Step by Step Guide to Reducing from Benzodiazepines
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

XANAX® Alprazolam Tablets, USP
XANAX® alprazolam tablets, USP CIV WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death [see Warnings, Drug Interactions]. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation. DESCRIPTION XANAX Tablets contain alprazolam which is a triazolo analog of the 1,4 benzodiazepine class of central nervous system-active compounds. The chemical name of alprazolam is 8-Chloro-1-methyl-6-phenyl-4H-s-triazolo [4,3-α] [1,4] benzodiazepine. The structural formula is represented to the right: Alprazolam is a white crystalline powder, which is soluble in methanol or ethanol but which has no appreciable solubility in water at physiological pH. Each XANAX Tablet, for oral administration, contains 0.25, 0.5, 1 or 2 mg of alprazolam. XANAX Tablets, 2 mg, are multi-scored and may be divided as shown below: 1 Reference ID: 4029640 Inactive ingredients: Cellulose, corn starch, docusate sodium, lactose, magnesium stearate, silicon dioxide and sodium benzoate. In addition, the 0.5 mg tablet contains FD&C Yellow No. 6 and the 1 mg tablet contains FD&C Blue No. 2. CLINICAL PHARMACOLOGY Pharmacodynamics CNS agents of the 1,4 benzodiazepine class presumably exert their effects by binding at stereo specific receptors at several sites within the central nervous system. Their exact mechanism of action is unknown. Clinically, all benzodiazepines cause a dose-related central nervous system depressant activity varying from mild impairment of task performance to hypnosis. -

Calculating Equivalent Doses of Oral Benzodiazepines
Calculating equivalent doses of oral benzodiazepines Background Benzodiazepines are the most commonly used anxiolytics and hypnotics (1). There are major differences in potency between different benzodiazepines and this difference in potency is important when switching from one benzodiazepine to another (2). Benzodiazepines also differ markedly in the speed in which they are metabolised and eliminated. With repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues) (2). The degree of sedation that they induce also varies, making it difficult to determine exact equivalents (3). Answer Advice on benzodiazepine conversion NB: Before using Table 1, read the notes below and the Limitations statement at the end of this document. Switching benzodiazepines may be advantageous for a variety of reasons, e.g. to a drug with a different half-life pre-discontinuation (4) or in the event of non-availability of a specific benzodiazepine. With relatively short-acting benzodiazepines such as alprazolam and lorazepam, it is not possible to achieve a smooth decline in blood and tissue concentrations during benzodiazepine withdrawal. These drugs are eliminated fairly rapidly with the result that concentrations fluctuate with peaks and troughs between each dose. It is necessary to take the tablets several times a day and many people experience a "mini-withdrawal", sometimes a craving, between each dose. For people withdrawing from these potent, short-acting drugs it has been advised that they switch to an equivalent dose of a benzodiazepine with a long half life such as diazepam (5). Diazepam is available as 2mg tablets which can be halved to give 1mg doses. -

Drugs of Abuse: Benzodiazepines
Drugs of Abuse: Benzodiazepines What are Benzodiazepines? Benzodiazepines are central nervous system depressants that produce sedation, induce sleep, relieve anxiety and muscle spasms, and prevent seizures. What is their origin? Benzodiazepines are only legally available through prescription. Many abusers maintain their drug supply by getting prescriptions from several doctors, forging prescriptions, or buying them illicitly. Alprazolam and diazepam are the two most frequently encountered benzodiazepines on the illicit market. Benzodiazepines are What are common street names? depressants legally available Common street names include Benzos and Downers. through prescription. Abuse is associated with What do they look like? adolescents and young The most common benzodiazepines are the prescription drugs ® ® ® ® ® adults who take the drug Valium , Xanax , Halcion , Ativan , and Klonopin . Tolerance can orally or crush it up and develop, although at variable rates and to different degrees. short it to get high. Shorter-acting benzodiazepines used to manage insomnia include estazolam (ProSom®), flurazepam (Dalmane®), temazepam (Restoril®), Benzodiazepines slow down and triazolam (Halcion®). Midazolam (Versed®), a short-acting the central nervous system. benzodiazepine, is utilized for sedation, anxiety, and amnesia in critical Overdose effects include care settings and prior to anesthesia. It is available in the United States shallow respiration, clammy as an injectable preparation and as a syrup (primarily for pediatric skin, dilated pupils, weak patients). and rapid pulse, coma, and possible death. Benzodiazepines with a longer duration of action are utilized to treat insomnia in patients with daytime anxiety. These benzodiazepines include alprazolam (Xanax®), chlordiazepoxide (Librium®), clorazepate (Tranxene®), diazepam (Valium®), halazepam (Paxipam®), lorzepam (Ativan®), oxazepam (Serax®), prazepam (Centrax®), and quazepam (Doral®). -

Alprazolam: Pediatric Medication
PATIENT & CAREGIVER EDUCATION Alprazolam This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US ALPRAZolam Intensol; ALPRAZolam XR; Xanax; Xanax XR Brand Names: Canada ALPRAZolam TS; ALPRAZolam-1; APO-Alpraz; APO-Alpraz TS; JAMP-Alprazolam [DSC]; MYLAN-ALPRAZolam [DSC]; NAT-ALPRAZolam [DSC]; RIVA- ALPRAZolam [DSC]; TEVA-Alprazolam; Xanax; Xanax TS Warning This drug is a benzodiazepine. The use of a benzodiazepine drug along with opioid drugs has led to very bad side effects. Side effects that have happened include slowed or trouble breathing and death. Opioid drugs include drugs like codeine, oxycodone, and morphine. Opioid drugs are used to treat pain and some are used to treat cough. Talk with the doctor. If your child is taking this drug with an opioid drug, get medical help right away if your child feels very sleepy or dizzy; if your child has slow, shallow, or trouble breathing; or if your child passes out. Get medical help right away if your child does not respond, does not answer or react like normal, or will not wake up. Benzodiazepines can put your child at risk for addiction, abuse, and misuse. Misuse or abuse of this drug can lead to overdose or death, especially when used along with certain other drugs, alcohol, or street drugs. Addiction can happen even if your child takes this drug as told by the doctor. Get medical Alprazolam 1/9 help right away if your child has changes in mood or behavior, suicidal thoughts or actions, seizures, or trouble breathing. -

Alprazolam (Xanax): Important Patient Information
What is most important to remember? If you have questions: Strong Internal Medicine • Alprazolam (Xanax®) can be habit-forming and should only be Ask your doctor, nurse or pharmacist for used by the person it was more information about alprazolam prescribed for (Xanax®) • Use this medicine as directed by your doctor • Many times this medicine is ordered to be taken on an as- needed basis. Do not take more often than directed by your doctor • Do not start any new medicines, over-the-counter drugs or herbal remedies without talking to your Strong Internal Medicine doctor 601 Elmwood Avenue th • Tell all doctors, dentists and Ambulatory Care Facility, 5 Floor Rochester, NY 14642 pharmacists that you are using Phone: (585) 275 -7424 alprazolam (Xanax®) Alprazolam Visit our website at: (Xanax®): • Contact your prescriber if your www.urmc.rochester.edu/medicine/ - genera medicine/patientcare/ Important Patient Information symptoms or health problems do l- not get better or are becoming worse What does alprazolam (Xanax®) do? Who should know I am taking alprazolam (Xanax®)? What are some things that I need to be aware of when • It is used to treat symptoms of anxiety • Keep a list of all your medicines (prescription, natural taking alprazolam (Xanax®)? • It is used to treat panic attacks products, supplements, vitamins, over-the-counter) and • Tell your doctor or pharmacist if you are allergic to give it to your healthcare provider (doctor, nurse, nurse alprazolam (Xanax®), or if you are allergic to any other How should alprazolam (Xanax®) be used? practitioner, pharmacist, or physician assistant) medicines, foods, or substances • Use this medicine as directed by your doctor Are there any interactions with other drugs that I need • Before using this medicine, tell your doctor if you have • Many times this medicine is ordered to be taken on an to worry about? glaucoma, liver disease, or lung disease as-needed basis • There are many drug interactions that may increase • This medicine is a controlled substance and may be • Take with or without food. -

Formulary Benzodiazepine Anti-Anxiety Agents
Alprazolam Shortage Recently, alprazolam has been in limited supply at both retail pharmacies and mail service facilities. Alprazolam is commercially manufactured as 0.25mg, 0.5mg, 1mg, and 2mg strength tablets. Retail pharmacies and mail order facilities may have alprazolam in stock but not necessarily all strengths. In response to the shortage of alprazolam, Xanax® (the branded product) has been temporarily added to the formulary. Xanax® XR, a recently approved sustained-release formulation of alprazolam, is not on the Highmark formulary. Although alprazolam quantities are available in limited supply, there are many other benzodiazepines available to treat anxiety. The following generic products in the table below are included on the Highmark formulary. Please consider these alternatives for patients who have difficulty obtaining Xanax or its generic. Formulary Benzodiazepine Anti-anxiety Agents Brandc Name Generic Name Approximate Dosage Range3 Equivalent (mg/day) Dosea, 1 b, 2 Short - Intermediate-acting benzodiazepines Xanax® alprazolam 0.5 mg 0.75 mg – 4 mg Ativan® lorazepam 1 mg 2 mg- 4 mg Serax® oxazepam 15 mg 30 mg – 120 mg b, 2Long-acting benzodiazepines Valium® diazepam 5 mg 4 mg – 40 mg Librium® chlordiazepoxide 10 mg 15 mg – 100 mg Tranxene® clorazepate 7.5 mg 15 mg – 60 mg a Elderly patients are treated with approximately one-half of dose listed b Based on effective half-life of parent drug and active metabolites c Brand products are non-formulary References 1. DiPiro, JT., et al. Pharmacotherapy: A Pathophysiologic Approach. 4th Edition, 1999; 1187 2. Shader RI, Greenblatt DJ. Use of Benzodiazepines in Anxiety Disorders. N Engl J Med 1993; 328: 1398-1405. -

Title Continuation and Discontinuation of Benzodiazepine Prescriptions: A
Continuation and discontinuation of benzodiazepine Title prescriptions: A cohort study based on a large claims database in Japan( Dissertation_全文 ) Author(s) Takeshima, Nozomi Citation 京都大学 Issue Date 2016-05-23 URL https://doi.org/10.14989/doctor.k19890 Right Type Thesis or Dissertation Textversion ETD Kyoto University Psychiatry Research ∎ (∎∎∎∎) ∎∎∎–∎∎∎ Contents lists available at ScienceDirect Psychiatry Research journal homepage: www.elsevier.com/locate/psychres Continuation and discontinuation of benzodiazepine prescriptions: A cohort study based on A large claims database in Japan Nozomi Takeshima, Yusuke Ogawa, Yu Hayasaka, Toshi A Furukawa n Department of Health Promotion and Human Behavior, Kyoto University Graduate School of Medicine/School of Public Health, Yoshida Konoe-cho, Sakyo-ku, Kyoto 606-8501, Japan article info abstract Article history: Although benzodiazepines (BZDs) are often prescribed to treat a wide range of psychiatric and neuro- Received 29 March 2015 logical conditions, they are also associated with various harms and risks including dependence. However Received in revised form the frequency of its continued use in the real world has not been well studied, especially at longer follow- 15 October 2015 ups. The aim of this study was to clarify the frequency of long-term BZD use among new BZD users over Accepted 15 January 2016 longer follow-ups and to identify its predictors. We conducted a cohort study to examine how frequently new BZD users became chronic users, based on a large claims database in Japan from January 2005 to Keywords: June 2014. We used Cox proportional hazards models to identify potential predictors. A total 84,412 Benzodiazepine patients with new BZD prescriptions were included in our cohort. -
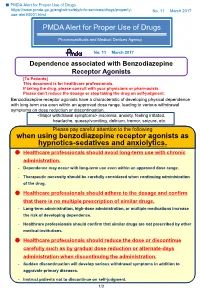
PMDA Alert for Proper Use of Drugs When Using Benzodiazepine
■ PMDA Alert for Proper Use of Drugs https://www.pmda.go.jp/english/safety/info-services/drugs/properly- No. 11 March 2017 use-alert/0001.html PMDA Alert for Proper Use of Drugs Pharmaceuticals and Medical Devices Agency No. 11 March 2017 Dependence associated with Benzodiazepine Receptor Agonists [To Patients] This document is for healthcare professionals. If taking the drug, please consult with your physicians or pharmacists. Please don’t reduce the dosage or stop taking the drug on self-judgment. Benzodiazepine receptor agonists have a characteristic of developing physical dependence with long-term use even within an approved dose range, leading to various withdrawal symptoms on dose reduction or discontinuation. <Major withdrawal symptoms> insomnia, anxiety, feeling irritated, headache, queasy/vomiting, delirium, tremor, seizure, etc. Please pay careful attention to the following when using benzodiazepine receptor agonists as hypnotics-sedatives and anxiolytics. Healthcare professionals should avoid long-term use with chronic administration. - Dependence may occur with long-term use even within an approved dose range. - Therapeutic necessity should be carefully considered when continuing administration of the drug. Healthcare professionals should adhere to the dosage and confirm that there is no multiple prescription of similar drugs. - Long-term administration, high-dose administration, or multiple medications increase the risk of developing dependence. - Healthcare professionals should confirm that similar drugs are not prescribed by other medical institutions. Healthcare professionals should reduce the dose or discontinue carefully such as by gradual dose reduction or alternate-days administration when discontinuing the administration. - Sudden discontinuation will develop serious withdrawal symptoms in addition to aggravate primary diseases. -

Focus on Benzodiazepines
Graylands Hospital Drug Bulletin Focus on Benzodiazepines North Metropolitan Health Service – Mental Health March 2015 Vol 22 No.1 ISSN 1323–1251 The Non -BZD hypnotics such as zolpidem and Introduction zopiclone (Z-drugs) are more selective for the alpha-1 subclass which seems to drive sleepiness but not anti-anxiety. Benzodiazepines (BZDs) are one of the most commonly prescribed medications for the treatment Table 1: BZDs and relative half-lives9,10 of insomnia and anxiety. 1 They are also frequently used to treat psychiatric emergencies, epilepsy, severe muscle spasm, acute alcohol withdrawal, Drug name Half -life (hours) anaesthesia and intensive care. Short -acting Triazolam 2 However, the use of BZDs is often controversial as Alprazolam 6-12 they are widely acknowledged to be addictive and Oxazepam 4-15 withdrawal symptoms can occur after 4-6 weeks of Temazepam 8-22 continuous use. This had led to the recommendation Medium -acting that they should not be used as hypnotics or Bromazepam 10 -20 anxiolytics for longer than 4 weeks. 2 In older age, Lorazepam 10 -20 BZDs also have serious adverse effects, including increased risk of falls, road traffic accidents and Long -acting 3,4 Clobazam 12 -60 cognitive impairment. Clonazepam 18 -50 More recently the risks of long term BZD use have Diazepam 20 -100 received greater focus with new evidence Flunitrazepam 18 -26 demonstrating a link between BZD use and the Nitrazepam 15 -38 5 development of Alzheimer’s disease and also 6 increased risk of mortality. Benzodiazepine use in Psychiatry Given the wide spread usage of these medications and the associated risk, this bulletin reviews BZDs Sleep disorders with particular emphasis upon adverse effects, dependence and abuse potential. -

NHS Fife Guidelines for Benzodiazepine Prescribing in Benzodiazepine Dependence
NHS Fife Guidelines for Benzodiazepine Prescribing in Benzodiazepine Dependence Dr. A. Baldacchino, Liz. Hutchings, Addiction Services Issued: April 2013 Review Date: April 2016 1 Approved by NHS Fife ADTC on behalf of NHS Fife Date June 2013 Contents Flowchart for Benzodiazepine Withdrawal ……………………………………………………………3 Establishing type of dependence. ........................................................................................... 4 Assessment of Benzodiazepine Dependence .............................................................................. 5 Management of dependence in therapeutic dose users ........................................................... 6 Management of dependence in prescribed high dose users. ................................................... 7 Management of dependence in illicit and recreational users. .................................................. 8 Psychological support. ................................................................................................................. 9 Pharmacological support............................................................................................................ 10 Appendices Appendix 1 Example Patient Letter (regular user) ................................................. 11 Appendix 2 Information leaflets and advice from the internet ................................ 13 Appendix 3 DRUG DIARY ..................................................................................... 14 Appendix 4 Benzodiazepine conversion table ...................................................... -

Borders Alcohol & Drugs Partnership (ADP)
Borders Alcohol & Drugs Partnership (ADP) Drug Briefing: Alprazolam (Xanax) April 2018 Alprazolam is a benzodiazepine and is a class C controlled drug. It is not prescribed under NHS but its availability is increased through illegal supply via online sources. Appearance: Alprazolam is most commonly seen in 1mg tablet form and 2mg bars more commonly known as Xanax but is also available in powder form which can be mixed with other substances. Strength: Alprazolam is 20 times the potency of Diazepam and approximately twice as potent as Etizolam. Xanax tablets are active from 0.25mg (meaning 8 doses in a 2mg bar) so people consuming full tablets are taking a very large dose. If larger amounts of Xanax is consumed this can increase the risk of overdose especially if mixed with alcohol and other drugs. Cost: Across the UK street prices are estimated at £1.50 for 1mg and £3-5 for a 2mg Xanax bar, but this can vary and the more tablets purchased the cheaper the price. Across the UK the drug is being used either as a comedown aid from stimulants or psychedelics or to enhance dissociative effects of some drugs. Effects: Reported effects of pleasure, relaxation and bodily comfort, disinhibition and reduction in anxiety. Other effects may include: • drowsiness, feeling tired; • slurred speech, lack of balance or coordination; • memory problems; or • feeling anxious early in the morning. After effects include increase in hostility and aggression. This is not a complete list of side effects and others may occur. Harm reduction advice for individuals: • Wherever possible, do not use on your own • Alprazolam is 20 times the potency of diazepam. -

XANAX (Alprazolam) Tablets, for Oral Use, CIV Ritonavir
HIGHLIGHTS OF PRESCRIBING INFORMATION When tapering, decrease dosage by no more than 0.5 mg every 3 days. These highlights do not include all the information needed to use XANAX Some patients may require an even slower dosage reduction. (2.3, 5.2) safely and effectively. See full prescribing information for XANAX. See the Full Prescribing Information for the recommended dosage in geriatric patients, patients with hepatic impairment, and with use with XANAX (alprazolam) tablets, for oral use, CIV ritonavir. (2.4, 2.5, 2.6) Initial U.S. Approval: 1981 --------------------- DOSAGE FORMS AND STRENGTHS --------------------- Tablets: 0.25 mg, 0.5 mg, 1 mg, and 2 mg (3) WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and ------------------------------ CONTRAINDICATIONS ------------------------------ DEPENDENCE AND WITHDRAWAL REACTIONS Known hypersensitivity to alprazolam or other benzodiazepines. (4) See full prescribing information for complete boxed warning. Concomitant use with strong cytochrome P450 3A (CYP3A) inhibitors, except ritonavir. (4, 5.5, 7.1) Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. ----------------------- WARNINGS AND PRECAUTIONS ----------------------- Reserve concomitant prescribing for use in patients for whom Effects on Driving and Operating Machinery: Patients receiving XANAX alternative treatment options are inadequate. Limit dosages and should be cautioned against operating machinery or driving a motor durations to the minimum required. Follow patients for signs and vehicle, as well as avoiding concomitant use of alcohol and other central symptoms of respiratory depression and sedation. (5.1, 7.1) nervous system (CNS) depressant drugs. (5.4) The use of benzodiazepines, including XANAX, exposes users to Neonatal Sedation and Withdrawal Syndrome (NOWS): Use of XANAX risks of abuse, misuse, and addiction, which can lead to overdose or during pregnancy can result in neonatal sedation and neonatal withdrawal death.