Forecasting COVID-19-Associated Hospitalizations Under Different
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hidden Canals in Bologna
ro” comes from an old iron and copper beating works. In the Lock of Casalecchio di Reno - Photo Paolo Cortesi surrounding area there are many industrial archaeological fi nds: on the right bank of the canal: the remains of a rice husker and a brick kiln. And on the other the fi rst hydroelectric power station in Bologna, built in 1901. Finally, the Fornace Galotti brickworks, - novemre 2015 now restored and used as a museum. 10. Industrial Heritage Museum - Via della Beverara, 123 Built in 1887 by Celeste Ga- lotti, the brickworks with its a metropolitana bolognatipografi Hoff mann furnace was used until 1966. Th e Museum illustrates the economic history of the city and return to the river the gravel and sand that would reduce the and its surrounding area, riverbed if deposited. from the Modern to the During harsh winters, the surface spillway of Paraporto Scaletta, Contemporary Age. better known as “the ice house”, stopped sheets of fl oating ice An interesting section shows from being carried towards the city, where they could damage the how between the XV and wheels of the water mills and thus harm local industries. the XVIII centuries Bologna For further information: was a centre of silk produc- Museo del Patrimonio Industriale Consorzi dei Canali di Reno e Savena in Bologna tel. +39 051.6493527 tion, thanks to technological www.consorzireno-savena.it innovations and a system of production that used water power. Th e focal point of the section is a working model of a silk mill, scale 1:2, rebuilt to evoke the memory of this astonishing machine lost Stazione viale P. -

Masters Erasmus Mundus Coordonnés Par Ou Associant Un EESR Français
Les Masters conjoints « Erasmus Mundus » Masters conjoints « Erasmus Mundus » coordonnés par un établissement français ou associant au moins un établissement français Liste complète des Masters conjoints Erasmus Mundus : http://eacea.ec.europa.eu/erasmus_mundus/results_compendia/selected_projects_action_1_master_courses_en.php *Master n’offrant pas de bourses Erasmus Mundus *ACES - Joint Masters Degree in Aquaculture, Environment and Society (cursus en 2 ans) UK-University of the Highlands and Islands LBG FR- Université de Nantes GR- University of Crete http://www.sams.ac.uk/erasmus-master-aquaculture ADVANCES - MA Advanced Development in Social Work (cursus en 2 ans) UK-UNIVERSITY OF LINCOLN, United Kingdom DE-AALBORG UNIVERSITET - AALBORG UNIVERSITY FR-UNIVERSITÉ PARIS OUEST NANTERRE LA DÉFENSE PO-UNIWERSYTET WARSZAWSKI PT-UNIVERSIDADE TECNICA DE LISBOA www.socialworkadvances.org AMASE - Joint European Master Programme in Advanced Materials Science and Engineering (cursus en 2 ans) DE – Saarland University ES – Polytechnic University of Catalonia FR – Institut National Polytechnique de Lorraine SE – Lulea University of Technology http://www.amase-master.net ASC - Advanced Spectroscopy in Chemistry Master's Course FR – Université des Sciences et Technologies de Lille – Lille 1 DE - University Leipzig IT - Alma Mater Studiorum - University of Bologna PL - Jagiellonian University FI - University of Helsinki http://www.master-asc.org Août 2016 Page 1 ATOSIM - Atomic Scale Modelling of Physical, Chemical and Bio-molecular Systems (cursus -

CONICYT Ranking Por Disciplina > Sub-Área OECD (Académicas) Comisión Nacional De Investigación 1
CONICYT Ranking por Disciplina > Sub-área OECD (Académicas) Comisión Nacional de Investigación 1. Ciencias Naturales > 1.2 Computación y Ciencias de la Científica y Tecnológica Informática PAÍS INSTITUCIÓN RANKING PUNTAJE USA Carnegie Mellon University 1 5,000 CHINA Tsinghua University 2 5,000 USA University of California Berkeley 3 5,000 USA Massachusetts Institute of Technology (MIT) 4 5,000 Nanyang Technological University & National Institute of Education SINGAPORE 5 5,000 (NIE) Singapore USA Stanford University 6 5,000 SWITZERLAND ETH Zurich 7 5,000 HONG KONG Chinese University of Hong Kong 8 5,000 FRANCE Universite Paris Saclay (ComUE) 9 5,000 INDIA Indian Institute of Technology System (IIT System) 10 5,000 SINGAPORE National University of Singapore 11 5,000 USA University of Michigan 12 5,000 USA University of Illinois Urbana-Champaign 13 5,000 GERMANY Technical University of Munich 14 5,000 CHINA Harbin Institute of Technology 15 5,000 CHINA Shanghai Jiao Tong University 16 5,000 USA Georgia Institute of Technology 17 5,000 UNITED KINGDOM University of Oxford 18 5,000 UNITED KINGDOM Imperial College London 19 5,000 CHINA Peking University 20 5,000 USA University of Southern California 21 5,000 USA University of Maryland College Park 22 5,000 CHINA Zhejiang University 23 5,000 USA University of Texas Austin 24 5,000 USA University of Washington Seattle 25 5,000 CHINA Huazhong University of Science & Technology 26 5,000 USA University of California San Diego 27 5,000 USA University of North Carolina Chapel Hill 28 5,000 HONG KONG -
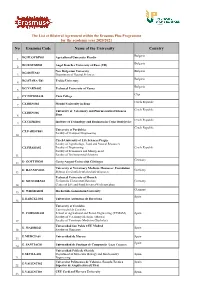
No Erasmus Code Name of the University Country
The List of Bilateral Agreement within the Erasmus Plus Programme for the academic year 2020/2021 No Erasmus Code Name of the University Country Bulgaria BG PLOVDIV01 Agricultural University Plovdiv 1. Bulgaria BG ROUSSE01 Angel Kanchev University of Ruse (UR) 2. New Bulgarian University Bulgaria BG SOFIA02 3. Department of Natural Sciences Bulgaria BG STARA-Z01 Trakia University 4. Bulgaria BG VARNA02 Technical University of Varna 5. Cypr CY NICOSIA36 Casa College 6. Czech Republic CZ BRNO02 Mendel University in Brno 7. University of Veterinary and Pharmaceutical Sciences Czech Republic CZ BRNO06 8. Brno Czech Republic CZ CESKE04 Institute of Technology and Businness in Ceske Budejovice 9. Czech Republic University of Pardubice CZ PARDUB01 Faculty of Transport Engineering 10. Czech University of Life Sciences Prague Faculty of Agrobiology, Food and Natural Resources CZ PRAHA02 Faculty of Engineering Czech Republic Faculty of Economics and Management 11. Faculty of Environmental Sciences Germany D GOTTING01 Georg-August-Universität Göttingen 12. University of Veterinary Medicine Hannover, Foundation D HANNOVE03 Germany 13. Stiftung Tierärztliche Hochschule Hannover Technical University of Munich D MUNCHEN02 Technische Universität Munchen Germany 14. Center of Life and Food SciencesWeihenstephan Germany 15. D WIESBAD04 Hochschule Geisenheim University Spain E BARCELO02 Universitat Autonoma de Barcelona 16. University of Cordoba Universidad de Cordoba E CORDOBA01 School of Agricultural and Forest Engineering (ETSIAM) Spain Faculty of Veterinary Medicine (Master) 17. Faculty of Veterinary Medicine (Bachelor) Universidad San Pablo CEU Madrid E MADRID21 Spain 18. Faculty of Pharmacy E MURCIA01 Universidad de Murcia Spain 19. Spain E SANTIAG01 Universidad de Santiago de Compostela (Lugo Campus) 20. -

The Bolognese Valleys of the Idice, Savena and Setta
3_ eo_gb 0 008 3: 0 ag a The Bolognese Valleys of the Idice, Savena and Setta 114 _ dce_gb 0 008 3: 9 ag a 5 The Rivers the Futa state highway SS 65 and the road The valleys of the tributaries to the right of along the valley-bottom, which continues as the Reno punctuate the central area of the far as the Lake of Castel dell’Alpi, passing the Bolognese Apennines in a truly surprising majestic Gorges of Scascoli. Along the river, variety of colours and landscapes. They are there are numerous mills, some of which can the Idice, Savena and Setta Rivers, of which be visited, constructed over the centuries. only the Idice continues its course onto the Before entering the plains, the Savena cros- plains, as far as the Park of the Po Delta. ses the Regional Park of Bolognese Gypsums and Abbadessa Gullies, which is also crossed The Idice by the River Idice. The Idice starts on Monte Oggioli, near the Raticosa Pass, and is the largest of the rivers in these valleys. Interesting from a geologi- cal and naturalistic point of view, its valley offers many reasons for a visit. Particularly beautiful is the stretch of river where it joins the Zena Valley: this is where the Canale dei Mulini (mills) branches off, continuing alon- gside it until it reaches the plains, in the ter- ritory of San Lazzaro di Savena. Flowing through the Valleys of Campotto, the Idice finally joins the Reno. Here an interesting system of manmade basins stop the Reno’s water flowing into the Idice’s bed in dry periods. -

Last Reviewed Palermo Trans.Making Week 24 28 February
Palermo trans•making week 24th February-28th February 2020 The trans-making project aims to establish a multilateral network of research and innovation staff active in the fields of placemaking/place-based art activities as a space to create alternative narratives for societal and economic renewal. It investigates and experiments with placemaking to contribute actively to the democratization/well-being of society, educating and empowering individuals and disadvantaged minorities through research and production in the connection between art and new technologies. Partners: BIS (TR), Bunker (SI), Citema (IT), Cluster Cairo (EG), Crvena (BA), El Taller TRES (CL), FTDES (TS), Istanbul Technical University (TR), Institute of Criminology (SI), Istituto Pedro Arrupe (IT), Izmir University of Economics (TR), Relais Culture Europe (FR), University College of London (UK), University of Havana (CU), University of Palermo (IT), University of Perugia (IT), University of Valencia (ES), Workshops of Culture (PL), Yunnan University (CH), ZRC-SAZU (SI). Enrollment by February 9th: Registration is required by filling the survey at the following link: https://docs.google.com/forms/d/e/1FAIpQLScaP PjDsFCKeStJh- Srf5nXYD_TSvtpYjeXiYSHj9N59xEFIw/viewform The «Palermo trans-making week» is proposed and animated by: This project has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Skłodowska-Curie grant agreement n°734855. #TRANS-MAPPING 24th & 25th February 2020 A workshop proposed by amberPlatform/BIS -
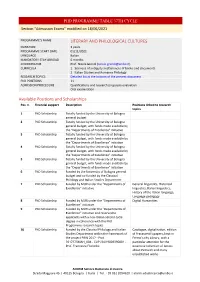
PHD PROGRAMME TABLE 37TH CYCLE Section “Admission Exams” Modified on 18/06/2021
PHD PROGRAMME TABLE 37TH CYCLE Section “Admission Exams” modified on 18/06/2021 PROGRAMME’S NAME LITERARY AND PHILOLOGICAL CULTURES DURATION 3 years PROGRAMME START DATE 01/11/2021 LANGUAGE Italian MANDATORY STAY ABROAD 6 months COORDINATOR Prof. Nicola Grandi ([email protected]) CURRICULA 1. Sciences of antiquity and Sciences of books and documents 2. Italian Studies and Romance Philology RESEARCH TOPICS Detailed list at the bottom of the present document PhD POSITIONS 11 ADMISSION PROCEDURE Qualifications and research proposals evaluation Oral examination Available Positions and Scholarships Pos. n. Financial support Description Positions linked to research topics 1 PhD Scholarship Totally funded by the University of Bologna general budget 2 PhD Scholarship Totally funded by the University of Bologna general budget, with funds made available by the "Departments of Excellence" initiative 3 PhD Scholarship Totally funded by the University of Bologna general budget, with funds made available by the "Departments of Excellence" initiative 4 PhD Scholarship Totally funded by the University of Bologna general budget, with funds made available by the "Departments of Excellence" initiative 5 PhD Scholarship Totally funded by the University of Bologna general budget, with funds made available by the "Departments of Excellence" initiative 6 PhD Scholarship Funded by the University of Bologna general budget and co-funded by the Classical Philology and Italian Studies Department 7 PhD Scholarship Funded by MUR under the "Departments of General -

S•H IOBC/WPRS Meeting- Florence, Italy, June 4-7, 2018
- IOBCjWPRS s•h IOBC/WPRS Meeting- Florence, Italy, June 4-7, 2018 Abstract book IOBC OILB WPRS/SROP 8th IOBC-WPRS meeting on “Integrated Protection of Olive Crops” Organising committee Prof. Patrizia Sacchetti Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Prof. Antonio Belcari Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Dr. Marzia Cristiana Rosi Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Dr. Bruno Bagnoli Department for Innovation in Biological, Agro-Food and Forestry Systems, Tuscia University, Viterbo, Italy Prof. Laura Mugnai Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Prof. Stefania Tegli Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Dr. Elisabetta Gargani Consiglio per la ricerca in agricoltura e l'analisi dell'economia agraria (Council for Agricultural Research and Economics, CREA), Centro Difesa e Certificazione (Research Centre for Plant Protection and Certification), Florence, Italy Dr. Claudio Cantini National Research Council, IVALSA Institute, Follonica, Grosseto, Italy v Scientific Committee Prof. Antonio Belcari Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Prof. Angelo Canale Department of Agricultural, Food and Agro-Environmental Sciences, University of Pisa Prof. José Alberto Cardoso Pereira Polytechnic Institute of Bragança, Department of Production and Plant Technology Bragança, Portugal Dr. Anna Maria D'Onghia CIHEAM-Mediterranean Agronomic Institute of Bari, Italy Prof. Riccardo Gucci Department of Agricultural, Food and Agro-Environmental Sciences, University of Pisa, Italy Prof. Kostas Mathiopoulos Department of Biochemistry and Biotechnology, University of Thessaly, Greece Prof. Laura Mugnai Department of Agrifood Production and Environmental Sciences, University of Florence, Italy Dr. -

FORMATO PDF Ranking Instituciones Acadã©Micas Por Sub áRea OCDE
Ranking Instituciones Académicas por sub área OCDE 2020 3. Ciencias Médicas y de la Salud > 3.01 Medicina Básica PAÍS INSTITUCIÓN RANKING PUNTAJE USA Harvard University 1 5,000 UNITED KINGDOM University College London 2 5,000 USA Johns Hopkins University 3 5,000 USA University of Pennsylvania 4 5,000 USA University of California San Francisco 5 5,000 CANADA University of Toronto 6 5,000 USA Stanford University 7 5,000 USA University of Washington Seattle 8 5,000 UNITED KINGDOM University of Oxford 9 5,000 USA University of Pittsburgh 10 5,000 USA University of California Los Angeles 11 5,000 USA Columbia University 12 5,000 USA University of California San Diego 13 5,000 UNITED KINGDOM Kings College London 14 5,000 SWEDEN Karolinska Institutet 15 5,000 USA Yale University 16 5,000 UNITED KINGDOM Imperial College London 17 5,000 USA University of North Carolina Chapel Hill 18 5,000 USA Icahn School of Medicine at Mount Sinai 19 5,000 USA Washington University (WUSTL) 20 5,000 USA University of Michigan 21 5,000 GERMANY Free University of Berlin 22 5,000 USA Duke University 23 5,000 AUSTRALIA University of Melbourne 24 5,000 USA Emory University 25 5,000 DENMARK University of Copenhagen 26 5,000 CANADA McGill University 27 5,000 FRANCE Sorbonne Universite 28 5,000 GERMANY Humboldt University of Berlin 29 5,000 USA Massachusetts Institute of Technology (MIT) 30 5,000 FRANCE Universite Sorbonne Paris Cite-USPC (ComUE) 31 5,000 NETHERLANDS University of Amsterdam 32 5,000 NETHERLANDS Utrecht University 33 5,000 GERMANY Charite Medical University -

BOLOGNA CAMPUS ACADEMIC YEAR 2019/2020 EXCHANGE Presentation
ALMA MATER STUDIORUM UNIVERSITÀ DI BOLOGNA STUDENTS GUIDE BOLOGNA CAMPUS ACADEMIC YEAR 2019/2020 EXCHANGE Presentation Exchange Students Guide Bologna Campus A.Y. 2019/2020 Welcome to the University of Bologna! This Guide also aims to introduce you to the city Produced by This Guide is for international exchange students and its beauty, helping you to discover the places, Alma Mater Studiorum - Università di Bologna at the Bologna Campus. To make the most of your the art, events, and people that will make your DIRI - International Relations Division experience at the university and to benefit of all experience unique. Exchange Students Desk the cultural and leisure opportunities offered by Editing and grapfhic design the city of Bologna and its students community Alma Mater Studiorum - Università di Bologna it is important to learn about the rules and the ARTEC - Industrial Relations, Third Mission and Communication Division procedures to be followed and to find out about the Insitutional Communication Office services offered by the university and its territory. www.unibo.it/exchangestudents Layout Alma Mater Studiorum - Università di Bologna ARTEC - Industrial Relations, Third Mission and Communication Division The origins of the University of Bologna go way back, University of Bologna is a Multicampus university with Insitutional Communication Office and it is considered to be the oldest university in the 5 campuses: Bologna, Cesena, Forlì, Ravenna and Printed by Western world. Its history began in 1088, when law Rimini, a school of excellence, the Collegio Superiore, ACM Spa was first taught freely in the city, and became tied and an Advanced Studies Centre in Buenos Aires. -
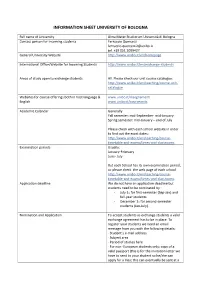
Information Sheet University of Bologna
INFORMATION SHEET UNIVERSITY OF BOLOGNA Full name of University Alma Mater Studiorum Università di Bologna Contact person for incoming students Ferruccio Quercetti [email protected] tel. +39 051 2099427 General University Website http://www.unibo.it/en/homepage International Office/Website for Incoming Students http://www.unibo.it/en/exchange-students Areas of study open to exchange students All. Please check our unit course catalogue: http://www.unibo.it/en/teaching/course-unit- catalogue Websites for course offerings both in host language & www.unibo.it/insegnamenti English www.unibo.it/courseunits Academic Calendar Generally Fall semester: mid-September- mid-January Spring semester: mid-January – end of July Please check with each school website in order to find out the exact dates: http://www.unibo.it/en/teaching/course- timetable-and-exams/times-and-classrooms Examination periods Usually: January-February June- July But each School has its own examination period, so please check the web page of each school. http://www.unibo.it/en/teaching/course- timetable-and-exams/times-and-classrooms Application deadline We do not have an application deadline but students need to be nominated by : - July 1st for first-semester (Sep-Jan) and full-year students. - December 1st for second-semester students (Jan-July). Nomination and Application To accept students as exchange students a valid exchange agreement has to be in place. To register your students we need an email message from you with the following details: · Student’s e-mail -

Curriculum Vitae ‐ Autumn 2014
Via Sarfatti 25 20136 Milano Curriculum Vitae ‐ Autumn 2014 Family name: Tagiuri Given name: Giacomo Gender: male Date of birth: (16/11/1986) Citizenship: Italian email address: [email protected] Qualifications Bocconi University Ph.D. in Legal Studies (September 2014 – 2017 expected) International Law and Economics • Full Scholarship Johns Hopkins University School of Advanced International Studies (Bologna and Washington, DC) Master of Arts in European Studies and International Economics (May 2013) • Fondazione del Monte Scholarship • Distinction in European Studies Università di Bologna Laurea Magistrale in Law (March 2011) • 110/110 magna cum laude • Erasmus Student at University of Copenhagen (January‐July 2008) Awards and Scholarships Fondazione del Monte Schoparship (Johns Hopkins University a.a. 2011/2012) Stavros Niarchos Summer Internship Funds (Johns Hopkins University, Summer 2013) University of Bologna scholarship for thesis preparation abroad (Sept.‐Dec. 2010) Bobby Abernethy Scholarship for Summer School “EU and legal reforms” (Igalo, Montenegro, Summer 2010) Research Interests International Law, Comparative Public Law, European Integration, Culture and Identity, Cultural Heritage and the Law. Publications – La dottrina Britannica in tema di diritti umani, Diritto Pubblico Comparato ed Europeo, 4/2014 – La dottrina britannica in tema di amministrazione, Diritto Pubblico Comparato ed Europeo, 1/2014. – Forging Identity: The EU and European Culture, Survival: Global Politics and Strategy, 1/2014. Article shortlisted for the International Institute of Strategic Studies (IISS)'s Palliser Essay Prize. – Letter from Italy, Survival:Global Politics and Strategy, 1/2013, pp. 197‐204. – G.Tagiuri, Romney's Italian Job, in IISS Voices, 05 November 2012 (Blog post on www.iiss.org/whats‐ new/iiss‐voices/) – Il referendum del 1975: quando i britannici decisero di rimanere nella Comunità economica europea (co‐authored with J.