RY2U2 Bridgewater CHCFT HMP Wymott
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Prison Education in England and Wales. (2Nd Revised Edition)
DOCUMENT RESUME ED 388 842 CE 070 238 AUTHOR Ripley, Paul TITLE Prison Education in England and Wales. (2nd Revised Edition). Mendip Papers MP 022. INSTITUTION Staff Coll., Bristol (England). PUB DATE 93 NOTE 30p. AVAILABLE FROMStaff College, Coombe Lodge, Blagdon, Bristol BS18 6RG, England, United Kingdom (2.50 British pounds). PUB TYPE Information Analyses (070) EDRS PRICE MF01/PCO2 Plus Postage. DESCRIPTORS Adult Basic Education; *Correctional Education; *Correctional Institutions; Correctional Rehabilitation; Criminals; *Educational History; Foreign Countries; Postsecondary Education; Prisoners; Prison Libraries; Rehabilitation Programs; Secondary Education; Vocational Rehabilitation IDENTIFIERS *England; *Wales ABSTRACT In response to prison disturbances in England and Wales in the late 1980s, the education program for prisoners was improved and more prisoners were given access to educational services. Although education is a relatively new phenomenon in the English and Welsh penal system, by the 20th century, education had become an integral part of prison life. It served partly as a control mechanism and partly for more altruistic needs. Until 1993 the management and delivery of education and training in prisons was carried out by local education authority staff. Since that time, the education responsibility has been contracted out to organizations such as the Staff College, other universities, and private training organizations. Various policy implications were resolved in order to allow these organizations to provide prison education. Today, prison education programs are probably the most comprehensive of any found in the country. They may range from literacy education to postgraduate study, with students ranging in age from 15 to over 65. The curriculum focuses on social and life skills. -

Development Control Committee Tuesday, 11Th December 2007
Development Control Committee Agenda and Reports For consideration on Tuesday, 11th December 2007 In the Council Chamber Town Hall, Chorley At 6.30 pm PROCEDURE FOR PUBLIC SPEAKING AT MEETINGS OF THE DEVELOPMENT CONTROL COMMITTEE • Persons must give notice of their wish to address the Committee, to the Democratic Services Section by no later than midday, two working days before the day of the meeting. (12 Noon on the Friday prior to the meeting) • One person to be allowed to address the Committee in favour of the officers recommendations on respective planning applications and one person to be allowed to speak against the officer’s recommendations. • In the event of several people wishing to speak either in favour or against the recommendation, the respective group/s will be requested by the Chair of the Committee to select one spokesperson to address the Committee. • If a person wishes to speak either in favour or against an application without anyone wishing to present an opposing argument that person will be allowed to address the Committee. • Each person/group addressing the Committee will be allowed a maximum of three minutes to speak. • The Committees debate and consideration of the planning applications awaiting decision will only commence after all of the public addresses. ORDER OF SPEAKING AT THE MEETINGS 1. The Corporate Director (Business) or her representative will describe the proposed development and recommend a decision to the Committee. A presentation on the proposal may also be made. 2. An objector/supporter will be asked to speak, normally for a maximum of three minutes. -

Mersey Care NHS Foundation Trust Quality Report 2018/19
Mersey Care NHS Foundation Trust Quality Report 2018/19 Page 133 of 284 Contents Page EXTERNAL AUDITOR’S OPINION 135 PART 1 INTRODUCTION & STATEMENT ON QUALITY BY THE 139 CHIEF EXECUTIVE 1.1 Introduction & Statement on Quality by the Chief Executive 139 1.2 Our Strategic Direction: Transforming our Trust 140 1.3 Improving Quality 142 1.4 Pursuing Perfect Care 142 PART 2 PRIORITIES FOR IMPROVEMENT 2019/20 AND 143 STATEMENT OF ASSURANCE FROM THE BOARD 2.1 Priorities for Improvement 2019/20 143 2.2 Review of Quality Performance 2018/19 145 2.3 Statement of Assurance from the Board: Review of Services 159 2.4 Participation in National and Local Clinical Audits and National 161 Confidential Enquires 2.5 NHS Staff Survey Results 2018 163 2.6 Research and Development 165 2.7 Sign Up to Safety Campaign 170 2.8 Commissioning for Quality & Innovation (CQUIN) 178 2.9 Care Quality Commission 188 2.10 Duty of Candour 192 2.11 Data Quality Improvement Plans 194 2.12 Information Governance 195 PART 3 QUALITY INDICATORS 196 3.1 Quality Indicators 196 3.2 Re-admissions 199 3.3 Performance against NHS Improvement’s Single Oversight 200 Framework Indicators 3.4 Stakeholder Metrics 201 Annex 1 Statements from Commissioner, Local Healthwatch 203 Organisations and Overview and Scrutiny Committees Annex 2 Statement of Director’s Responsibilities for the Quality 213 Report Annex 3 Clinical Audit Report 2018/19 213 Page 134 of 284 Independent Practitioner's Limited Assurance Report to the Council of Governors of Mersey Care NHS Foundation Trust on the Quality Report We have been engaged by the Council of Governors of Mersey Care NHS Foundation Trust to perform an independent limited assurance engagement in respect of Mersey Care NHS Foundation Trust’s Quality Report for the year ended 31 March 2019 (the “Quality Report”) and certain performance indicators contained therein against the criteria set out in the ‘NHS Foundation Trust Annual Reporting Manual 2018/19’ and additional supporting guidance in the ‘Detailed requirements for quality reports 2018/19' (the 'Criteria'). -
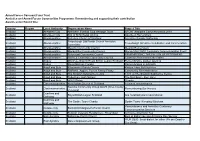
Remembering and Supporting Their Contribution Awards Under Round One
Armed Forces Covenant Fund Trust Armistice and Armed Forces Communities Programme: Remembering and supporting their contribution Awards under Round One Country Region Local Authority Organisation Name Project Title Scotland Aberdeen City Aberdeen Football Club Heritage Trust AFCHT Armistice Commemoration 2018 Scotland Aberdeen City Kirk of St Nicholas Uniting Aberdeen Remembers Scotland Aberdeenshire Belhelvie Church of Scotland Armistice Sunday Gathering Fraserburgh Old Parish Church Armistice Scotland Aberdeenshire Fraserburgh Armistice Celebration and Commeration Committee Scotland Aberdeenshire Mearns Community Council Mearns Remembers Scotland Aberdeenshire Monquhitter Community Council Monquhitter WW1 Centenary Commemoration Event Scotland Aberdeenshire Peterhead Community Council REMEMBERING THE FALLEN OF PETERHEAD Scotland Aberdeenshire Slains & Collieston Community Council Collieston Remembers the Fallen Scotland Angus Montrose Branch Royal British Legion Scotland Remembrance garden opening Scotland Angus Royal Marines Condor Remembrance in Arbroath Scotland Argyll and Bute Kilcalmonell Parish Church Kintyre: Here But Not Here Scotland Argyll and Bute RNRMW, Aggies, Forces Family Friday Community Rememberance Scotland Argyll and Bute The Scottish Submarine Centre 11/11 at The Scottish Submarine Centre Scotland Argyll and Bute Tobermory High School The Mull Boys - their story. Scotland Argyll and Bute WW100Islay Otranto Scotland Clackmannanshire Alva Parish Church of Scotland A time of remembrance Sauchie Community Group QAVS (Wee -

Prison Information Bulletin
ISSN 0254-5225 COUNCIL CONSEIL OF EUROPE DE L'EUROPE Prison Information Bulletin THE COUNCIL OF EUROPE No. 16 - JUNE 1992 5 4003 00194419 7 CONTENTS PRISON INFORMATION BULLETIN Page 1/92 The Demosthenes Programme : a penological challenge ............................................................................. 3 Published twice yearly in French and English, by the Council of Europe The European prison rules: context, philosophy and Issues ................................................................................. 4 Reproduction Articles or extracts may be reproduced on condition that the Cornerstones in a modern treatment philosophy: source is mentioned. A copy should be sent to the Chief Editor. normalisation, openness and responsibility............... 6 The right to reproduce the cover illustration is reserved. The organisation of imprisonment, the treatment of prisoners and the preparation of prisoners for release 13 Correspondence All correspondence should be addressed to the Directorate of Legal Affairs, Division of Crime Problems, Recruitment, training and use of staff ........................ 19 Council of Europe, 67006 Strasbourg, Cedex France News from the member States Statistics on prison population In the member Opinions States of the Council of Europe ................................... 24 Articles published in the Prison Information Bulletin are the authors ’ responsibility alone and do not necessarily reflect the opinions of the Council of Europe. Laws, bills, regulations.................................................... -
HM Prison Wymott
HM Prison Wymott HM Prison Wymott is a Category C men's training prison, located in the village of Ulnes Walton near Leyland, in Lancashire, England Wymott is operated by Her Majesty's Prison Service, and is situated next to HMP Garth The prison has facilities for housing sex offenders, in addition to inmates sentenced for mainstream offences. Contents. Wymott Prison opened in 1979 as short term category C prison In 1986 there was a large prison riot at Wymott which caused serious damage to the fabric of living units of HMP Wymott Wymott is a male category C trainer prison which has facilities for vulnerable prisoners. It opened in 1979 as short term category C prison. Governor: Jayne G. Blake Operational capacity The map created by people like you! HMP Wymott | prison. United Kingdom / England / Croston /. World / United Kingdom / England / Croston World / United Kingdom / England. prison Add category. Upload a photo. Wymott is a male category C trainer prison which has facilities for vulnerable prisoners. We found one dictionary with English definitions that includes the word hm prison wymott: Click on the first link on a line below to go directly to a page where "hm prison wymott" is defined. General (1 matching dictionary). HM Prison Wymott: Wikipedia, the Free Encyclopedia [home, info]. ▸ Words similar to hm prison wymott. ▸ Words that often appear near hm prison wymott. ▸ Rhymes of hm prison wymott. ▸ Invented words related to hm prison wymott. Search for hm prison wymott on Google or Wikipedia. HM Prison Wymott is a Category C men's training prison, located in the village of Ulnes Walton (near Leyland), in Lancashire, England. -
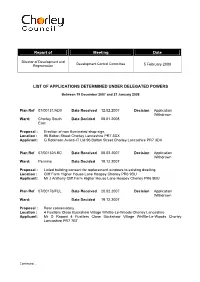
Report of Meeting Date LIST of APPLICATIONS DETERMINED
Report of Meeting Date Director of Development and Development Control Committee Regeneration 5 February 2008 LIST OF APPLICATIONS DETERMINED UNDER DELEGATED POWERS Between 19 December 2007 and 21 January 2008 Plan Ref 07/00131/ADV Date Received 12.02.2007 Decision Application Withdrawn Ward: Chorley South Date Decided 08.01.2008 East Proposal : Erection of non illuminated shop sign, Location : 96 Bolton Street Chorley Lancashire PR7 3DX Applicant: G Robinson Avanti-IT Ltd 96 Bolton Street Chorley Lancashire PR7 3DX Plan Ref 07/00132/LBC Date Received 08.02.2007 Decision Application Withdrawn Ward: Pennine Date Decided 19.12.2007 Proposal : Listed building consent for replacement windows to existing dwelling. Location : Cliff Farm Higher House Lane Heapey Chorley PR6 9BU Applicant: Mr J Anthony Cliff Farm Higher House Lane Heapey Chorley PR6 9BU Plan Ref 07/00176/FUL Date Received 20.02.2007 Decision Application Withdrawn Ward: Date Decided 19.12.2007 Proposal : Rear conservatory Location : 4 Fusiliers Close Buckshaw Village Whittle-Le-Woods Chorley Lancashire Applicant: Mr D Raponi 4 Fusiliers Close Buckshaw Village Whittle-Le-Woods Chorley Lancashire PR7 7BT Continued.... Plan Ref 07/00245/TPO Date Received 26.02.2007 Decision Application Withdrawn Ward: Clayton-le-Woods Date Decided 04.01.2008 North Proposal : Proposed trimming of trees covered by TPO2 (Clayton Le Woods) 1994 Location : 6 Mallards Walk Bamber Bridge Preston PR5 6AY Applicant: Jamel Khalifa 6 Mallards Walk Bamber Bridge Preston PR5 6AY Plan Ref 07/00286/FUL Date Received -
Development Control Committee Tuesday, 9Th October 2007
Development Control Committee Agenda and Reports For consideration on Tuesday, 9th October 2007 In the Council Chamber, Town Hall, Chorley At 6.30 pm PROCEDURE FOR PUBLIC SPEAKING AT MEETINGS OF THE DEVELOPMENT CONTROL COMMITTEE • Persons must give notice of their wish to address the Committee, to the Democratic Services Section by no later than midday, two working days before the day of the meeting. (12 Noon on the Friday prior to the meeting) • One person to be allowed to address the Committee in favour of the officers recommendations on respective planning applications and one person to be allowed to speak against the officer’s recommendations. • In the event of several people wishing to speak either in favour or against the recommendation, the respective group/s will be requested by the Chair of the Committee to select one spokesperson to address the Committee. • If a person wishes to speak either in favour or against an application without anyone wishing to present an opposing argument that person will be allowed to address the Committee. • Each person/group addressing the Committee will be allowed a maximum of three minutes to speak. • The Committees debate and consideration of the planning applications awaiting decision will only commence after all of the public addresses. ORDER OF SPEAKING AT THE MEETINGS 1. The Corporate Director (Business) or her representative will describe the proposed development and recommend a decision to the Committee. A presentation on the proposal may also be made. 2. An objector/supporter will be asked to speak, normally for a maximum of three minutes. -

2019 Koestler Awards Results (At 28.08.19)
2019 Koestler Awards Results (at 28.08.19) . This is the final list of entries which have won awards. If an entry is not listed, it probably did not win an award. We are open all year round to entries from under 18s and will respond to these with feedback and certificates within 6 weeks. Your package must be marked “Under 18s Fast Feedback Programme”. In most artforms, the awards given are as follows: Platinum £100 + certificate Gold £60 + certificate Silver £40 + certificate Bronze £20 + certificate Special Award for Under 18s / Under 25s £25 + certificate First-time Entrant £25 + certificate Highly Commended Certificate Commended Certificate Some awards are generously sponsored and named by Koestler Trust supporters. Every entrant will receive a Participation Certificate, and most will receive written feedback. Certificates, feedback and prize cheques for entrants will be sent by the end of October 2019. “K No” is the Koestler reference number that we allocate to each artwork. Please have this number and your entry details to hand if you have an enquiry about a particular entry. More information from [email protected] or 020 8740 0333. We cannot give out information to third parties. Entrants are not named, but this list shows where entrants have originally entered from – not where they are now. Around 180 examples of visual art, audio, film and writing, have been selected for our annual UK exhibition. This is open to the public from 19 Sept – 03 Nov daily at London’s Southbank Centre. The opening event is on Wednesday 18 Sept from 2pm; all are welcome. -
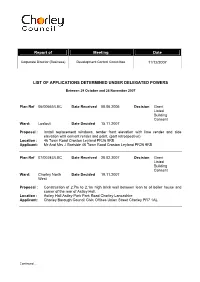
Report of Meeting Date
Report of Meeting Date Corporate Director (Business) Development Control Committee 11/12/2007 LIST OF APPLICATIONS DETERMINED UNDER DELEGATED POWERS Between 29 October and 26 November 2007 Plan Ref 06/00665/LBC Date Received 08.06.2006 Decision Grant Listed Building Consent Ward: Lostock Date Decided 15.11.2007 Proposal : Install replacement windows, render front elevation with lime render and side elevation with cement render and paint. (part retrospective) Location : 46 Town Road Croston Leyland PR26 9RB Applicant: Mr And Mrs J Gartside 46 Town Road Croston Leyland PR26 9RB Plan Ref 07/00243/LBC Date Received 28.02.2007 Decision Grant Listed Building Consent Ward: Chorley North Date Decided 19.11.2007 West Proposal : Construction of 2.7m to 2.1m high brick wall between lean to of boiler house and corner of the rear of Astley Hall. Location : Astley Hall Astley Park Park Road Chorley Lancashire Applicant: Chorley Borough Council Civic Offices Union Street Chorley PR7 1AL Continued.... Plan Ref 07/00375/FUL Date Received 02.04.2007 Decision Permit retrospecti ve planning permission Ward: Chorley South Date Decided 20.11.2007 East Proposal : Retrospective application for the erection of a awning and wall mounted rest to facilitate an external smoking area. Location : Gala Bingo Market Street Chorley PR7 1BD Applicant: Mr Paul Duffree New Castle House Castle Boulevard Nottingham NG7 1FT Plan Ref 07/00602/FUL Date Received 23.05.2007 Decision Permit Full Planning Permission Ward: Eccleston And Date Decided 19.11.2007 Mawdesley Proposal : -

Mersey Care NHS Foundation Trust: Annual Report and Accounts 2018/19
Mersey Care NHS Foundation Trust Annual Report 2018/19 Quality Report 2018/19 Annual Accounts 2018/19 Striving for perfect care and a just culture Page 1 of 284 [page left intentionally blank] Page 2 of 284 Mersey Care NHS Foundation Trust Annual Report and Accounts 2018/19 Presented to Parliament pursuant to Schedule 7, paragraph 25(4)(a) of the National Health Service Act 2006 Page 3 of 284 Copyright © Mersey Care NHS Foundation Trust, 2019. All Rights Reserved. Page 4 of 284 Contents Page Annual Report – 2018/19 7 Quality Report – 2018/19 133 Annual Accounts – 2018/19 217 Page 5 of 284 [page left intentionally blank] Page 6 of 284 Mersey Care NHS Foundation Trust Annual Report 2018/19 Annual Report and Accounts 2018/19 Presented to Parliament pursuant to Schedule 7, paragraph 25(4)(a) of the National Health Service Act 2006 Page 7 of 284 Contents Chapter Page Foreword 9 PART A OVERVIEW 11 1 Introduction 11 2 Risk Management 19 PART B PERFORMANCE REPORT 21 3 Executive Performance Report 21 4 Environment and Sustainability 24 5 Equality, Diversity and Human Rights 27 6 Complaints and Compliments 28 7 Freedom to Speak Up (Whistleblowing) 29 8 Emergency Planning, Resilience and Response 31 9 Finance Director’s Report 32 PART C ACCOUNTABILITY REPORT 37 10 Director’s Report 37 11 Statement of the Chief Executive’s Responsibilities as 60 the Accountable Officer for the Trust 12 Audit Committee 62 13 Remuneration Report 65 14 Staff Report 78 15 Single Oversight Framework 90 16 Annual Governance Statement 94 APPENDICES App A Attendance at Council of Governor Meetings 127 App B Attendance at Board of Directors / Board Committee 129 Meetings Page 8 of 284 FOREWORD Welcome to our annual report covering the financial year 2018/19. -

Independent Investigation Into the Death of Mr Prince Albert Wright, a Prisoner at HMP Wymott, on 19 September 2018
Independent investigation into the death of Mr Prince Albert Wright, a prisoner at HMP Wymott, on 19 September 2018 © Crown copyright 2019 This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected]. Where we have identified any third-party copyright information you will need to obtain permission from the copyright holders concerned. The Prisons and Probation Ombudsman aims to make a significant contribution to safer, fairer custody and community supervision. One of the most important ways in which we work towards that aim is by carrying out independent investigations into deaths, due to any cause, of prisoners, young people in detention, residents of approved premises and detainees in immigration centres. My office carries out investigations to understand what happened and identify how the organisations whose actions we oversee can improve their work in the future. Mr Prince Albert Wright died on 19 September 2018 of throat cancer at a regional healthcare inpatient facility at HMP Preston. (He remained, technically, a prisoner of HMP Wymott, where he had been for three years before transferring to Preston.) Mr Wright was 84 years old. I offer my condolences to his family and friends. I am satisfied that Mr Wright received a good standard of care at Wymott and Preston and am pleased to see that there was a good multidisciplinary approach to his care.