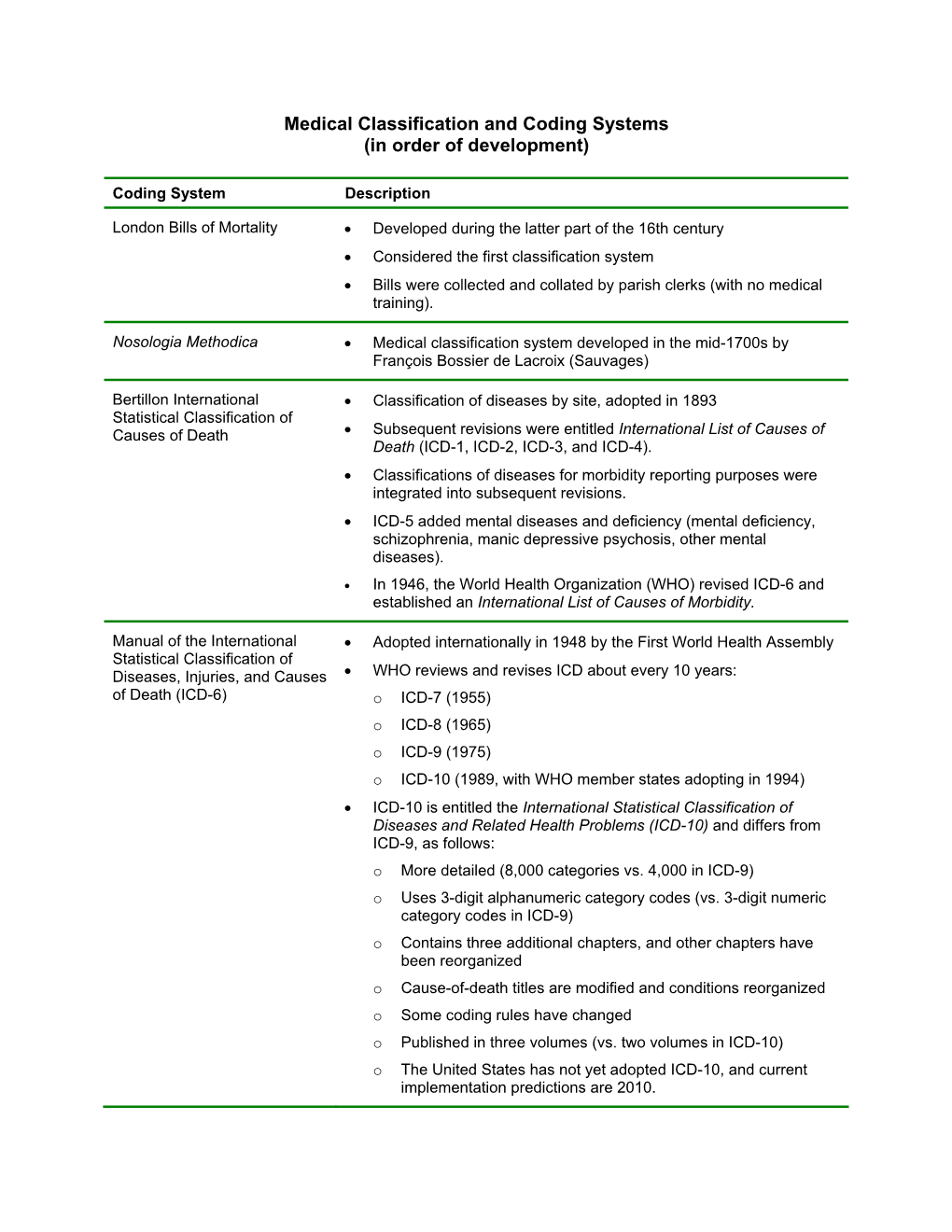
Medical Classification and Coding Systems (In Order of Development)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
UB04 Hospital Billing Instructions & Revenue Code Matrix
Maryland Department of Health Medical Assistance UB04 Hospital Billing Instructions & Revenue Code Matrix Revised 11/2017 Medical Assistance Problem Resolution Institutional Hotline: 410-767-5457 Nevis Smith, Division Chief, MAPR UB04 Hospital Instructions TABLE of CONTENTS Introduction 7 Electronic Verification System (EVS) 9 Sample UB04 11 UB04 FORM LOCATORS FL 01 Billing Provider Name, Address, and Telephone Number 12 FL 02 Pay-to Name and Address 12 FL 03a Patient Control Number 12 FL 03b Medical/Health Record Number 12 FL 04 Type of Bill 12 FL 05 Federal Tax No 17 FL 06 Statement Covers Period (From - Through) 17 FL 07 Reserved for Assignment by NUBC 17 FL 08 Patient Name – Identifier 18 FL 09 Patient address, city, State, zip code, and county code 18 FL 10 Patient Birth Date 18 FL 11 Patient Sex 18 FL 12 Admission/Start of Care Date 18 FL 13 Admission Hour 18 FL 14 Priority (Type) of Visit 19 FL 15 Source of Referral for Admission or Visit 19 FL 16 Discharge Hour 21 FL 17 Patient Status 21 FL 18-28 Condition Codes 23 FL 29 Accident State 32 FL 30 Reserved for Assignment by NUBC 32 FL 31-34 Occurrence Codes and Dates 32 FL 35-36 Occurrence Span Codes and Dates 36 FL 37 NOT USED 38 FL 38 Responsible party name and address 38 FL 39-41 Value Codes and Amounts 38 FL 42 Revenue Codes 42 FL 43 National Drug Code (NDC) Reporting 43 FL 44 HCPCS/Accommodation Rates/HIPPS Rate Codes 45 (HCPCS & HIV Testing Instructions) 45 FL 45 Service Date 46 FL 46 Units of Service 46 FL 47 Total Charges 46 FL 48 Non-Covered Charges 47 FL 49 Reserved for -

Maryland PBHS Provider Billing Appendix
Maryland PBHS Provider Billing Appendix 1. Billing Appendix Overview This Maryland PBHS Provider Billing Appendix (Billing Appendix) is included in the Optum Maryland Provider Manual by reference in section 13 Claim Submission. Note: Information contained in this Billing Appendix may be periodically updated or further explained through Provider Alerts. 2. General Claim Submission Guidelines Claims may be submitted online using Incedo Provider Portal (formerly known as Provider Connect), through a clearinghouse using Electronic Data Interchange (EDI) with 837batch files or by U.S. Mail. Online and Electronic Claim Submission For Incedo Provider Portal: After logging into Incedo Provider Portal, use the Incedo Provider Portal User Guide for instructions on entering a claim or for submitting an electronic file of claims. The link to the Incedo Provider Portal guide is found at maryland.optum.com > Behavioral Health Providers. For EDI/Electronic claims: Electronic Data Interchange (EDI) is the exchange of information for routine business transactions in a standardized computer format; for example, data interchange between a practitioner (physician, psychologist, social worker) and a payer. You may choose any clearinghouse vendor to submit claims using EDI. For PBHS claim submissions, use Payer ID OMDBH. The link to the 837i and 837p companion guides is maryland.optum.com Paper Claim Submission For U.S. Mail (paper claims): Optum Maryland will accept paper CMS-1500 forms for practitioner/professional services or Uniform Billing (UB)-04 forms for inpatient and outpatient facility claims. The mailing address for completed claim forms and required attachments is: Optum Maryland P.O. Box 30531 Salt Lake City, UT 84130 1 | P a g e BH2536_Billing Appendix 122019 Optum Maryland Please see the section on Paper claim submission for more specific instructions for use of CMS-1500 and UB-04 claim forms. -

A Reason for Visit Classification for Ambulatory Care
DATA EVALUATION AND METHODS RESEARCH Series 2 Number 78 A Reasonfor Visit Classification for AmbulatoryCare This report presents a classification system developed to code rea- sons for seeking ambulatory medical care. DHEW Publication No. (PHS) 79-1352 U.S. DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service Office of the Assistant Secretary for Health National Center for Health Statistics Hyattsville, Md. February 1979 Library of Congress Cataloging in Publication Data Schneider, Don. A reason for visit classification for ambulatory care. (Vital and health statistics: Series 2, Data evaluation and methods research; no. 78) (DHEW publication; no. (PHS) 79-1352) Includes bibliographical references and index. 1. Nosology. 2. Ambulatory medical care. I. Appleton, Linda, joint author. II. McLemore, Thomas, ,joint author. III. Title. IV. Series: United States. National Center for Health Sta- tistics. Vital and health statistics: Series 2, Data evaluation and methods research; no. 78. V. Series: United States. Dept. of Health, Education and Welfare. DHEW publication; no. (PHS) 79-1352. [DNLM: 1. Ambulatory care. 2. Classification. W2 A N148vb no. 78] RA409.U45 no. 78 [RB115] 312’.07’23s [616’.001’2] 78-11549 NATIONAL CENTER FOR HEALTH STATISTICS DOROTHY P. RICE, Director ROBERT A. ISRAEL, Deputy Director JACOB J. FELDMAN, Ph.D., Associate Director for Analysis GAIL F. FISHER, Ph.D., Associate Director for the Cooperative Health Statistics System ELIJAH L. WHITE, Associate Director for Data Systems JAMES T. BAIRD, JR., Ph.D., Associate .Directorfor International Statistics ROBERT C, HUBER, Associate Director for Management MONROE G. SIRKEN, Ph. D., Associate Director for Mathematiccd Statistics PETER L. HURLEY, Associate Director for Operations JAMES M. -

Section 4 Procedure Codes
Home Health Services Provider Manual Manual Updated 06/01/18 SECTION 4 PROCEDURE CODES TABLE OF CONTENTS PROCEDURE CODES 1 PROCEDURE CODES .............................................................................................................. 1 MODIFIERS ............................................................................................................................ 1 DIAGNOSIS CODES ................................................................................................................. 1 INCONTINENCE SUPPLIES PROCEDURE CODES ......................................................................... 2 i Home Health Services Provider Manual Manual Updated 06/01/18 SECTION 4 PROCEDURE CODES PROCEDURE CODES PROCEDURE CODES The following procedure codes will be used for home health visits: T1030 Nursing care by a Registered Nurse T1030 Pediatric Home Health nursing care T1031 Nursing care by a Licensed Practical Nurse T1031 Nursing Visit – Stabilized Patient T1021 Home Health Aide Visit T1028 Assessment Visit DME Evaluation A9900 Supplies S9127 Social Work Services to Enhance the Effectiveness of Home Health S9128 Speech Therapy S9129 Occupational Therapy S9131 Physical Therapy 36415 Venipuncture MODIFIERS Two nursing care visits, medically justified, for the same date of service shall be allowed under procedure code T1030 with a modifier 76 (repeat procedure or service by same physician or other qualified health care professional). Modifier 76 shall be recorded for the second visit only, and reflected on the CMS-1500 -

ICD-10 International Statistical Classification of Diseases and Related Health Problems
ICD-10 International Statistical Classification of Diseases and Related Health Problems 10th Revision Volume 2 Instruction manual 2010 Edition WHO Library Cataloguing-in-Publication Data International statistical classification of diseases and related health problems. - 10th revision, edition 2010. 3 v. Contents: v. 1. Tabular list – v. 2. Instruction manual – v. 3. Alphabetical index. 1.Diseases - classification. 2.Classification. 3.Manuals. I.World Health Organization. II.ICD-10. ISBN 978 92 4 154834 2 (NLM classification: WB 15) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

International Classification of Diseases- 10Th Revision (ICD-10)
Massachusetts Deaths 1999 Frequently Asked Questions: International Classification of Diseases- 10th Revision (ICD-10) Effective with data year 1999, the International Classification of Diseases, Tenth Revision (ICD-10) is used to code and classify causes of death. This change in coding systems will affect the comparison of mortality data between 1999 and previous years. Definitions and Concepts What is ICD-10? ICD-10 is an abbreviation for the International Classification of Diseases- Tenth revision. The International Classification of Diseases is a classification system developed by the World Health Organization (WHO). The United States uses the ICD in accordance with an international agreement. The purpose of an international classification system is to promote international comparability in collecting, classifying, and tabulating mortality statistics. Why has the ICD been revised? The ICD is revised to reflect changes in medical classification practices. The ICD was first implemented in 1900, and has undergone revisions approximately every ten years, except for the Ninth revision which was in effect between 1979-1998. There has been an increase in the number of specific cause of death codes from about 4,000 codes in ICD-9 to about 8,000 codes in ICD-10. Beginning with 1999, mortality data are coded according to the Tenth revision of the ICD. Can I compare data classified in ICD-10 to data classified in ICD-9? Differences in the coding between ICD-9 and ICD-10 make direct comparisons between the two classification systems difficult for three reasons: 1) there have been changes made in the codes that are assigned to causes of death; 2) there have been changes to the rules used to determine the underlying cause of death; and 3) there have been changes in the codes that comprise the leading cause of death categories. -

1 the Business of Medicine
Chapter 1 The Business of Medicine Coding as a Profession language, a patient’s condition, or the care provided can change code selection completely. Each time you receive health care, a record is maintained of the resulting observations, medical or surgical inter- Technicians who specialize in coding are medical coders ventions, and treatment outcomes. This medical record or coding specialists. Medical coders assign a code to includes information concerning your symptoms and each diagnosis, service/procedure, and (when applicable) medical history, the results of examinations, reports of supply, using classification systems. The classification X-rays and laboratory tests, diagnoses, and treatment system determines the amount health care providers plans. will be reimbursed if the patient is covered by Medi- care, Medicaid, or other insurance programs using the At its most basic, coding is the process of translating system. this written or dictated medical record into a series of numeric or alpha-numeric codes. There are sepa- If the medical record is inaccurate or incomplete, it rate code sets to describe diagnoses, medical and will not translate properly to the language of codes and surgical services/procedures, and supplies. These reimbursement for services may be lost. The coder must code sets serve as a common “shorthand” language to evaluate the medical record for completeness and accu- ease data collection (for example, to track disease), to racy and communicate regularly with physicians and evaluate the quality of care, and to determine costs and other health care professionals to clarify diagnoses or reimbursement. to obtain additional patient information. Coders may use computer programs to tabulate and analyze data to Coders may use several coding systems, such as those improve patient care, better control cost, provide docu- required for ambulatory settings, physician offices, mentation for use in legal actions, or use in research or long-term care. -

ICF: REPRESENTING the PATIENT BEYOND a MEDICAL CLASSIFICATION of DIAGNOSES Posted on July 17, 2009 by Administrator
ICF: REPRESENTING THE PATIENT BEYOND A MEDICAL CLASSIFICATION OF DIAGNOSES Posted on July 17, 2009 by Administrator Category: Clinical Terms & Vocabularies Tag: ICF Page: 1 by Kathy Giannangelo, RHIA, CCS; Sue Bowman, RHIA, CCS; Michelle Dougherty, RHIA, CHP; and Susan Fenton, MBA, RHIA Abstract The International Classification of Functioning, Disability and Health (ICF) is a component essential to ensuring the collection of accurate and complete healthcare data that correctly reflect the care provided to individuals. In fact, many countries outside of the United States have found uses for ICF. While research continues in the United States on the potential value of implementing ICF, deliberations are establishing the need to implement ICF to develop knowledge about the physical, mental, and social functioning of patients. In the course of these deliberations, issues related to current data collection activities, the use of ICF in an electronic health record (EHR) system, training requirements, and terminology maps are beginning to emerge. Introduction The International Classification of Functioning, Disability and Health (ICF) is one of the World Health Organization’s Family of International Classifications (WHO-FIC).1 The purpose of WHO-FIC is to promote the appropriate selection of classifications in the range of settings in the healthcare field around the world. Since a single classification system cannot encompass all types of healthcare information or provide the level of detail desired for various uses of healthcare data, multiple classifications have been developed to meet specific user requirements. WHO-FIC provides a framework to code a wide range of information about health (for example, diagnosis, functioning, disability, and reasons for contact with health services) and uses standardized language, permitting communication about health and healthcare around the world and among various disciplines and sciences. -

Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Development of the ICD-10 Procedure Coding System (ICD-10-PCS) Richard F. Averill, M.S., Robert L. Mullin, M.D., Barbara A. Steinbeck, RHIT, Norbert I. Goldfield, M.D, Thelma M. Grant, RHIA, Rhonda R. Butler, CCS, CCS-P The International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) has been developed as a replacement for Volume 3 of the International Classification of Diseases 9th Revision (ICD-9-CM). The development of ICD-10-PCS was funded by the U.S. Centers for Medicare and Medicaid Services (CMS).1 ICD-10- PCS has a multiaxial seven character alphanumeric code structure that provides a unique code for all substantially different procedures, and allows new procedures to be easily incorporated as new codes. ICD10-PCS was under development for over five years. The initial draft was formally tested and evaluated by an independent contractor; the final version was released in the Spring of 1998, with annual updates since the final release. The design, development and testing of ICD-10-PCS are discussed. Introduction Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro- cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. -

Toward a Preliminary Layered Network Model Representation of Medical Coding in Clinical Decision Support Systems
146 Int'l Conf. Health Informatics and Medical Systems | HIMS'15 | Toward a Preliminary Layered Network Model Representation of Medical Coding in Clinical Decision Support Systems H. Mallah1, I. Zaarour2, A. Kalakech2 1 Doctoral School of Management Information Systems, Lebanese University, Beirut, Lebanon 2 Management Information Systems Department, Lebanese University, Beirut, Lebanon Abstract - The aim of this research is to describe the impact increase in medical errors, poor trainings to human resources of Medical Codes (MC) on building a successful Clinical and their derivatives. Many studies were done on how to Decision Support System (CDSS) that helps in structuring a computerize medical processes, especially critical decisions beneficial Information Model, we highlight a preliminary in medical fields, using Artificial Intelligence. From these Architectural Layered network model to assist health care needs, Clinical Decision Support System (CDSS) and givers and researchers in representing their work in a Medical classification or medical coding gave birth after the unified manner. Via a descriptive methodology, we development of the Electronic Health Record (EHR) and the incorporate the relationship between (MC) and (CDSS), we Computer-based Physician Order Entry (CPOE). CDSS is discussed a brief state of art of (CDSS) as well as medical the key of success of clinical information systems designed coding as a process of converting descriptions of to assist health care providers in decision making during the medical diagnoses and procedures into universal medical process of care. This means that a clinician would cooperate codes and numbers. Integrated with CDSS, medical codes with a CDSS to help determine diagnosis, analysis of patient are illustrated as an advanced search engine in the data. -
(ICD-11) Expert Roundtable Preliminary Meeting Summary
NCVHS International Classification of Diseases, Eleventh Revision (ICD-11) Expert Roundtable Preliminary Meeting Summary Held August 6-7, 2019 Subcommittee on Standards National Committee on Vital and Health Statistics (NCVHS) U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Preliminary Meeting Summary 2 This report was written by NCVHS consultant Jill W. Roberts, MS, and colleagues at Rose Li and Associates, Inc., in collaboration with NCVHS members and staff. NCVHS Members and Staff in Attendance William W. Stead, MD, NCVHS Chair Alexandra Goss, Subcommittee Co-chair* Richard W. Landen, MPH, MBA Co-chair* Nicholas L. Coussoule, Subcommittee (via Webex)* Llewellyn J. Cornelius, PhD, LCSW Denise E. Love, BSN, MBA* Vickie M. Mays, PhD, MSPH Frank Pasquale, JD (via Webex) Debra Strickland, MS (via Webex)* *Member of the Subcommittee on Standards Rebecca Hines, MHS, NCVHS Executive Secretary/Designated Federal Officer Health Scientist National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC) Department of Health and Human Services (HHS) Geneva Cashaw, NCHS, CDC Lorraine Tunis Doo, MPH, Centers for Medicare & Medicaid Services (CMS), HHS Debbie Jackson, MA, NCHS, CDC, HHS Donna Pickett, RHA, MPH, NCHS, CDC, HHS See Appendix B and C for a complete list of meeting participants. Publication Date: October 10, 2019 Preliminary Meeting Summary 3 NCVHS―The National Committee on Vital and Health Statistics NCVHS serves as the advisory committee to the Secretary of Health and Human Services (HHS) on health data, statistics, privacy, national health information policy, and the Health Insurance Portability and Accountability Act (HIPAA) (42 U.S.C. 242k[k]). The Committee also serves as a forum for interaction with interested private-sector groups on important health data issues. -

Understanding Coding in Ophthalmology
Understanding Coding in Ophthalmology Background Information The coding process is the translation of written medical terminology into codes. Medical terminology, as it is written by the clinician to describe a patient’s complaint, problem, diagnosis, treatment or other reason for seeking medical attention, must be translated into a form which can be easily tabulated, aggregated and sorted for statistical analysis in an efficient and meaningful manner. The coding process is a much more complex function than merely assigning a code to a clinical term. After procedures and admissions for surgery (day case or inpatient), the notes are reviewed by a member of your coding staff. They will look through what you have written in the clinical history sheets, operation note and letter to the GP (or electronic equivalents) and must convert the information to recognised codes, using large reference manuals to inform their actions. It is crucial to understand that a coder cannot interpret or extrapolate and can only use exactly what is written in a very strict manner to produce the codes which allow trusts to be paid for work. It’s therefore extremely important that clinicians understand how the system works and what to write down to allow coders to code fully so that hospitals are reimbursed for the work they do. In addition, there are certain rules and hierarchies of combinations of codes which are complex but determine payment which are useful for clinicians to understand the principles of. Currently only inpatient and daycase admissions and procedures are fully coded. Outpatient procedures are coded but attendances without procedures are not coded by diagnosis etc.