Understanding Coding in Ophthalmology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
UB04 Hospital Billing Instructions & Revenue Code Matrix
Maryland Department of Health Medical Assistance UB04 Hospital Billing Instructions & Revenue Code Matrix Revised 11/2017 Medical Assistance Problem Resolution Institutional Hotline: 410-767-5457 Nevis Smith, Division Chief, MAPR UB04 Hospital Instructions TABLE of CONTENTS Introduction 7 Electronic Verification System (EVS) 9 Sample UB04 11 UB04 FORM LOCATORS FL 01 Billing Provider Name, Address, and Telephone Number 12 FL 02 Pay-to Name and Address 12 FL 03a Patient Control Number 12 FL 03b Medical/Health Record Number 12 FL 04 Type of Bill 12 FL 05 Federal Tax No 17 FL 06 Statement Covers Period (From - Through) 17 FL 07 Reserved for Assignment by NUBC 17 FL 08 Patient Name – Identifier 18 FL 09 Patient address, city, State, zip code, and county code 18 FL 10 Patient Birth Date 18 FL 11 Patient Sex 18 FL 12 Admission/Start of Care Date 18 FL 13 Admission Hour 18 FL 14 Priority (Type) of Visit 19 FL 15 Source of Referral for Admission or Visit 19 FL 16 Discharge Hour 21 FL 17 Patient Status 21 FL 18-28 Condition Codes 23 FL 29 Accident State 32 FL 30 Reserved for Assignment by NUBC 32 FL 31-34 Occurrence Codes and Dates 32 FL 35-36 Occurrence Span Codes and Dates 36 FL 37 NOT USED 38 FL 38 Responsible party name and address 38 FL 39-41 Value Codes and Amounts 38 FL 42 Revenue Codes 42 FL 43 National Drug Code (NDC) Reporting 43 FL 44 HCPCS/Accommodation Rates/HIPPS Rate Codes 45 (HCPCS & HIV Testing Instructions) 45 FL 45 Service Date 46 FL 46 Units of Service 46 FL 47 Total Charges 46 FL 48 Non-Covered Charges 47 FL 49 Reserved for -

Maryland PBHS Provider Billing Appendix
Maryland PBHS Provider Billing Appendix 1. Billing Appendix Overview This Maryland PBHS Provider Billing Appendix (Billing Appendix) is included in the Optum Maryland Provider Manual by reference in section 13 Claim Submission. Note: Information contained in this Billing Appendix may be periodically updated or further explained through Provider Alerts. 2. General Claim Submission Guidelines Claims may be submitted online using Incedo Provider Portal (formerly known as Provider Connect), through a clearinghouse using Electronic Data Interchange (EDI) with 837batch files or by U.S. Mail. Online and Electronic Claim Submission For Incedo Provider Portal: After logging into Incedo Provider Portal, use the Incedo Provider Portal User Guide for instructions on entering a claim or for submitting an electronic file of claims. The link to the Incedo Provider Portal guide is found at maryland.optum.com > Behavioral Health Providers. For EDI/Electronic claims: Electronic Data Interchange (EDI) is the exchange of information for routine business transactions in a standardized computer format; for example, data interchange between a practitioner (physician, psychologist, social worker) and a payer. You may choose any clearinghouse vendor to submit claims using EDI. For PBHS claim submissions, use Payer ID OMDBH. The link to the 837i and 837p companion guides is maryland.optum.com Paper Claim Submission For U.S. Mail (paper claims): Optum Maryland will accept paper CMS-1500 forms for practitioner/professional services or Uniform Billing (UB)-04 forms for inpatient and outpatient facility claims. The mailing address for completed claim forms and required attachments is: Optum Maryland P.O. Box 30531 Salt Lake City, UT 84130 1 | P a g e BH2536_Billing Appendix 122019 Optum Maryland Please see the section on Paper claim submission for more specific instructions for use of CMS-1500 and UB-04 claim forms. -

Section 4 Procedure Codes
Home Health Services Provider Manual Manual Updated 06/01/18 SECTION 4 PROCEDURE CODES TABLE OF CONTENTS PROCEDURE CODES 1 PROCEDURE CODES .............................................................................................................. 1 MODIFIERS ............................................................................................................................ 1 DIAGNOSIS CODES ................................................................................................................. 1 INCONTINENCE SUPPLIES PROCEDURE CODES ......................................................................... 2 i Home Health Services Provider Manual Manual Updated 06/01/18 SECTION 4 PROCEDURE CODES PROCEDURE CODES PROCEDURE CODES The following procedure codes will be used for home health visits: T1030 Nursing care by a Registered Nurse T1030 Pediatric Home Health nursing care T1031 Nursing care by a Licensed Practical Nurse T1031 Nursing Visit – Stabilized Patient T1021 Home Health Aide Visit T1028 Assessment Visit DME Evaluation A9900 Supplies S9127 Social Work Services to Enhance the Effectiveness of Home Health S9128 Speech Therapy S9129 Occupational Therapy S9131 Physical Therapy 36415 Venipuncture MODIFIERS Two nursing care visits, medically justified, for the same date of service shall be allowed under procedure code T1030 with a modifier 76 (repeat procedure or service by same physician or other qualified health care professional). Modifier 76 shall be recorded for the second visit only, and reflected on the CMS-1500 -

ICD-10 International Statistical Classification of Diseases and Related Health Problems
ICD-10 International Statistical Classification of Diseases and Related Health Problems 10th Revision Volume 2 Instruction manual 2010 Edition WHO Library Cataloguing-in-Publication Data International statistical classification of diseases and related health problems. - 10th revision, edition 2010. 3 v. Contents: v. 1. Tabular list – v. 2. Instruction manual – v. 3. Alphabetical index. 1.Diseases - classification. 2.Classification. 3.Manuals. I.World Health Organization. II.ICD-10. ISBN 978 92 4 154834 2 (NLM classification: WB 15) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/copyright_form). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

1 the Business of Medicine
Chapter 1 The Business of Medicine Coding as a Profession language, a patient’s condition, or the care provided can change code selection completely. Each time you receive health care, a record is maintained of the resulting observations, medical or surgical inter- Technicians who specialize in coding are medical coders ventions, and treatment outcomes. This medical record or coding specialists. Medical coders assign a code to includes information concerning your symptoms and each diagnosis, service/procedure, and (when applicable) medical history, the results of examinations, reports of supply, using classification systems. The classification X-rays and laboratory tests, diagnoses, and treatment system determines the amount health care providers plans. will be reimbursed if the patient is covered by Medi- care, Medicaid, or other insurance programs using the At its most basic, coding is the process of translating system. this written or dictated medical record into a series of numeric or alpha-numeric codes. There are sepa- If the medical record is inaccurate or incomplete, it rate code sets to describe diagnoses, medical and will not translate properly to the language of codes and surgical services/procedures, and supplies. These reimbursement for services may be lost. The coder must code sets serve as a common “shorthand” language to evaluate the medical record for completeness and accu- ease data collection (for example, to track disease), to racy and communicate regularly with physicians and evaluate the quality of care, and to determine costs and other health care professionals to clarify diagnoses or reimbursement. to obtain additional patient information. Coders may use computer programs to tabulate and analyze data to Coders may use several coding systems, such as those improve patient care, better control cost, provide docu- required for ambulatory settings, physician offices, mentation for use in legal actions, or use in research or long-term care. -

Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Development of the ICD-10 Procedure Coding System (ICD-10-PCS) Richard F. Averill, M.S., Robert L. Mullin, M.D., Barbara A. Steinbeck, RHIT, Norbert I. Goldfield, M.D, Thelma M. Grant, RHIA, Rhonda R. Butler, CCS, CCS-P The International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) has been developed as a replacement for Volume 3 of the International Classification of Diseases 9th Revision (ICD-9-CM). The development of ICD-10-PCS was funded by the U.S. Centers for Medicare and Medicaid Services (CMS).1 ICD-10- PCS has a multiaxial seven character alphanumeric code structure that provides a unique code for all substantially different procedures, and allows new procedures to be easily incorporated as new codes. ICD10-PCS was under development for over five years. The initial draft was formally tested and evaluated by an independent contractor; the final version was released in the Spring of 1998, with annual updates since the final release. The design, development and testing of ICD-10-PCS are discussed. Introduction Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro- cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. -
(ICD-11) Expert Roundtable Preliminary Meeting Summary
NCVHS International Classification of Diseases, Eleventh Revision (ICD-11) Expert Roundtable Preliminary Meeting Summary Held August 6-7, 2019 Subcommittee on Standards National Committee on Vital and Health Statistics (NCVHS) U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Preliminary Meeting Summary 2 This report was written by NCVHS consultant Jill W. Roberts, MS, and colleagues at Rose Li and Associates, Inc., in collaboration with NCVHS members and staff. NCVHS Members and Staff in Attendance William W. Stead, MD, NCVHS Chair Alexandra Goss, Subcommittee Co-chair* Richard W. Landen, MPH, MBA Co-chair* Nicholas L. Coussoule, Subcommittee (via Webex)* Llewellyn J. Cornelius, PhD, LCSW Denise E. Love, BSN, MBA* Vickie M. Mays, PhD, MSPH Frank Pasquale, JD (via Webex) Debra Strickland, MS (via Webex)* *Member of the Subcommittee on Standards Rebecca Hines, MHS, NCVHS Executive Secretary/Designated Federal Officer Health Scientist National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC) Department of Health and Human Services (HHS) Geneva Cashaw, NCHS, CDC Lorraine Tunis Doo, MPH, Centers for Medicare & Medicaid Services (CMS), HHS Debbie Jackson, MA, NCHS, CDC, HHS Donna Pickett, RHA, MPH, NCHS, CDC, HHS See Appendix B and C for a complete list of meeting participants. Publication Date: October 10, 2019 Preliminary Meeting Summary 3 NCVHS―The National Committee on Vital and Health Statistics NCVHS serves as the advisory committee to the Secretary of Health and Human Services (HHS) on health data, statistics, privacy, national health information policy, and the Health Insurance Portability and Accountability Act (HIPAA) (42 U.S.C. 242k[k]). The Committee also serves as a forum for interaction with interested private-sector groups on important health data issues. -
Methods Series Report #2016-02
HCUP Methods Series Contact Information: Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality 5600 Fishers Lane Room 07W17B Mail Stop 7W25B Rockville, MD 20857 http://www.hcup-us.ahrq.gov For Technical Assistance with HCUP Products: Email: [email protected] or Phone: 1-866-290-HCUP Recommended Citation: Gibson T, Casto A, Young J, Karnell L, Coenen N. Impact of ICD-10- CM/PCS on Research Using Administrative Databases. HCUP Methods Series Report # 2016- 02 ONLINE. July 25, 2016. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. TABLE OF CONTENTS 1. EXECUTIVE SUMMARY ..................................................................................................... I 2. INTRODUCTION ................................................................................................................ 1 3. DIFFERENCES BETWEEN ICD-9-CM AND ICD-10-CM/PCS CODING SYSTEMS ........... 4 Diagnosis Coding Systems ............................................................................................. 4 Procedure Coding Systems ............................................................................................ 7 Focus Areas in the Medical and Surgical Section: Root Operations and Approaches ....10 4. LESSONS FROM DUALLY CODED DATA ........................................................................14 Differences in the ICD-9-CM and ICD-10-CM/PCS Coding Systems .............................14 Changes in Coding Rules ..............................................................................................15 -
New Cognitive Procedure Coding What You Need To
Presented by ASHA’s Health NEW COGNITIVE PROCEDURE CODING Care Economics Committee 2017 ASHA Convention WHAT YOU NEED TO KNOW Los Angeles, California SESSION # 1075 November 9, 2017 1 DISCLOSURES Dee Adams Nikjeh Renee Kinder Katie Holterman Dee is contracted by the US Dept of Renee is paid a salary by Encore Katie is paid a salary by Care Justice as an SLP expert witness. She Rehabilitation, serves on the HCEC and One Management LLC, serves on is co-chair of the HCEC and the AMA the AMA RUC HCPAC, is reimbursed for the HCEC and on the AMA CPT RUC HCPAC, serves on the AMA RUC, HCEC and AMA RUC HCPAC travel, and Editorial Panel, and is reimbursed and is reimbursed for HCEC and received a complimentary conference for HCEC and AMA CPT related AMA RUC HCPAC travel. registration for her participation in a travel. Short Course. Shannon Butkus Mark DeRuiter Tim Weise Shannon owns a private practice, Mark DeRuiter is paid a salary by the Tim is contracted by Blue Cross Blue serves on the HCEC, and is University of Arizona, serves on the Shield of MI as an SLP Reviewer. reimbursed for HCEC related HCEC, is reimbursed for HCEC travel, He serves on the HCEC and is travel. and received a complimentary reimbursed for HCEC-related travel conference registration for his participation with the Research, Academic Town Meeting. 2 HEALTH CARE ECONOMICS COMMITTEE (HCEC) PURPOSE Assist Government Relations and Public Policy Board (GRPP) and cluster staff in determining current economic issues and develop goals for ensuring equitable coverage and reimbursement -

Coding and Documentation of Domestic Violence
Coding and Documentation of Domestic Violence December, 2000 Authored by: William J. Rudman Ph.D. Associate Professor School of Health Related Professions The University of Mississippi Medical Center Edited by Elaine Alpert, MD, MPH Boston University Schools of Public Health and Medicine Lisa James, MA Family Violence Prevention Fund Produced by the Family Violence Prevention Fund Coding and Documentation of Domestic Violence Part I: Introduction and Rationale Introduction Domestic violence (DV) is a major public health problem in the United States, affecting between two and four million women each year.1,2 Women turn to the health care system throughout their lives for routine health maintenance; pregnancy and childbirth; illness or injury care; mental health assessment and treatment; and when assisting or accompanying their children or other family members for their own health care. Doctors, nurses and other providers are urged to screen routinely for DV, yet progress is hindered because health systems lack the data, formalized procedures and the reimbursement schemes to fully implement and sustain published screening guidelines. Documentation and coding of DV can improve our ability to conduct useful research and also positively affect reimbursement for DV screening, identification, assessment, care and follow-up. Improved documentation and coding will thus ultimately improve health services for victims. Although medical record documentation of DV is recommended3 it is still uncommon. Accurate coding of DV is even more unusual. Two -

NC Medicaid: Outpatient Behavioral Health Services
NC Medicaid Medicaid and Health Choice Outpatient Behavioral Health Services Clinical Coverage Policy No. 8C Provided by Direct-Enrolled Providers Amended Date: January 1, 2021 To all beneficiaries enrolled in a Prepaid Health Plan (PHP): for questions about benefits and services available on or after implementation, please contact your PHP. Table of Contents 1.0 Description of the Procedure, Product, or Service ........................................................................... 1 1.1 Definitions .......................................................................................................................... 1 1.1.1 Psychological Testing ............................................................................................ 1 1.1.2 Psychotherapy for Crisis ........................................................................................ 1 2.0 Eligibility Requirements .................................................................................................................. 2 2.1 Provisions............................................................................................................................ 2 2.1.1 General ................................................................................................................... 2 2.1.2 Specific .................................................................................................................. 2 2.2 Special Provisions .............................................................................................................. -
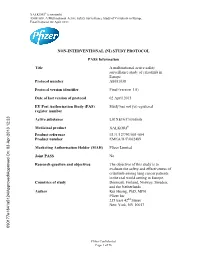
STUDY PROTOCOL PASS Information Title a Multinational Active Safety Surveillance Study of Crizotinib In
XALKORI (crizotinib) A8081038, A Multinational Active Safety Surveillance Study of Crizotinib in Europe Final Protocol, 02 April 2013 NON-INTERVENTIONAL (NI) STUDY PROTOCOL PASS Information Title A multinational active safety surveillance study of crizotinib in Europe Protocol number A8081038 Protocol version identifier Final (version 1.0) Date of last version of protocol 02 April 2013 EU Post Authorisation Study (PAS) Study has not yet registered register number Active substance L01XE16/Crizotinib Medicinal product XALKORI Product reference EU/1/12/793/001-004 Product number EMEA/H/C/002489 Marketing Authorisation Holder (MAH) Pfizer Limited Joint PASS No Research question and objectives The objective of this study is to evaluate the safety and effectiveness of crizotinib among lung cancer patients in the real world setting in Europe. Countries of study Denmark, Finland, Norway, Sweden, and the Netherlands Author Kui Huang, PhD, MPH Pfizer Inc 235 East 42nd Street New York, NY 10017 090177e1841a5124\Approved\Approved On: 03-Apr-2013 12:23 Pfizer Confidential Page 1 of 76 XALKORI (crizotinib) A8081038, A Multinational Active Safety Surveillance Study of Crizotinib in Europe Final Protocol, 02 April 2013 Marketing Authorisation Holder(s) Marketing Authorisation Holder(s) Pfizer Limited Ramsgate Road, Sandwich, Kent CT130NJ United Kingdom MAH contact person Kui Huang, PhD, MPH Pfizer Inc 235 East 42nd Street New York, NY 10017 This document contains confidential information belonging to Pfizer. Except as otherwise agreed to in writing, by accepting or reviewing this document, you agree to hold this information in confidence and not copy or disclose it to others (except where required by applicable law) or use it for unauthorized purposes.