNAL OF THE INTERNATIONAL SOCIETY OF NEPHROLOGY KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease VOLUME 3 | ISSUE 1 | JANUARY 2013 http://www.kidney-international.org KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease KDIGO gratefully acknowledges the following consortium of sponsors that make our initiatives possible: Abbott, Amgen, Bayer Schering Pharma, Belo Foundation, Bristol-Myers Squibb, Chugai Pharmaceutical, Coca-Cola Company, Dole Food Company, Fresenius Medical Care, Genzyme, Hoffmann-LaRoche, JC Penney, Kyowa Hakko Kirin, NATCO—The Organization for Transplant Professionals, NKF-Board of Directors, Novartis, Pharmacosmos, PUMC Pharmaceutical, Robert and Jane Cizik Foundation, Shire, Takeda Pharmaceutical, Transwestern Commercial Services, Vifor Pharma, and Wyeth. Sponsorship Statement: KDIGO is supported by a consortium of sponsors and no funding is accepted for the development of specific guidelines. http://www.kidney-international.org contents & 2013 KDIGO VOL 3 | ISSUE 1 | JANUARY (1) 2013 KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease v Tables and Figures vii KDIGO Board Members viii Reference Keys x CKD Nomenclature xi Conversion Factors & HbA1c Conversion xii Abbreviations and Acronyms 1 Notice 2 Foreword 3 Work Group Membership 4 Abstract 5 Summary of Recommendation Statements 15 Introduction: The case for updating and context 19 Chapter 1: Definition, and classification -

Adverse Renal and Metabolic Effects Associated with Oral Sodium Phosphate Bowel Preparation
CJASN ePress. Published on July 2, 2008 as doi: 10.2215/CJN.02040408 In-Depth Review Adverse Renal and Metabolic Effects Associated with Oral Sodium Phosphate Bowel Preparation Eliot C. Heher,* Samuel O. Thier,*† Helmut Rennke,‡ and Benjamin D. Humphreys§ *Department of Medicine, Division of Nephrology, Massachusetts General Hospital, Boston, Massachusetts; †Department of Medicine and Healthcare Policy, Harvard Medical School, Boston, Massachusetts; ‡Renal Pathology and §Renal Division, Brigham and Women’s Hospital, Boston, Massachusetts Colorectal cancer can be prevented by the removal of adenomatous polyps during screening colonoscopy, but adequate bowel preparation is required. Oral sodium phosphate (OSP), an effective bowel purgative, is available over the counter and requires a substantially lower volume than polyethylene glycol-based preparative agents. Accumulating reports implicate OSP in electrolyte disturbances as well as acute kidney injury (AKI) in a syndrome termed phosphate nephropathy (a form of nephrocalcinosis). Despite published case reports and case series, the actual incidence, risk factors, and natural history of phosphate nephropathy remain largely undefined. Several recent observational studies have provided new information on these important issues while supporting a link between OSP and acute phosphate nephropathy as well as the development of chronic kidney disease in elderly patients, many of whom had a normal serum creatinine at the time of OSP ingestion. This review summarizes current knowledge about the renal complications of OSP, risk factors for its development, and the pathophysiology of acute and chronic kidney damage in nephrocalcinosis. Clin J Am Soc Nephrol ●●: ●●●-●●●, 2008. doi: 10.2215/CJN.02040408 pproximately 14 million colonoscopies are performed known as Nu-Lytely, formulated without the unpalatable in- in the United States yearly for colon cancer screening, gredient sodium sulfate, became available in 1990 (9). -

Renal Failure Due to Acute Phosphate Nephropathy
CAsE rEPorT renal failure due to acute phosphate nephropathy T.M. Slee1, L.J. Vleming2, R.M. Valentijn2* 1Department of Internal Medicine, Leiden University Medical Centre, Leiden, the Netherlands, 2Department of Internal Medicine, Haga Hospital, location Sportlaan, Sportlaan 600, 2566 MJ The Hague, the Netherlands, *corresponding author: tel.: +31 (0)70-312 62 00 ABsTract Case report of a 62-year-old woman who developed acute the use of oral sodium phosphate preparation is 1.14 to 2.35 renal failure due to nephrocalcinosis, also called acute (OR).1,2 The main reasons for not diagnosing this condition phosphate nephropathy, after large bowel cleansing in are unfamiliarity with this complication, the time lag between preparation for colonoscopy using oral sodium phosphate the ingestion of the drug and the onset of renal failure and the solution (Phosphoral, de Witt, Cheshire, UK). subsequently fact that the acute as well as the chronic renal failure which her renal insufficiency resolved only partially resulting results from this ingestion is not routinely checked for. in stage 4 chronic kidney disease. in retrospect multiple risk factors for this condition (hypertension, diuretics, AT-II receptor blocker, female gender, advanced age CAsE rEPorT and volume depleting due to vomiting and nausea) were identified. if these factors had been taken into A 62-year-old woman was referred to our dialysis centre consideration prior to prescribing this drug, acute for acute renal failure of three days duration, which did not and chronic renal failure would have been prevented. respond to conservative treatment and volume loading. future investigation of potential risk factors and the exact Her previous history was unremarkable with the mechanism of this complication is necessary to identify exception of a hysterectomy and hypertension, which was those patients prone to develop this complication. -

Towards the Incidence of Acute Phosphate Nephropathy
JASN Express. Published on November 14, 2007 as doi: 10.1681/ASN.2007101073 EDITORIALS www.jasn.org Towards the Incidence of significant but small percentage of patients who undergo colonoscopy develop mild, transient elevations in serum cre- Acute Phosphate Nephropathy atinine related to hypovolemia. In this study, the mean rise in serum creatinine among patients with AKI was only 0.41 Glen S. Markowitz,* Jai Radhakrishnan,† and mg/dl and no data on reversibility were available. In contrast, Vivette D. D’Agati* among the 21 cases of APhN we previously reported, the *Department of Pathology and †Department of Medicine, Ne- mean increase in serum creatinine was 2.9 mg/dl (mean base- phrology Division, Columbia University, College of Physicians & line, 1.0 mg/dl; mean peak, 3.9 mg/dl).2 The renal insuffi- Surgeons, New York, New York ciency was largely irreversible, with 4 patients progressing to J Am Soc Nephrol 18: 3020–3022, 2007. end-stage renal disease and a mean final creatinine of 2.4 doi: 10.1681/ASN.2007101073 mg/dl in the remaining 17 patients.2 When Brunelli et al. re-examined their data using a stricter definition of AKI that In 2003, Desmeules et al.1 reported a 71-yr-old female who de- requires a 1 mg/dl increase in serum creatinine, the number veloped acute renal failure after the use of an oral sodium phos- of patients with AKI declined from 116 to only 3.8 Thus, their phate (OSP) solution as bowel purgative before colonoscopy. study design is biased toward detection of relatively small Renal biopsy revealed tubular injury and abundant tubular cal- increments in serum creatinine that are not likely to repre- cium phosphate deposits, suggesting a pathophysiological link sent APhN. -

Sodium Phosphate Tablets and Acute Phosphate Nephropathy
nature publishing group THE RED SECTION 1903 see related editorial on page 1907 Sodium Phosphate Tablets and Acute Phosphate Nephropathy Ann Corken Mackey, RPh, MPH1, Lanh Green, PharmD, MPH1, Keith St Amand, MD1 and Mark Avigan, MD, CM1 Am J Gastroenterol 2009;104:1903–1906; doi:10.1038/ajg.2009.342 We report 10 cases of acute phosphate From July 2006 to September 2008, It has been documented in the litera- nephropathy (APN), associated with 10 cases of APN associated with SPT ture that maintaining adequate hydra- acute renal failure (ARF), following use for bowel cleansing were reported tion and dividing the two SP doses administration of sodium phosphate to the FDA’s Adverse Event Report- by 12 hours are important to prevent tablets (SPTs) that were used as a bowel ing System (AERS) database (Table 1; intravascular volume depletion and preparation before colonoscopy. SPTs patients 1–7 took Visicol and patients thereby minimize the risk of APN and were first approved by the US Food and 8–10 took OsmoPrep). Note that two ARF (9–11). The product labels for Drug Administration (FDA) in Septem- cases (patients 5 and 6 in Table 1) also Visicol and OsmoPrep recommend ber 2000 for bowel cleansing at a dose of have been reported in the literature; that patients take a total of at least 112 60 g (40 tablets) in two divided doses with no additional cases have been pub- ounces and 64 ounces of liquid, respec- adequate hydration (trade name Visi- lished (2,4). Renal biopsy in these 10 tively, and that divided doses be taken col). -

Orthophosphoric Acid and Inorganic Phosphate Compounds, Including Ortho- and Condensed Phosphates) (Various Casrns Included in the Text)
EPA/690/R-11/061F l Final 3-01-2011 Provisional Peer-Reviewed Toxicity Values for Inorganic Phosphates (Orthophosphoric Acid and Inorganic Phosphate Compounds, Including Ortho- and Condensed Phosphates) (Various CASRNs included in the text) Superfund Health Risk Technical Support Center National Center for Environmental Assessment Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 AUTHORS, CONTRIBUTORS, AND REVIEWERS CHEMICAL MANAGER Custodio V. Muianga, PhD, MPH National Center for Environmental Assessment, Cincinnati, OH DRAFT DOCUMENT PREPARED BY ICF International 9300 Lee Highway Fairfax, VA 22031 PRIMARY INTERNAL REVIEWERS Dan D. Petersen, PhD, DABT National Center for Environmental Assessment, Cincinnati, OH Anuradha Mudipalli, MSc, PhD National Center for Environmental Assessment, Research Triangle Park, NC This document was externally peer reviewed under contract to Eastern Research Group, Inc. 110 Hartwell Avenue Lexington, MA 02421-3136 Questions regarding the contents of this document may be directed to the U.S. EPA Office of Research and Development’s National Center for Environmental Assessment, Superfund Health Risk Technical Support Center (513-569-7300). TABLE OF CONTENTS COMMONLY USED ABBREVIATIONS .................................................................................... ii BACKGROUND .............................................................................................................................3 HISTORY ...................................................................................................................................3 -
Toxins and the Kidneys
Toxins and the Kidneys Panduranga S Rao MD DNB MS Associate Professor, Division of Nephrology Department of Medicine University of Michigan Case Presentation • 55 year old woman takes a variety of vitamin supplements, and recently purchased “Worry Free” • PMH: HTN, Hyperlipidemia • Medications: • OTC – Furosemide 20 mg daily – Ginseng – Simvastatin 40 mg daily – Blue Cohosh – Lisinopril 40 mg daily – Aspirin 81 mg daily Case Presentation • She asks you if its OK to take “Worry Free”. You tell her: A. Yes, but stop the Ginseng as it will cause hypokalemia B. No, “worry free” will increase hepatic P-450 activity and reduce the effectiveness of atorvastatin C. Yes, but stop the blue cohosh as it will worsen hypertension D. Because you’re 30 minutes behind schedule in clinic, you tell her you are not really sure, but it’s probably fine. Use of Complementary & Alternative Medicine (CAM) • 38% of Adults use CAM in 2007 – Women > Men, higher education, higher income http://nccam.nih.gov/news/camstats/2007/camsurvey_fs1.htm#use CAM: Don’t Ask CAM use in CV Disease CAM use in Renal Disease 60 60 Txp 50 50 HD 40 40 30 30 Percent Percent 20 20 10 10 0 0 MD Aware PharmD Asked Regularly Occasionally Never Aware about CAM Chagan et al. BMC Compl Alternative Medicine 2005, 5:4 CAM: Don’t Tell Oncology Patients • Reasons why patient’s 50 don’t tell 40 – Perceived lack of MD’s 30 20 Percent knowledge & interest 10 – Fear of termination of 0 therapy Using CAM Reported CAM Nephrology Patients – Perceived simplicity of 80 some of the CAM therapies 60 40 Percent 20 0 Ge et al. -
Histopathological Patterns of Nephrocalcinosis: a Phosphate Type Can Be Distinguished from a Calcium Type
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by RERO DOC Digital Library Nephrol Dial Transplant (2012) 27: 1122–1131 doi: 10.1093/ndt/gfr414 Advance Access publication 29 July 2011 Histopathological patterns of nephrocalcinosis: a phosphate type can be distinguished from a calcium type Thorsten Wiech1,2, Helmut Hopfer3, Ariana Gaspert4, Susanne Banyai-Falger5, Martin Hausberg6, Josef Schro¨der7, Martin Werner2 and Michael J. Mihatsch3 1Centre of Chronic Immunodeficiency, University Medical Center Freiburg, University of Freiburg, Freiburg, Germany, 2Institute of Pathology, University Hospital Freiburg, Freiburg, Germany, 3Institute for Pathology, University Hospital Basel, Basel, Switzerland, 4Institute of Surgical Pathology, University Hospital Zurich, Zurich, Switzerland, 5Klinik St Anna, Luzern, Switzerland, 6Sta¨dtisches Klinikum Karlsruhe, Karlsruhe, Germany and 7Institute of Pathology, University Hospital Regensburg, Regensburg, Germany Correspondence and offprint requests to: Thorsten Wiech; E-mail: [email protected] Abstract different chemical composition, such as calcium oxalate or Background. The etiology of nephrocalcinosis is variable. calcium phosphate, and can, but does not have to be associ- In this study, we wanted to elucidate whether the histopa- ated with nephrolithiasis. Pathologists distinguish between thological appearance of calcium phosphate deposits oxalosis and nephrocalcinosis, the latter again covering dif- provides information about possible etiology. ferent compositions but excluding calcium oxalate. Tradi- Methods. Autopsy cases from the years 1988 to 2007 and tionally, pathologists used the term ‘calcium nephrosis’ for native kidney biopsies from a 50-year period (1959–2008) dystrophic calcification i.e. calcification of necrosis and the with nephrocalcinosis were identified. The biopsy cases term ‘nephrocalcinosis’ for metastatic calcification [1]. -

Bowel Preps Tied to Phosphate Nephropathy Risk
26 DIGESTIVE DISORDERS JANUARY 1, 2009 • FAMILY PRACTICE NEWS Bowel Preps Tied to Phosphate Nephropathy Risk BY MIRIAM E. TUCKER sodium phosphate product (OSPs) for 2009, Dr. Charles Ganley, director of the acute kidney injury associated with these Senior Writer bowel cleansing. Although available data FDA’s Office of Nonprescription Prod- products, Dr. Joyce Korvick, deputy di- do not show a risk of acute kidney injury ucts, said in a telephone press briefing. rector of the FDA’s Division of Gastroen- he Food and Drug Administra- when the OTC products are taken at the The FDA has also directed Salix Phar- terology Products said at the briefing. tion has added a boxed warning lower doses for laxative use, when used maceuticals, maker of both products, to In 2006, the FDA issued a Science Paper Tto the prescription oral sodium at higher doses for bowel cleansing they develop a risk evaluation and mitigation and a Healthcare Professional sheet on the phosphate bowel preparation products are associated with the same risks as the strategy, distribute a Medication Guide to risks associated with the use of OSP prod- Visicol and OsmoPrep concerning the prescription OSP products. Boxed warn- alert patients to the risk of acute kidney ucts for bowel cleansing. Since then, the risk of acute phosphate nephropathy. ings are not used for OTC products, but injury associated with the use of OSP agency has received reports of acute phos- The agency is also recommending the agency plans to issue an amended la- products and conduct a postmarketing phate nephropathy with both prescrip- consumers not use over-the-counter oral bel for OTC OSP products by May of clinical trial to further assess the risk of tion and products available in the OTC set- ting, including 20 unique cases of kidney injury associated with the use of Osmo- Brief Summary—see package insert for full prescribing information. -

Histopathological Patterns of Nephrocalcinosis: a Phosphate Type Can Be Distinguished from a Calcium Type
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2012 Histopathological patterns of nephrocalcinosis: a phosphate type can be distinguished from a calcium type Wiech, T ; Hopfer, H ; Gaspert, A ; Banyai-Falger, S ; Hausberg, M ; Schröder, J ; Werner, M ; Mihatsch, M J Abstract: BACKGROUND: The etiology of nephrocalcinosis is variable. In this study, we wanted to elucidate whether the histopathological appearance of calcium phosphate deposits provides information about possible etiology. METHODS: Autopsy cases from the years 1988 to 2007 and native kidney biopsies from a 50-year period (1959-2008) with nephrocalcinosis were identified. The biopsy cases were re-evaluated by light microscopy. The autopsy cases were analysed according to the underlying disease. The biopsy cases were grouped with respect to the likely etiology of nephrocalcinosis. Total number, den- sity, localization, size and pattern of all calcification foci were documented and correlated with clinical and laboratory data. RESULTS: About 223 of 12 960 autopsy cases (1.7%) had nephrocalcinosis, 111 of which (49.8%) suffered from advanced malignant tumours. Nephrocalcinosis was the main diagnosis in 48 of 12 480 native kidney biopsies (0.4%). Clinicopathological correlation revealed a specific pat- tern of calcification associated with hyperphosphataemia and/or hyperphosphaturia: these cases showed predominant globular or shell-like calcifications (phosphate type). In contrast, the biopsies of thehy- percalcaemic/hypercalciuric group had a different predominant pattern with clumpy or finely granular calcifications (calcium type). CONCLUSIONS: Our results indicate that hyperphosphaturia-associated cases of nephrocalcinosis can be distinguished from hypercalciuria-associated cases histopathologically.