Covidview Week 1, Ending January 9, 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Early Dance Division Calendar 17-18
Early Dance Division 2017-2018 Session 1 September 9 – November 3 Monday Classes Tuesday Classes September 11 Class September 12 Class September 18 Class September 19 Class September 25 Class September 26 Class October 2 Class October 3 Class October 9 Class October 10 Class October 16 Class October 17 Class October 23 Class October 24 Class October 30 Last Class October 31 Last Class Wednesday Classes Thursday Classes September 13 Class September 14 Class September 20 Class September 21* Class September 27 Class September 28 Class October 4 Class October 5 Class October 11 Class October 12 Class October 18 Class October 19 Class October 25 Class October 26 Class November 1 Last Class November 2 Last Class Saturday Classes Sunday Classes September 9 Class September 10 Class September 16 Class September 17 Class September 23 Class September 24 Class September 30* Class October 1 Class October 7 Class October 8 Class October 14 Class October 15 Class October 21 Class October 22 Class October 28 Last Class October 29 Last Class *Absences due to the holiday will be granted an additional make-up class. Early Dance Division 2017-2018 Session 2 November 4 – January 22 Monday Classes Tuesday Classes November 6 Class November 7 Class November 13 Class November 14 Class November 20 No Class November 21 No Class November 27 Class November 28 Class December 4 Class December 5 Class December 11 Class December 12 Class December 18 Class December 19 Class December 25 No Class December 26 No Class January 1 No Class January 2 No Class January 8 Class -

January 9, 2020 Farmington Public Library, Main Branch, Conference Room A
MEETING MINUTES CITY OF FARMINGTON HILLS COMMISSION ON CHILDREN YOUTH & FAMILIES JANUARY 9, 2020 FARMINGTON PUBLIC LIBRARY, MAIN BRANCH, CONFERENCE ROOM A. located at 43737 W. TWELVE MILE RD. 48334 CALLED TO ORDER BY: Chair Kathy Ashcraft at 6:00 pm. MEMBERS PRESENT: Kathy Ashcraft, Ed Cherkinsky, Joan McGlincy, Anwar Mahmood, Bette Rose, Sharon Snodgrass and Brian Spitsbergen. MEMBERS ABSENT: Diane Hague and Mitch Seelye OTHERS PRESENT: Farmington and Farmington Hills Council, City, or Staff Liaison members and Alternate and Associates members: Todd Anderson, Mary Newlin, Dan Rodriguez, Lauren Savage and Kristel Sexton. APPROVAL OF AGENDA: MOTION by Rose, support by McGlincy to approve the Agenda of January 9, Motion approved. APPROVAL OF MINUTES -November 7, 2019: MOTION by Rose, support by Snodgrass to approve the minutes of October 3. Motion carried unanimously. INTRODUCTIONS: Everyone at the Meeting introduced themselves. YOUTH DIVISION UPDATE: Tabled until February Meeting. CALL TO ACTION UPDATE: Tabled until February Meeting. ISSUES COMMITTEE UPDATE: Kathy Ashcraft: The Issues Committee and Tech Night were explained. There are 14 vendors signed up for the Tech Event and a final list will be furnished to City Council liaison, Mary Newlin. Assignments and commitments were confirmed. The next meeting is scheduled for Monday, February 3 in the Conference Room at the Costick Center. SPOTLIGHT SHOW UPDATE: Sharon Snodgrass: The Spotlight show was described. The shows can be accessed through the CYF website and some shows have a short excerpt posted on Facebook. The current shows including vaping which was filmed at St. Joseph Mercy Canton Health Center and its Health Exploration Center and another on Fire Safety featuring Todd Anderson, Commander at Farmington Public Safety and Detective James Wren, Fire Marshall of City of Farmington Public Safety Operations Bureau. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -
Flex Dates.Xlsx
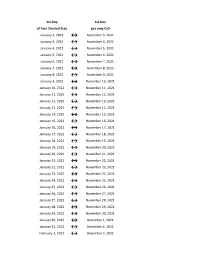
1st Day 1st Day of Your Desired Stay you may Call January 2, 2022 ↔ November 3, 2021 January 3, 2022 ↔ November 4, 2021 January 4, 2022 ↔ November 5, 2021 January 5, 2022 ↔ November 6, 2021 January 6, 2022 ↔ November 7, 2021 January 7, 2022 ↔ November 8, 2021 January 8, 2022 ↔ November 9, 2021 January 9, 2022 ↔ November 10, 2021 January 10, 2022 ↔ November 11, 2021 January 11, 2022 ↔ November 12, 2021 January 12, 2022 ↔ November 13, 2021 January 13, 2022 ↔ November 14, 2021 January 14, 2022 ↔ November 15, 2021 January 15, 2022 ↔ November 16, 2021 January 16, 2022 ↔ November 17, 2021 January 17, 2022 ↔ November 18, 2021 January 18, 2022 ↔ November 19, 2021 January 19, 2022 ↔ November 20, 2021 January 20, 2022 ↔ November 21, 2021 January 21, 2022 ↔ November 22, 2021 January 22, 2022 ↔ November 23, 2021 January 23, 2022 ↔ November 24, 2021 January 24, 2022 ↔ November 25, 2021 January 25, 2022 ↔ November 26, 2021 January 26, 2022 ↔ November 27, 2021 January 27, 2022 ↔ November 28, 2021 January 28, 2022 ↔ November 29, 2021 January 29, 2022 ↔ November 30, 2021 January 30, 2022 ↔ December 1, 2021 January 31, 2022 ↔ December 2, 2021 February 1, 2022 ↔ December 3, 2021 1st Day 1st Day of Your Desired Stay you may Call February 2, 2022 ↔ December 4, 2021 February 3, 2022 ↔ December 5, 2021 February 4, 2022 ↔ December 6, 2021 February 5, 2022 ↔ December 7, 2021 February 6, 2022 ↔ December 8, 2021 February 7, 2022 ↔ December 9, 2021 February 8, 2022 ↔ December 10, 2021 February 9, 2022 ↔ December 11, 2021 February 10, 2022 ↔ December 12, 2021 February -
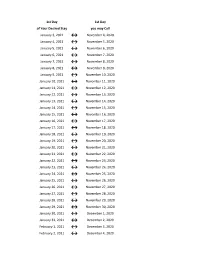
Flex Dates.Xlsx
1st Day 1st Day of Your Desired Stay you may Call January 3, 2021 ↔ November 4, 2020 January 4, 2021 ↔ November 5, 2020 January 5, 2021 ↔ November 6, 2020 January 6, 2021 ↔ November 7, 2020 January 7, 2021 ↔ November 8, 2020 January 8, 2021 ↔ November 9, 2020 January 9, 2021 ↔ November 10, 2020 January 10, 2021 ↔ November 11, 2020 January 11, 2021 ↔ November 12, 2020 January 12, 2021 ↔ November 13, 2020 January 13, 2021 ↔ November 14, 2020 January 14, 2021 ↔ November 15, 2020 January 15, 2021 ↔ November 16, 2020 January 16, 2021 ↔ November 17, 2020 January 17, 2021 ↔ November 18, 2020 January 18, 2021 ↔ November 19, 2020 January 19, 2021 ↔ November 20, 2020 January 20, 2021 ↔ November 21, 2020 January 21, 2021 ↔ November 22, 2020 January 22, 2021 ↔ November 23, 2020 January 23, 2021 ↔ November 24, 2020 January 24, 2021 ↔ November 25, 2020 January 25, 2021 ↔ November 26, 2020 January 26, 2021 ↔ November 27, 2020 January 27, 2021 ↔ November 28, 2020 January 28, 2021 ↔ November 29, 2020 January 29, 2021 ↔ November 30, 2020 January 30, 2021 ↔ December 1, 2020 January 31, 2021 ↔ December 2, 2020 February 1, 2021 ↔ December 3, 2020 February 2, 2021 ↔ December 4, 2020 1st Day 1st Day of Your Desired Stay you may Call February 3, 2021 ↔ December 5, 2020 February 4, 2021 ↔ December 6, 2020 February 5, 2021 ↔ December 7, 2020 February 6, 2021 ↔ December 8, 2020 February 7, 2021 ↔ December 9, 2020 February 8, 2021 ↔ December 10, 2020 February 9, 2021 ↔ December 11, 2020 February 10, 2021 ↔ December 12, 2020 February 11, 2021 ↔ December 13, 2020 -
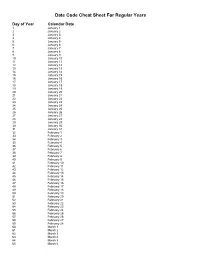
Julian Date Cheat Sheet for Regular Years
Date Code Cheat Sheet For Regular Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 March 1 61 March 2 62 March 3 63 March 4 64 March 5 65 March 6 66 March 7 67 March 8 68 March 9 69 March 10 70 March 11 71 March 12 72 March 13 73 March 14 74 March 15 75 March 16 76 March 17 77 March 18 78 March 19 79 March 20 80 March 21 81 March 22 82 March 23 83 March 24 84 March 25 85 March 26 86 March 27 87 March 28 88 March 29 89 March 30 90 March 31 91 April 1 92 April 2 93 April 3 94 April 4 95 April 5 96 April 6 97 April 7 98 April 8 99 April 9 100 April 10 101 April 11 102 April 12 103 April 13 104 April 14 105 April 15 106 April 16 107 April 17 108 April 18 109 April 19 110 April 20 111 April 21 112 April 22 113 April 23 114 April 24 115 April -

January 9, 2020 Eagle Flyer
January 9, 2020 Eagle Flyer https://mailchi.mp/c8678547d18f/january-9-2020-eagle-flyer Subscribe Past Issues Translate RSS Here's the latest news and information from Grace Academy! View this email in your browser Come out and support our basketball teams! Pictured HS Girls (L-R): Aeris, Heidi, Kathryn, Heather, and Emily. 1 of 3 1/13/2020, 2:15 PM 1/13/2020, 2:15 PM January 9, 2020 Eagle Flyer https://mailchi.mp/c8678547d18f/january-9-2020-eagle-flyer Subscribe Past Issues Translate RSS The Principal Observes Re-Enrollment Rally A few years ago, we started holding an annual Re-Enrollment Rally in order to highlight re- enrollment information and to build anticipation for the following year. Once again, we have an informative, helpful, and fun rally planned for Thursday, January 16, at 6:45 p.m. in the gym. As always, the rally is our kick-off to the enrollment season, but this year is particularly important because I will be giving more details about new continuous enrollment policies. This will be my only opportunity to explain to our families in a face-to-face environment some of the changes that we are making to streamline our processes. Though we are only making small adjustments, they require that we change some of the words regarding enrollment. When families re-enroll this year the documents will be a little different and I want people prepared. We will put the information out through email as well. Like last year, we will give school spirit thank-you gifts as people enter the gym, and we end with raffle drawings that include scholarships to help families with next year’s tuition. -

January 9-15, 2020
Highlighted Activity for January 9-15, 2020 During the last seven-day period, the Police Department handled 366 service events, resulting in 56 investigations. To see a complete listing of crimes reported, go to http://www.crimemapping.com/map/ca/monrovia for crime mapping. For Police Department news and information, visit our website and follow us on Twitter, Facebook, Instagram or Nextdoor. Domestic Violence – Suspect Arrested January 9 at 10:50 a.m., a female subject called police to report her husband pushed her while at their home in the 100 block of W. Cypress. Officers arrived and contacted both parties. The couple was involved in an argument that escalated into a physical altercation and the female subject sustained multiple injuries. The male subject was arrested for domestic violence and taken into custody. Wanted Person / Resisting Arrest – Suspect Arrested January 9 at 1:54 p.m., a resident in the 500 block of W. Colorado called police to report seeing possible drug activity. When the officer arrived, he saw a vehicle matching the description provided by the caller. A traffic stop was conducted, and the investigation revealed one of the occupants in the vehicle was a wanted person. The subject initially resisted arrest, but was eventually arrested and taken into custody. Driving Under the Influence – Suspect Arrested January 10 at 12:39 a.m., an officer was patrolling the 700 block of S. Magnolia, when he saw a vehicle commit several traffic violations. A traffic stop was conducted and the officer spoke with the driver. After field sobriety tests were conducted, the driver was arrested for DUI. -

January 9, 2020 (252) 636-6602
Board of Commissioners Administration Building Thomas F. Mark, Chairman 406 Craven Street Jason R. Jones, Vice Chairman New Bern, NC 28560 Denny Bucher Fax 252-636-2728 George S. Liner [email protected] Theron L. McCabe Etteinne “E.T.” Mitchell Johnnie Sampson, Jr. Administrative Staff Jack B. Veit, III, County Manager Commissioners 252-636-6601 Gene Hodges, Assistant County Manager Manager 252-636-6600 Nan Holton, Clerk to the Board Finance 252-636-6603 Amber M. Parker, Human Resources Director Human Resources 252-636-6602 Craig Warren, Finance Director FOR IMMEDIATE RELEASE Media Contact: Amber M. Parker News Release: January 9, 2020 (252) 636-6602 Craven County Assessor’s Office Implements Online Listing for 2020 Personal Property Tax Craven County, N.C. – The Craven County Assessor’s Office has implemented online listing as an option for taxpayers to list their 2020 personal property owned as of January 1, 2020. Tax listing began January 2, 2020 and must be submitted no later than Friday, January 31, 2020 in order to avoid late listing penalties. To list personal property through the online system, taxpayers will need to first receive their 2020 Personal Property Tax Listing Form via U.S. Mail. Tax listing forms were mailed out by the Craven County Assessor’s Office between January 2, 2020 and January 7, 2020. The 2020 Personal Property Tax Listing Forms mailed to taxpayers will include an Online Record number on the form that will be required to access the online listing form. Once taxpayers receive their listing forms they can go online to complete their listing at http://bit.ly/craven2020personalproperty. -

Early Dance Division Session 1 2012-2013
Early Dance Division Session 1 2012-2013 *Classes will be held. Absences due to the holiday will be granted make-up class. Monday Classes Tuesday Classes September 10 Class September 11 Class September 17* Class September 18 Class September 24 Class September 25 Class October 1 Class October 2 Class October 8 Class October 9 Class October 15 Class October 16 Class October 22 Class October 23 Class October 29 Last Class October 30 Last Class Wednesday Classes Thursday Classes September 12 Class September 13 Class September 19 Class September 20 Class September 26* Class September 27 Class October 3 Class October 4 Class October 10 Class October 11 Class October 17 Class October 18 Class October 24 Class October 25 Class October 31 Last Class November 1 Last Class Friday Classes Saturday Classes September 14 Class September 8 Class September 21 Class September 15 Class September 28 Class September 22 Class October 5 Class September 29 Class October 12 Class October 6 Class October 19 Class October 13 Class October 26 Class October 20 Class November 2 Last Class October 27 Last Class Sunday Classes September 9 Class September 16 Class September 23 Class September 30 Class October 7 Class October 14 Class October 21 Class October 28 Last Class Early Dance Division Session 2 2012-2013 Monday Classes Tuesday Classes November 5 Class November 6 Class November 12 Class November 13 Class November 19 No Class November 20 No Class November 26 Class November 27 Class December 3 Class December 4 Class December 10 Class December 11 Class December 17 -
CHED 501-SECTION 1 F21 CHED 501 SECTION 2 F21 Week 1
INDIVIDUAL SESSIONS INDIVIDUAL SESSIONS CHED 501-SECTION 1 F21 CHED 501 SECTION 2 F21 Week 1 - September 5 - September 11 Week 1 - October 10 - October 16 Week 2 - September 12 - September 18 Week 2 - October 17 - October 23 Week 3 - September 19 - September 25 Week 3 - October 24 - October 30 Week 4 - September 26 - October 2 Week 4 - October 31 - November 6 Week 5 - October 3 - October 9 Week 5 - November 7 - November 13 CHED 502 SECTION 1 F21 CHED 502 -SECTION 1 SP22 Week 1 - October 10 - October 16 Week 1 - January 9 - January 15 Week 2 - October 17 - October 23 Week 2 - January 16 - January 22 Week 3 - October 24 - October 30 Week 3 - January 23 - January 29 Week 4 - October 31 - November 6 Week 4 - January 30 - February 5 Week 5 - November 7 - November 13 Week 5 - February 6 - February 12 CHED 503 SECTION 1 F21 CHED 503 SECTION 1 SP22 Week 1 - November 14 - November 20 Week 1 - January 9 - January 15 Week 2 - November 21 - November 27 Week 2 - January 16 - January 22 Week 3 - November 28 - December 4 Week 3 - January 23 - January 29 Week 4 - December 5 - December 11 Week 4 - January 30 - February 5 Week 5 - December 12 - December 18 Week 5 - February 6 - February 12 INDIVIDUAL SESSIONS INDIVIDUAL SESSIONS INDIVIDUAL SESSIONS CHED 501 SECTION 1 SP22 CHED 501 SECTION 2 SP22 Week 1 - January 9 - Janaury 15 Week 1 - April 3 - April 9 Week 2 - January 16 - January 22 Week 2 - April 10 - April 16 Week 3 - January 23 - January 29 Week 3 - April 17 - April 23 Week 4 - January 30 - February 5 Week 4 - April 24 - April 30 Week 5 - February -

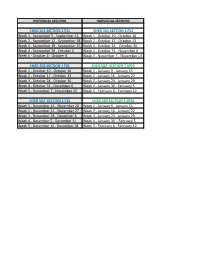
Date of Close Contact Exposure
Date of Close Contact Exposure 7 days 10 days 14 days Monday, November 16, 2020 Tuesday, November 24, 2020 Friday, November 27, 2020 Tuesday, December 1, 2020 Tuesday, November 17, 2020 Wednesday, November 25, 2020 Saturday, November 28, 2020 Wednesday, December 2, 2020 Wednesday, November 18, 2020 Thursday, November 26, 2020 Sunday, November 29, 2020 Thursday, December 3, 2020 Thursday, November 19, 2020 Friday, November 27, 2020 Monday, November 30, 2020 Friday, December 4, 2020 Friday, November 20, 2020 Saturday, November 28, 2020 Tuesday, December 1, 2020 Saturday, December 5, 2020 Saturday, November 21, 2020 Sunday, November 29, 2020 Wednesday, December 2, 2020 Sunday, December 6, 2020 Sunday, November 22, 2020 Monday, November 30, 2020 Thursday, December 3, 2020 Monday, December 7, 2020 Monday, November 23, 2020 Tuesday, December 1, 2020 Friday, December 4, 2020 Tuesday, December 8, 2020 Tuesday, November 24, 2020 Wednesday, December 2, 2020 Saturday, December 5, 2020 Wednesday, December 9, 2020 Wednesday, November 25, 2020 Thursday, December 3, 2020 Sunday, December 6, 2020 Thursday, December 10, 2020 Thursday, November 26, 2020 Friday, December 4, 2020 Monday, December 7, 2020 Friday, December 11, 2020 Friday, November 27, 2020 Saturday, December 5, 2020 Tuesday, December 8, 2020 Saturday, December 12, 2020 Saturday, November 28, 2020 Sunday, December 6, 2020 Wednesday, December 9, 2020 Sunday, December 13, 2020 Sunday, November 29, 2020 Monday, December 7, 2020 Thursday, December 10, 2020 Monday, December 14, 2020 Monday, November