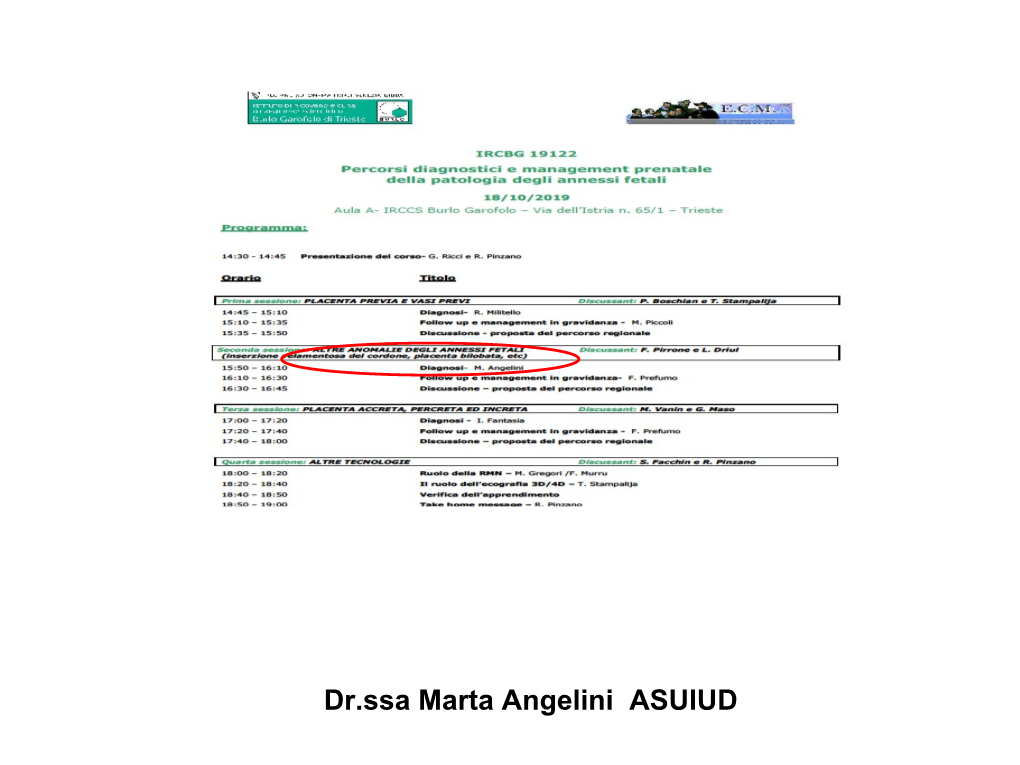
Dr.Ssa Marta Angelini ASUIUD Early Placental Development
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Placental Findings and Effect of Prophylactic Hydrocortisone in Extremely Preterm Infants
Placental Findings and Effect of Alice Héneau, MD, a Fabien Guimiot, PD, PhD, b Damir Mohamed, MSc, c, d Aline Rideau Batista Novais, MD, PhD, a ProphylacticCorinne Alberti, MD, PhD, c, d Olivier Baud, HydrocortisoneMD, PhD, a, e for the PREMILOC Trial study group in Extremely Preterm Infants OBJECTIVES: abstract To investigate the relationship between histologic findings of the placenta and response to early postnatal hydrocortisone treatment used to prevent bronchopulmonary METHODS: dysplasia (BPD) in extremely preterm infants. In an exploratory analysis of the Early Low-Dose Hydrocortisone to Improve Survival Without Bronchopulmonary Dysplasia in Extremely Preterm Infants (PREMILOC) trial, detailed placental analyses were performed on the basis of standardized macroscopic and histologic examinations. Placental histology, categorized into 3 groups, was correlated RESULTS: to neonatal outcomes and response to hydrocortisone treatment. Of 523 randomly assigned patients, 457 placentas were analyzed. In total, 125 out of 457 (27%) placentas were classified as normal, 236 out of 457 (52%) placentas were classified as inflammatory, and 96 out of 457 (21%) placentas were classified as vascular. ’ Placental inflammation was associated with a significant, increased rate of BPD-freeP survival at 36 weeks postmenstrual age, independent of gestational age, treatment group, and sex (adjusted odds ratio: 1.72, 95% confidence interval [CI]: 1.05 to 2.82, = .03). Regarding the response to treatment, the strongest benefit of hydrocortisone Pcompared with placebo was found in infants born after placental vascular disease, with significantly more Ppatients extubated at day 10 (risk difference: 0.32, 95% CI: 0.08 to 0.56, = .004) and similar positive direction on survival without BPD (risk difference: 0.23, 95% CI: 0.00 to 0.46, = .06). -

High Risk L&D
High Risk L&D, pg 1 of 12 Taking care of patients who have non-reasurring pattern • A non-reassuring pattern is: • no variability • less than 2 accelerations • decelerations • In antepartum setting, you are looking at variable and accelerations • Parameters for 28-32 weeks is different than 32 weeks or greater • What about in labor? • looking for late decels (these are bad) • variability is THE most important thing! • moderate variability shows the CNS is intact • absent variability is no bueno...this would be a big issue if it was moderate before and now has become absent. If pt had medication, then this may not be so much of a concern b/c the meds affects the baby. • minimal may be bad (probably is) • marked is also not good • Category 1: has variablity, maybe a random decel (but most likely none), has accelerations • Category 2: starting to get into a little gray area; physician can proceed forward with usual plan of care; moderate or minimal variability; may have recurring decels (of any type); • Category3 : absent or minimal variability with repetitive late decels; baby is not coping • What’s the first thing you would do if pt had repetitive variable decels? • reposition, increase IV, put Oxygen on mom, call doc (You will reposition b/c the variable decels are d/t cord compression). • You would give O2 if she had decreased variability (according to Dr. Ferguson) • Baby can get late decels from mom lying on her back (so position change), or from having low BP (so give IV bolus). Things you need for precipitous birth • IV • Oxygen • BOA kit (Birth on Arrival kit) What kind of risks are involved with precipitous birth? • Tearing at perineum • Hemorrhage d/t lacerations and such • Pneumothorax (not in boook!). -

Twin Transfusion Syndrome
Obstetrica }i Ginecologia LXVI (2018) 129-133 Review article UNDERSTANDING THE PATHOPHYSIOLOGY OF THE TWIN-TO- TWIN TRANSFUSION SYNDROME N. Suciu1,2, A.Oncescu1, Andreea-Cătălina Fetecău1, L. Pop1, Oana Toader1,2 1Departament of Obstetrics and Gynecology, “Alessandrescu-Rusescu” National Institute for Mother and Child Care, Polizu Hospital, Bucharest. 2 Department of Obstetrics and Gynecology, ”Carol Davila” University of Medicine and Pharmacy, Bucharest Abstract Twin-to-twin transfusion syndrome (TTTS) also known as twin oligohydramnios-polyhydramnios sequence (TOPS) is considered to be one of the most frequent complications of monochorionic diamniotic pregnancies. The placenta lies at the core of the TTTS pathophysiology and during the past two decades, numerous studies have been carried out in order to help understand the transfusional mechanisms. The placental anastomoses, which are the primary mediators of transfusional imbalance are incapable of fully explaining the disease and also the negative impact it has on both the renal and cardiovascular systems. The current paper is aimed at providing an insight into the placental and fetal pathophysiology of the syndrome after reviewing the current articles published in the literature. Rezumat Sindromul transfuzor-transfuzat (TTTS), cunoscut si sub denumirea de secventa oligohidramnios- polihidramnios (TOPS) este considerat a fi una dintre cele mai frevvente si severe complicatii ce apar la sarcinile gemelare monocoriale, biamniotice. Placentatia jocă un rol substantial în fiziopatologia sindromului transfuzor- transfuzat si, în ultimii 20 de ani, numaroase studii au fost efectuate pentru a ajuta la întelegerea mecanismelor transfuzionale ce stau la baza acestui tip de sindrom. Anastomozele placentare, depistate la sarcinile gemelare cu TTTS si principalii mediatori răspunzători de dezechilibrul transfuzional sunt insuficienti pentru a putea explica aparitia sindromului precum si impactul negativ al acestuia asupra sistemelor renal si cardiovascular fetale. -

Pregnant Woman with Circumvallate Placenta and Suspected Fetal Hypotrophy Caused by Placental Insufficiency: a Case Report
© Copyright by PMWSZ w Opolu e-ISSN 2544-1620 Medical Science Pulse 2020 (14) 4 Case reports Published online: 31 Dec 2020 DOI: 10.5604/01.3001.0014.6735 PREGNANT WOMAN with circumvALLATE PLACENTA AND suspEctED FETAL hypOtrOphy CAusED BY PLACENTAL INsuFFiciENcy: A CASE REPOrt Jadwiga Surówka1 A,B,D–F 1 SSG of Midwifery Care, Jagiellonian University Medical College, • ORCID: 0000-0003-0170-8820 Kraków, Poland 2 A,B,D–F 2 Institute of Nursing and Midwifery, Faculty of Health Sciences, Dorota Matuszyk Jagiellonian University Medical College, Kraków, Poland • ORCID: 0000-0002-3765-6869 A – study design, B – data collection, C – statistical analysis, D – interpretation of data, E – manuscript preparation, F – literature review, G – sourcing of funding ABSTRACT Background: The circumvallate placenta is a rare pathology of the human placenta that occurs in 1–2% of pregnancies. It is characterized by extrachorial placental development, resulting in a ring formation along the edges of the placenta, which leads to efficiency impairment. As a consequence, it causes an intrauter- ine fetal hypotrophy. The fetal hypotrophic pregnancies are classified as high-risk pregnancies, requiring not only intensive monitoring of fetal development but also maternal and fetal care by the highest reference clinical center. Aim of the study: The aim of this study was to analyze the case of a patient with circumvallate placenta and fetal hypotrophy suspicion. Material and methods: The study was based on the case study method. The data was obtained by analyzing medical documentation collected during hospitalization. The patient was interviewed and observed. All of the selected parameters were measured and scaled. -

Evaluation of Prenatal Adenoviral Vascular Endothelial Growth Factor Gene Therapy in the Growth-Restricted Sheep Fetus and Neonate
Evaluation of Prenatal Adenoviral Vascular Endothelial Growth Factor Gene Therapy in the Growth-Restricted Sheep Fetus and Neonate David John Carr University College London 2013 A thesis submitted for the degree of Doctor of Philosophy 1 Declaration I, David Carr, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 Abstract Background Fetal growth restriction (FGR) is associated with reduced uterine blood flow (UBF). In normal sheep pregnancies, adenovirus (Ad) mediated over-expression of vascular endothelial growth factor (VEGF) in the uterine arteries (UtA) increases UBF. It was hypothesised that enhancing UBF would improve fetal substrate delivery in an ovine paradigm of FGR characterised by reduced UBF from mid-gestation. Methods Singleton pregnancies were established using embryo transfer in adolescent ewes subsequently overnourished to generate FGR (n=81). Ewes were randomised mid-gestation to 11 receive bilateral UtA injections of 5x10 particles Ad.VEGF-A165 or inactive treatment (saline or 5x1011 particles Ad.LacZ, a control vector). Fetal growth/wellbeing were evaluated using serial ultrasound. Late-gestation study: UBF was monitored using indwelling flowprobes until necropsy at 0.9 gestation. Vasorelaxation, neovascularisation in perivascular adventitia and placental mRNA expression of angiogenic factors/receptors were examined. A group of control-fed ewes with normally-developing fetuses was included (n=12). Postnatal study: Pregnancies continued until spontaneous delivery near to term. Lambs were weighed and measured weekly and underwent metabolic challenge at 7 weeks, dual-energy X-ray absorptiometry at 11 weeks, and necropsy at 12 weeks postnatal age. -

Preface Preface from the Editors
Preface Preface from the Editors t is with both excitement and sadness that we present to etry came onto the stage, dramatically changing the newborn you the final issue of the UTMJ for the 2011-2012 aca- screen to include the identification of more than 50 metabol- Idemic year. Serving as your Editors-in-Chief this year has ic disorders.3 However, with the increasing ability to identify been an immense pleasure, and has allowed us the oppor- disorders comes the complex challenge of treating them, and tunity to carry on the many exciting endeavours and initia- the ensuing debate on the value of identifying a disorder if no tives associated with the UTMJ. For our final issue, we decided viable or definitive treatment currently exists.3 to focus on a topic that is widely popular, multifaceted and The topic of fetal treatment is another issue that often sometimes controversial: obstetrics and gynaecology. comes into the news headlines, with astonishing advances in The landscape of obstetrics and gynaecology is an ever- fetal therapy and fetal surgery. Familiar early fetal therapies changing one. For example, something as seemingly simple include simple procedures, such as the first transplacental as contraception has seen a continuous stream of changes and administration of glucorticoids to mature fetal lungs in situ- advancements over the years, which is evident in our Histori- ations of premature delivery in 1972.4 More advanced fetal cal Perspective article published by Foster in 1969. The prac- surgeries began in the 1980s, often credited -

New Perspectives on the Late-Term Mare and Newborn Foal
IN-DEPTH: PERINATOLOGY—END OF PREGNANCY THROUGH BEGINNING OF LIFE New Perspectives on the Late-Term Mare and Newborn Foal Wendy Vaala, VMD, Diplomate ACVIM Author’s address: Equine Technical Services, Intervet Inc., 29160 Intervet Lane, Millsboro, DE 19966; e-mail: [email protected]. © 2007 AAEP. 1. Introduction dotal observations and conclusions can be inferred, A successful perinatal program requires the col- because there is not a large enough number of clin- laborative efforts of those trained in reproduction ical cases with similar problems from which to and neonatology. In ambulatory situations, one draw significant conclusions. Until larger, multi- person must often specialize in both areas; addition- centric collaborative trials validate the usefulness of ally, that person must have the equipment and monitoring specific hormones or the efficacy of var- expertise available to manage obstetrical complica- ious therapies designed to manage and maintain tions and to provide neonatal resuscitation and complicated pregnancies, it is the author’s recom- nursing care. Periparturient complications during mendation that no one therapy or monitoring aid late pregnancy may include severe maternal illness should be relied on exclusively. Any mare receiv- or colic, reproductive tract disease, or fetal anoma- ing therapy to prolong an abnormal pregnancy lies. The most serious threats to uteroplacental should receive frequent assessment. That way, the health and foal survival are perinatal sepsis, hypox- clinician can promptly determine if silent or unde- ia/ischemia, and maturation disorders. The chal- tected fetal demise occurs without ensuing abortion lenge is to improve our ability to recognize mares or if parturition occurs without the customary warn- with jeopardized pregnancies at an earlier stage in ing signs. -

Coverkids Diagnosis Codes for Pregnancy and Complications of Pregnancy
CoverKids Diagnosis Codes for Pregnancy and Complications of Pregnancy This list is for informational purposes only and is not a binding or definitive list of covered conditions. It is not a guarantee of coverage; coverage depends on the available benefits and eligibility at the time services are rendered. It is for use only with the CoverKids program. When filing claims, providers should use the most accurate codes for the condition being treated – it is fraud against the State of Tennessee and BlueCross BlueShield of Tennessee to intentionally use a code for a covered condition when the treatment provided is for a non- covered condition. -
![Twin-To-Twin Transfusion Syndrome [1]](https://docslib.b-cdn.net/cover/7968/twin-to-twin-transfusion-syndrome-1-1587968.webp)
Twin-To-Twin Transfusion Syndrome [1]
Published on The Embryo Project Encyclopedia (https://embryo.asu.edu) Twin-to-Twin Transfusion Syndrome [1] By: DeRuiter, Corinne Keywords: Fetus [2] Congenital disorders [3] Human development [4] Twin-to-Twin Transfusion Syndrome (TTTS) is a rare placental disease that can occur at any time duringp regnancy [5] involving identical twins. TTTS occurs when there is an unequal distribution of placental blood vessels between fetuses, which leads to a disproportionate supply of blood delivered. This unequal allocation of blood leads to developmental problems in both fetuses that can range in severity depending on the type, direction, and number of interconnected blood vessels. TTTS only affects identical twin pregnancies during which the fetuses share ap lacenta [6] during development. The placenta [6] acts as an interface between the mother and twins during pregnancy [5], and is the organ that is responsible for supplying the developing fetuses with blood. Twins afflicted by TTTS have a higher mortality rate than twins without TTTS, especially if the syndrome occurs twenty-six weeks or earlier in pregnancy [5]. In describing TTTS, one of the developing fetuses is considered a donor twin and the other a recipient twin. TTTS occurs when the placenta [6] has fewer blood vessels that connect it to the donor twin than connect it to the recipient twin. The blood that would normally go to the donor twin is then diverted to the recipient twin, causing a reduction [7] in blood volume in the donor twin. This excess of blood in the recipient twin can strain the recipient twin’s heart and may ultimately lead to heart failure. -

SARS-Cov-2 and Placenta: New Insights and Perspectives
viruses Article SARS-CoV-2 and Placenta: New Insights and Perspectives Leonardo Resta 1 , Antonella Vimercati 2 , Gerardo Cazzato 1,* , Giulia Mazzia 1, Ettore Cicinelli 2, Anna Colagrande 1, Margherita Fanelli 3 , Sara Vincenza Scarcella 1, Oronzo Ceci 1 and Roberta Rossi 1 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (L.R.); [email protected] (G.M.); [email protected] (A.C.); [email protected] (S.V.S.); [email protected] (O.C.); [email protected] (R.R.) 2 Department of Biomedical Sciences and Human Oncology, Gynecologic and Obstetrics Clinic, University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (A.V.); [email protected] (E.C.) 3 Medical Statistic, Department of Interdisciplinary Medicine, University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-340-5203641 Abstract: The study of SARS-CoV-2 positive pregnant women is of some importance for gynecolo- gists, obstetricians, neonatologists and women themselves. In recent months, new works have tried to clarify what happens at the fetal–placental level in women positive for the virus, and different pathogenesis mechanisms have been proposed. Here, we present the results of a large series of placentas of Coronavirus disease (COVID) positive women, in a reference center for COVID-positive pregnancies, on which we conducted histological, immunohistochemical and electron microscopy investigations. A case–control study was conducted in order to highlight any histopathological alterations attributable to SARS-CoV-2. -

Macroscopic Examination of Fetal Appendices in Delivery Room: Good Practice at Panzi Hospital
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Walala BD et al. Int J Reprod Contracept Obstet Gynecol. 2020 May;9(5):2215-2221 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20201841 Clinical Problem Solving Macroscopic examination of fetal appendices in delivery room: good practice at Panzi hospital Boengandi Walala D.1*, Nyakio Ngeleza O.1, Mukanire Ntakwinja B.1, Raha Maroyi K.1, Katenga Bosunga G.2, Mukwege Mukengere D.1 1Department of Gynecology and Obstetrics, Panzi Hospital, School of Medicine, Evangelical University in Africa, Bukavu, DR Congo 2Department of Gynecology and Obstetrics, Kisangani University Clinics, School of Medicine, Kisangani University, Kisangani, DR Congo Received: 14 January 2020 Revised: 20 February 2020 Accepted: 28 February 2020 *Correspondence: Dr. Boengandi Walala D., E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT The review of fetal appendices is described in the literature, and its importance is well established. Indeed, pathological findings in the placenta can provide information on the pathogenesis of the fetus, including intrauterine growth retardation, mental retardation or neurodevelopmental disorders. This helps to understand a child's disability, but also maternal complications such as preeclampsia. Despite the relevant information provided by the various studies, fetal appendices are not systematically examined in several maternity hospitals in our country, DR Congo. -

Pregnant Woman with Circumvallate Placenta and Suspected Fetal Hypotrophy Caused by Placental Insufficiency: a Case Report
© Copyright by PMWSZ w Opolu e-ISSN 2544-1620 Medical Science Pulse 2020 (14) 4 Case reports Published online: 31 Dec 2020 DOI: 10.5604/01.3001.0014.6735 PREGNANT WOMAN with circumvALLATE PLACENTA AND suspEctED FETAL hypOtrOphy CAusED BY PLACENTAL INsuFFiciENcy: A CASE REPOrt Jadwiga Surówka1 A,B,D–F 1 SSG of Midwifery Care, Jagiellonian University Medical College, • ORCID: 0000-0003-0170-8820 Kraków, Poland 2 A,B,D–F 2 Institute of Nursing and Midwifery, Faculty of Health Sciences, Dorota Matuszyk Jagiellonian University Medical College, Kraków, Poland • ORCID: 0000-0002-3765-6869 A – study design, B – data collection, C – statistical analysis, D – interpretation of data, E – manuscript preparation, F – literature review, G – sourcing of funding ABSTRACT Background: The circumvallate placenta is a rare pathology of the human placenta that occurs in 1–2% of pregnancies. It is characterized by extrachorial placental development, resulting in a ring formation along the edges of the placenta, which leads to efficiency impairment. As a consequence, it causes an intrauter- ine fetal hypotrophy. The fetal hypotrophic pregnancies are classified as high-risk pregnancies, requiring not only intensive monitoring of fetal development but also maternal and fetal care by the highest reference clinical center. Aim of the study: The aim of this study was to analyze the case of a patient with circumvallate placenta and fetal hypotrophy suspicion. Material and methods: The study was based on the case study method. The data was obtained by analyzing medical documentation collected during hospitalization. The patient was interviewed and observed. All of the selected parameters were measured and scaled.