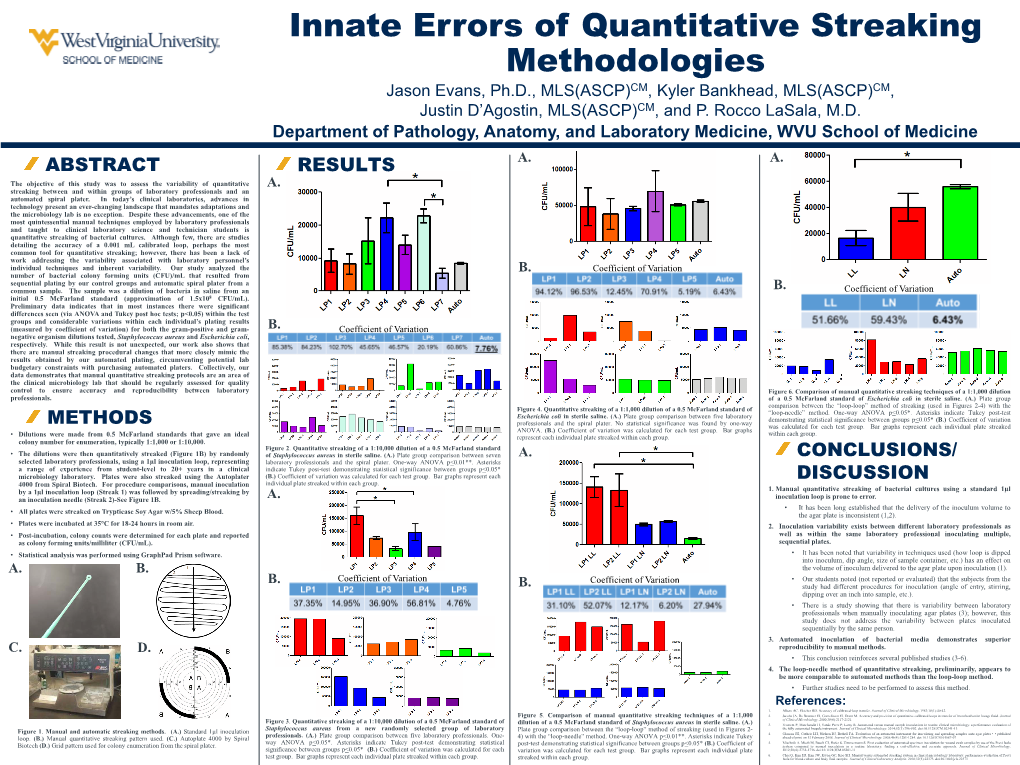
Innate Errors of Quantitative Streaking Methodologies Jason Evans, Ph.D., MLS(ASCP)CM, Kyler Bankhead, MLS(ASCP)CM, Justin D’Agostin, MLS(ASCP)CM, and P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Genus Staphylococcus 19 171
43038_CH19_0171.qxd 1/3/07 3:53 PM Page 171 THE GENUS STAPHYLOCOCCUS 19 171 The Genus 19 Staphylococcus embers of the genus Staphylococcus are gram-positive spherical organisms about 1 micrometer in diameter. They M occur singly, in pairs, and in irregular clusters, and form yel- low, orange, or white colonies on agar media. They are salt tolerant and grow on ordinary bacteriological media as well as on the selective media used in this exercise. Up to three species of Staphylococcus are studied in this exercise. Cer- tain strains of Staphylococcus aureus are the cause of food poisoning and toxic shock syndrome. They also are the cause of boils and carbuncles. A second species, S. epidermidis, usually is a saprobe of the skin that is rarely involved in human infection. The third species, S. saprophyticus, is an opportunistic species that may cause urinary tract infections in women of childbearing years. In this exercise, staphylococcal species will be isolated from the body’s environment and their properties examined. A. Isolation of Staphylococci Species of Staphylococcus are tolerant to salt and, therefore, they can be PURPOSE: to isolate and selected out from a mixture of bacteria in a high-salt medium. In addition, identify staphylococcal species from the nasal cavity S. aureus ferments mannitol, an alcoholic derivative of the hexose mannose, and other environments. while S. epidermidis and S. saprophyticus do not. Therefore, if the differential medium contains mannitol, the two species may be differentiated from one another. In this section, we will use mannitol salt agar, a medium that is both selective and differential. -

Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation
City University of New York (CUNY) CUNY Academic Works Open Educational Resources Queensborough Community College 2016 Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation Joan Petersen CUNY Queensborough Community College Susan McLaughlin CUNY Queensborough Community College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/qb_oers/16 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation By Dr. Susan McLaughlin & Dr. Joan Petersen Queensborough Community College Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation Table of Contents Preface………………………………………………………………………………………i Acknowledgments…………………………………………………………………………..ii Microbiology Lab Safety Instructions…………………………………………………...... iii Lab 1. Introduction to Microscopy and Diversity of Cell Types……………………......... 1 Lab 2. Introduction to Aseptic Techniques and Growth Media………………………...... 19 Lab 3. Preparation of Bacterial Smears and Introduction to Staining…………………...... 37 Lab 4. Acid fast and Endospore Staining……………………………………………......... 49 Lab 5. Metabolic Activities of Bacteria…………………………………………….…....... 59 Lab 6. Dichotomous Keys……………………………………………………………......... 77 Lab 7. The Effect of Physical Factors on Microbial Growth……………………………... 85 Lab 8. Chemical Control of Microbial Growth—Disinfectants and Antibiotics…………. 99 Lab 9. The Microbiology of Milk and Food………………………………………………. 111 Lab 10. The Eukaryotes………………………………………………………………........ 123 Lab 11. Clinical Microbiology I; Anaerobic pathogens; Vectors of Infectious Disease….. 141 Lab 12. Clinical Microbiology II—Immunology and the Biolog System………………… 153 Lab 13. Putting it all Together: Case Studies in Microbiology…………………………… 163 Appendix I. -

Thesis Evaluations That Increase Value for Pork
THESIS EVALUATIONS THAT INCREASE VALUE FOR PORK EXPORT PRODUCTS Submitted by Dan Sewald Department of Animal Sciences In partial fulfillment of the requirements For the degree of Master of Science Colorado State University Fort Collins, Colorado Fall 2017 Master’s Committee: Advisor: Dale R. Woerner Keith E. Belk Gary Mason Copyright by Dan Robert Sewald 2017 All Rights Reserved ABSTRACT EVALUATIONS THAT INCREASE VALUE FOR PORK EXPORT PRODUCTS Experiment 1: An evaluation of the suitability of porcine lung tissue for human consumption This study was conducted to provide evidence of the safety of pork lungs for human consumption via an assessment of prevalence of potentially pathogenic bacteria and infectious agents. Specifically, the goal was to collect evidence that could be used to petition the current regulation disallowing use of pork lungs for human food. Pork lungs have been labeled by the U.S. Meat Export Federation as a widely consumed product across Asia as well as South and Central America. It was believed that there is profit potential in saving pork lungs and exporting them to specified countries. Pork lungs must first be deemed safe and edible before they can be sold on the export market. Lungs (N = 288) were collected from a total of six federally inspected young market barrow/gilt or sow processing facilities. In an attempt to obtain a representative sample of production at each facility on a given day, lungs were randomly selected throughout the entire production day. All collected lungs were removed and processed using aseptic techniques to prevent any exogenous contamination. Lung samples were tested for the presence of pathogens and other physical contamination. -

Experiment 4 Aseptic Cult-Ure Technique
I EXPERIMENT 4 ASEPTIC CULT-URE I TECHNIQUE I I Structure I 4.1 Introduction I Objectives I 4.2 Experiment I 4.1.1 Principle I 4.1.2 Observations I 4.3 Precautions I 4.1 INTRODUCTION I I In previous experiments you learned that microorganisms thrive pretty much I everywhere. It is far too easy to contaminate your lab cultures and experiments with stray microorganisms from the air, the countertop, or your tools. It is also possible to I expose your surroundings or ycurself'to a possible pathogen. In this lab exercise, you wrll I learn to transfer microbiological cultures from one medium to a second sterile medium without contamination of the culture, sterile medium, or the surroundings. I I Objectives I After studying and performing this experiment, you should be able to: I • know how to handle microorganisms, tubed media, plated media, and inoculating I tools such as loops, needles, or swabs etc.; I • leai n how to transfer bacteria from test tubes or broth and agar; and I • learn how to transfer bacteria from Petri plates. I 4.2 EXPERIMENT I I 4.2.1 Principle I Aseptic technique is a method that prevents the introduction of unwanted organisms into I an environment. In order to protect sterile broth, media, plates, slants etc. from I contamination we must practice aseptic i.e. sterile techniques to protect our material from contamination. By using aseptic technique only sterile surface touches other sterile I surface and exposure to the non sterile environment is minimized. I Though, observingaseptic technique is the most important instruction for any micrcbiology I experiment, some common circumstances will be discussed in this practical to make you aware of aseptic techniques. -

LAB 2: Staining and Streaking Protocols for Simple Stain, Gram Stain, Streak Plate Technique and Culture Maintenance
LAB 2: Staining and Streaking Protocols for Simple stain, Gram Stain, Streak Plate Technique and Culture Maintenance Lab 2a: INTRODUCTION To Staining Live specimens are difficult to see with the bright field microscope. The contrast between a cell, which is primarily water, and the background, which is water, is poor. Staining is used to increase contrast and can be employed to provide information about the chemistry of a specimen. Stains, or dyes, are salts in which one of the ions is colored. In a basic stain, the color is in the positively charged ion. In an acidic stain the color is in the negatively charged ion. Bacterial surfaces have a slight negative charge. Thus, there is an affinity between a positively charged color ion and the negatively charged bacterial cell. In the Direct or Positive Staining Procedure a cell takes up a positively charged dye and becomes stained. Methylene blue, crystal violet, and safranin, are all basic dyes. In the Indirect or Negative Staining Procedure, a cell is immersed in a negatively charged dye. As the cell will repel the dye, the cell appears clear in a background of color. Nigrosine is an example of an acidic stain. Staining procedures that use one dye to increase contrast between specimen and background are simple staining procedures. Complex staining procedures employ a series of stains and chemical reagents to increase contrast and reveal information about the specimen. Any staining procedure that allows differentiation of one type of bacterium from another is a differential staining procedure. For all staining procedures, it is first required that cells be fixed to the slide. -

Medical Bacteriology
LECTURE NOTES Degree and Diploma Programs For Environmental Health Students Medical Bacteriology Abilo Tadesse, Meseret Alem University of Gondar In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education September 2006 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2006 by Abilo Tadesse, Meseret Alem All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. PREFACE Text book on Medical Bacteriology for Medical Laboratory Technology students are not available as need, so this lecture note will alleviate the acute shortage of text books and reference materials on medical bacteriology. -

Fifth Semester: Paper V: Environmental Microbiology Paper VI: Agricultural Microbiology and Biotechnology Practical V Practical VI
KUVEMPU UNIVERSITY Revised Syllabus Semester scheme syllabus for B.Sc. Degree course of Microbiology (Effective from 2018-19 onwards) SCHEME OF THE COURSE (Three year course with two semesters in each year) First Semester Paper I: General Microbiology Practical I Second Semester Paper II: Microbiological techniques and instrumentation Part I Practical II Third Semester Paper III: Microbiological techniques and instrumentation Part II Practical III Fourth Semester Paper IV: Microbial physiology and Genetics Practical IV Fifth Semester: Paper V: Environmental Microbiology Paper VI: Agricultural Microbiology and Biotechnology Practical V Practical VI Sixth Semester: Paper VII: Food, Dairy and Industrial Microbiology Paper VIII: Immunology and Medical Microbiology Practical VII: Project/Dissertation Teaching Hours: a. 1st to 4th Semester Theory: 04 hrs/paper/week Practicals: 03 hrs/paper/week b. 5th & 6th Semester Theory: 03 hrs/paper/week Practicals: 03 hrs/paper/week Dissertation/Project work: 03 hrs/week B.Sc. syllabus file Doc. 1 SCHEME OF EXAMINATION First Semester Duration Marks Internal assessment Theory Paper I: 03 hrs. 50 10 (Two tests of 05 marks) Practical I 03 hrs 40 (Practical proper 30; Record 05; Viva 05) Total 100 Second Semester Theory Paper II: 03 hrs. 50 10 (Two tests of 05 marks) Practical II 03 hrs 40 (Practical proper 30; Record 05; Viva 05) Total 100 Third Semester Theory Paper III: 03 hrs. 50 10 (Two tests of 05 marks) Practical III 03 hrs 40 (Practical proper 30; Record 05; Viva 05) Total 100 Fourth Semester Theory Paper IV: 03 hrs. 50 10 (Two tests of 05 marks) Practical IV 03 hrs 40 (Practical proper 30; Record 05; Viva 05) Total 100 Fifth Semester: Theory Paper V: 03 hrs. -

18Btc103j-Microbiology Laboratory Manual
18BTC103J-MICROBIOLOGY LABORATORY MANUAL B.TECH. BIOTECHNOLOGY THIRD SEMESTER DEPARTMENT OF BIOTECHNOLOGY SCHOOL OF BIOENGINEERING SRM INSTITUTE OF SCIENCE AND TECHNOLOGY KATTANKULATHUR-603 203 1 List of Experiments S.No. Experiments 1 Aseptic techniques and Media preparation (Both liquid and solid) 2 Purification techniques of microorganisms (Streak plate) and preservation methods of bacterial cultures 3 Staining Techniques (Simple, Gram staining, and spore staining) 4 Motility test by Hanging drop method 5 Biochemical Characterization of Bacteria– IMViC test 6 Enzyme based biochemical characterizations-Catalase test 7 Enzyme based biochemical characterizations-oxidase test 8 Enzyme based biochemical characterizations-Urease test 9 Triple sugar Iron agar test-H2S production 10 Casein and Starch Hydrolysis 11 Antibiotic sensitivity test-Kirby-Bauer assay 12 Identification of Bacterial morphology by phase contrast Microscopy/Live and dead bacterial cells by Fluorescence Microscopy 13 Identification of bacteria using 16s-rRNA sequencing (Demonstration) 2 Experiment No.1: Aseptic techniques and Media preparation Aim: To acquire the knowledge on aseptic techniques and develop the skill of media preparation for culturing the microbes Principle: Aseptic techniques are a fundamental and important laboratory skill in the field of microbiology. Microbiologists use aseptic techniques for a variety of procedures such as transferring cultures, inoculating media, isolation of pure cultures, and for performing microbiological tests. Proper aseptic technique prevents contamination of cultures from foreign microbes inherent in the environment. For example, airborne microorganisms (including fungal spores), microbes picked up from the researcher’s body, the lab bench-top or other surfaces, microbes found in dust, as well as microbes found on unsterilized glassware and equipment, etc. -

Short Operational Manual for Clinical Microbiology Lab
Short operational manual for clinical microbiology lab SPECIMEN Specimen isolated from non-sterile sites: Sputum, Stool, Urine, Genital tract secretion etc. Specimen isolated from normally sterile sites: Blood, Cerebrospinal fluid (CSF), Pleural fluid, Abdominal fluid, Joint fluid etc. CULTURE MEDIA AND REAGENT Culture media: Columbia blood agar plate Chocolate agar plate(non-selective) Chocolate agar plate(selective) EMB agar plate MacConkey agar plate SS agar plate HE agar plate TCBS agar plate MH agar plate Gonococcal (GC) agar plate Sabouraud’s Dextrose Agar Plate etc. Reagent Gram stain Ziehl-Neelsen Stain India ink (ink stain) 3% H2O2 (Catalase reagent) Oxidase test strip Sterile mineral oil Cedar oil Dimethylbenzene etc. Sterile saline (0.9% NaCl) INSTRUMENT AND CONSUMABLES Instrument and consumables: Bio-safety cabinet: for routine operation such as inoculation etc. CO2 incubator: incubation of streptococcus, fastidious bacteria etc. Air incubator: incubation of regular bacteria such as staphylococcus, enterobacteriaceae etc. Microscope: bacteria morphological examination. Centrifuge: pretreatment of some specimen such as CSF etc. Medicine refrigerator: reagent preservation. Refrigerator(-70℃): bacteria strain preservation. Inoculation needle: puncture inoculation. Inoculation loop: inoculation Quantitative inoculation loop: quantitative inculation. Glass slide: basic operation such as Gram staining, catalase test etc. SS-spreader: spread the plate (or use sterile cotton swab instead) Electronic sterilizer/alcohol lamp: sterilize the inoculation loop etc. Pipettes and pipette tips Pressure steam sterilizer (autoclave) etc SPECIMEN PLANTING PROCEDURES Streaking for isolation: Before identification of bacteria or fungi may be achieved, pure colony must be isolated. That is only one type of colony containing one type of bacteria must be transplanted to the identification system in use. -

Characterization of the Lactobacillus Isolated from Different Curd Samples
African Journal of Biotechnology Vol. 11(79), pp. 14448-14452, 2 October, 2012 Available online at http://www.academicjournals.org/AJB DOI: 10.5897/AJB11.310 ISSN 1684–5315 © 2012 Academic Journals Full Length Research Paper Characterization of the Lactobacillus isolated from different curd samples Renuka Goyal, Harish Dhingra*, Pratima Bajpai and Navneet Joshi Department of Biotechnology and Microbiology, Mody Institute of Technology and Science, Faculty of Arts, Science and Commerce, Lakshmangarh—332311, Distt.-Sikar, Rajasthan, India. Accepted 16 February, 2012 Lactic acid bacteria are commonly found in the fermented dairy products. Lactobacillus is a genus of lactic acid bacteria and described as heterogeneous group of regular, non-spore forming, gram- positive, rod shaped, non-motile bacteria and absence of catalase enzyme. The aim of this study was to isolate Lactobacillus from different curd samples. A total of 14 curd samples were collected from the local areas of Gurgaon (Haryana) and Lakshmangarh (Rajasthan). From these, 28 isolates were obtained by growing on de Man, Rogosa and Sharpe (MRS) agar medium and characterised by their phenotypic characteristics. The Lactobacillus isolates also possess homofermentative and heterofermentative characteristics. Key words: Lactobacillus, curd, microorganism INTRODUCTION Microorganisms are important in dairy products. One of carbohydrates to organic acids (lactic acid and acetic the most important groups of acid producing bacteria in acids) in the food during their development. the food industry is the lactic acid bacteria, which are Among all lactic acid bacteria, the genus Lactobacillus used in making starter culture for dairy products. has some beneficial characteristics which make it useful Genus Lactobacillus contains over 110 species, which for the industrial applications. -

Development of a Standardized Protocol for Optochin Susceptibility Testing Using Total Lab Automation
Hindawi BioMed Research International Volume 2017, Article ID 4174168, 7 pages https://doi.org/10.1155/2017/4174168 Research Article Identification of Streptococcus pneumoniae: Development of a Standardized Protocol for Optochin Susceptibility Testing Using Total Lab Automation Irene Burckhardt,1 Jessica Panitz,1 Florian Burckhardt,2 and Stefan Zimmermann1 1 Department for Infectious Diseases, Microbiology and Hygiene, University Hospital of Heidelberg, Heidelberg, Germany 2EPIET Alumni Network (EAN), Heidelberg, Germany Correspondence should be addressed to Irene Burckhardt; [email protected] Received 5 January 2017; Accepted 22 February 2017; Published 19 March 2017 Academic Editor: Gyorgy¨ Schneider Copyright © 2017 Irene Burckhardt et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose. Optochin susceptibility is one parameter used in the laboratory to identify Streptococcus pneumoniae.However,asingle standardized procedure does not exist. Optochin is included neither in the current EUCAST breakpoint tables nor in the CLSI performance standards for antimicrobial susceptibility testing. We wanted to establish an evidence-based protocol for optochin testing for our Total Lab Automation. Methods. We tested seven different agars and four different reading time points (7 h, 12h, 18 h, and 24 h). To accommodate for serotype diversity, all tests were done with 99 different strains covering 34 different serotypes of S. pneumoniae. We calculated a multivariable linear regression using data from 5544 inhibition zones. Results. Reading was possible for all strains at 12 h. Agar type and manufacturer influenced the size of the inhibition zones by up to 2 mm and they varied considerably depending on serotype (up to 3 mm for serotype 3). -

Exercise 4 ASEPTIC TECHNIQUE & STREAK PLATE PREPARATION
Exercise 4 ASEPTIC TECHNIQUE & STREAK PLATE PREPARATION Introduction In order to make laboratory studies with pure microbial cultures, microbiologists must start with sterile culture media and must be able to prevent contamination of this media. At the same time, they must be able to inoculate media with the desired pure cultures without introducing any other organisms. The procedure utilized to accomplish this is referred to as aseptic technique and is essential to any microbiology laboratory. Remember that all culture media must be sterile prior to inoculation. Media samples that appear to be contaminated with unknown cultures (are already supporting growth) must be discarded and not used for laboratory exercises. Transfer Instruments In order to inoculate a tube or plate with a desired microbial culture, students will use some type of transfer instrument, usually a wire loop or a pipette. If a wire loop or needle is being used, it must be sterilized (heated to redness by flaming) before and after making the microbial transfer. This heating destroys any living forms on the surface of the needle or loop, thus preventing unwanted contamination. To sterilize the loop or needle, hold it in the hottest part of the flame at an angle that will distribute heat to the entire length of the wire. After the loop or needle is sterilized in this manner, it must be allowed to cool briefly before being used to pick up the desired culture. Remember that contact with hot metal will kill bacteria. When using a wire loop to transfer bacteria from cultures grown on solid media it is recommended that students avoid filling the loop.