Does Capitation Prepayment Based Integrated County Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Bank Document
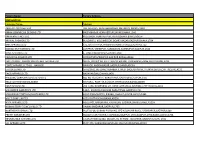
Project Name : Anhui Highway Maintenance Innovation and Demonstration Project Financed by the World Bank 、、、、、、、、、、、、、、、、、、、、、 Procurement Plan、、、、 Public Disclosure Authorized Date /、、、July 4, 2017/2017、7、4、 Thresholds for Procurement Method 、、、、、、 Description、、 Thresholds 、、 Works 、、/ S&I NCB、、、、、、、: <USD40,000,000.00 、、、、、、、 4000、、、、、、、、、、、、、、、、 Shopping、、、、: <USD500,000.00 、、、、、、、 50、、、、、、、、、、、、、 Goods 、、 NCB、、、、、、、、 <USD10,000,000.00 、、、、、、、 1000、、、、、、、、、、、、、、、、 Shopping、、、、: : <USD200,000.00、、、、、、、 20、、、、、、、、、、、、、 Consultant 、、 CQS、、、、、、、、、、、: <=USD300,000.00、、、、、、、 30、、、、、、、、、、、、、、、、、、、、 Public Disclosure Authorized Thresholds for Prior Review 、、、、 Description、、 Thresholds 、、 Works 、、/ S&I >=USD20,000,000.00; 、、、、、、、、、 2000、、、、、、、、、、、 Goods 、、 >=USD6,000,000.00; 、、、、、、、、、 600、、、、、、、、、、、 Consultant 、、 Firm being consultant、、、、: >=USD4,000,000.00; 、、、、、、、、、 400、、、、、、、、、、、、、、、、、、、、、 Individual being consultant、、、、:>=USD500,000.00、、、、、、、、、 50、、、、、、、、、、、、、、、、、、、、、 Public Disclosure Authorized Threshold for Shortlist Comprising Entirely national Consultants: <=USD500,000 or equivalent 、、、、、、、、、、、、、、、、、、、、、50、、、 Public Disclosure Authorized Project Name: Anhui Highway Maintenance Innovation and Demonstration Project Financed by the World Bank 、、、、: 、、、、、、、、、、、、、、、、 Procurement Plan 、、、、 Updated Date 、、、、、 2017.7.4 For Contracts For Contracts Not Signed Already Signed 、、、、、、、、、 、、、、、、、、、、 Cost Prior Contract Procurement Number Works/S&I/Goods/Consultants Estimate /Post Actual Remarks Number Contract Description 、、、、、、、、、、、、、、 Method Estimated -

A Miraculous Ningguo City of China and Analysis of Influencing Factors of Competitive Advantage
www.ccsenet.org/jgg Journal of Geography and Geology Vol. 3, No. 1; September 2011 A Miraculous Ningguo City of China and Analysis of Influencing Factors of Competitive Advantage Wei Shui Department of Eco-agriculture and Regional Development Sichuan Agricultural University, Chengdu Sichuan 611130, China & School of Geography and Planning Sun Yat-Sen University, Guangzhou 510275, China Tel: 86-158-2803-3646 E-mail: [email protected] Received: March 31, 2011 Accepted: April 14, 2011 doi:10.5539/jgg.v3n1p207 Abstract Ningguo City is a remote and small county in Anhui Province, China. It has created “Ningguo Miracle” since 1990s. Its general economic capacity has been ranked #1 (the first) among all the counties or cities in Anhui Province since 2000. In order to analyze the influencing factors of competitive advantages of Ningguo City and explain “Ningguo Miracle”, this article have evaluated, analyzed and classified the general economic competitiveness of 61 counties (cities) in Anhui Province in 2004, by 14 indexes of evaluation index system. The result showed that compared with other counties (cities) in Anhui Province, Ningguo City has more advantages in competition. The competitive advantage of Ningguo City is due to the productivities, the effect of the second industry and industry, and the investment of fixed assets. Then the influencing factors of Ningguo’s competitiveness in terms of productivity were analyzed with authoritative data since 1990 and a log linear regression model was established by stepwise regression method. The results demonstrated that the key influencing factor of Ningguo City’s competitive advantage was the change of industry structure, especially the change of manufacture structure. -

China's New Top Government Leaders
China’s new top government leaders China’s state leaders were revealed on March 18th, 2018 at the conclusion of the 13th National People’s Congress (NPC). Most notably, the NPC approved a constitutional change abolishing term limits for China’s president Xi Jinping. Below are background profiles for the seven top government leaders. Compiled by Cheng Li and the staff of the John L. Thornton China Center at Brookings 1 Xi Jinping 习近平 Born 1953 Current Positions • President of the People’s Republic of China (PRC) (2013–present) • General Secretary of the Chinese Communist Party (CCP) (2012– present) • Chairman of the Central Military Commission (CMC) (2012–present) • Member of the Politburo Standing Committee (PSC) (2007–present) • Chairman of the National Security Committee (2013–present) • Head of the Central Leading Group for Comprehensively Deepening Reforms (2013–present) • Head of the Central Leading Group for Foreign Affairs and National Security (2013–present) • Head of the Central Leading Group for Taiwan Affairs (2012–present) • Head of the Central Leading Group for Financial and Economic Work (2013–present) • Head of the Central Leading Group for Network Security and Information Technology (2014–present) • Head of the CMC Central Leading Group for Deepening Reforms of National Defense and the Military (2014–present) • Commander in Chief of the Joint Operations Command Center of the People’s Liberation Army (PLA) (2016–present) • Chairman of the Central Military and Civilian Integration Development Committee (2017– present) • Member of the Politburo (2007–present) • Full member of the Central Committee of the CCP (2002–present) Personal and Professional Background Xi Jinping was born on June 15, 1953, in Beijing. -

Annual Report 2019
HAITONG SECURITIES CO., LTD. 海通證券股份有限公司 Annual Report 2019 2019 年度報告 2019 年度報告 Annual Report CONTENTS Section I DEFINITIONS AND MATERIAL RISK WARNINGS 4 Section II COMPANY PROFILE AND KEY FINANCIAL INDICATORS 8 Section III SUMMARY OF THE COMPANY’S BUSINESS 25 Section IV REPORT OF THE BOARD OF DIRECTORS 33 Section V SIGNIFICANT EVENTS 85 Section VI CHANGES IN ORDINARY SHARES AND PARTICULARS ABOUT SHAREHOLDERS 123 Section VII PREFERENCE SHARES 134 Section VIII DIRECTORS, SUPERVISORS, SENIOR MANAGEMENT AND EMPLOYEES 135 Section IX CORPORATE GOVERNANCE 191 Section X CORPORATE BONDS 233 Section XI FINANCIAL REPORT 242 Section XII DOCUMENTS AVAILABLE FOR INSPECTION 243 Section XIII INFORMATION DISCLOSURES OF SECURITIES COMPANY 244 IMPORTANT NOTICE The Board, the Supervisory Committee, Directors, Supervisors and senior management of the Company warrant the truthfulness, accuracy and completeness of contents of this annual report (the “Report”) and that there is no false representation, misleading statement contained herein or material omission from this Report, for which they will assume joint and several liabilities. This Report was considered and approved at the seventh meeting of the seventh session of the Board. All the Directors of the Company attended the Board meeting. None of the Directors or Supervisors has made any objection to this Report. Deloitte Touche Tohmatsu (Deloitte Touche Tohmatsu and Deloitte Touche Tohmatsu Certified Public Accountants LLP (Special General Partnership)) have audited the annual financial reports of the Company prepared in accordance with PRC GAAP and IFRS respectively, and issued a standard and unqualified audit report of the Company. All financial data in this Report are denominated in RMB unless otherwise indicated. -

World Bank Document
E1114 v 8 Public Disclosure Authorized WORLD BANK FUNDED CHINA IRRIGATED AGRICULTURE INTENSIFICATION III PROJECT DAM SAFETY REPORT Public Disclosure Authorized Public Disclosure Authorized PREPARED BY STATE OFFICE OF COMPREHENSIVE AGRICULTURAL DEVELOPMENT JANUARY 2005 Public Disclosure Authorized Table of Contents 1. Description of the dams in the project areas 2. Main problems of the 4 dangerous dams and the remedy arrangement 3. Operation of the safe dams and conclusions from their safety inspection 4. Safety control of the dams 5. Summary of the major specifications of the dams 6. Monitoring and reporting systems on dam safety 1. Description of the dams in the project areas There exist 17 dams higher than 15 meters in the 5 project provinces, which supply irrigation water to the project areas. Of which the large sized dams with a water storage capacity each of more than 100 million cubic meters account for 10 and the others are medium sized dams with a water storage capacity ranging from 10 million to 100 million cubic meters each. The 17 dams are allocated as 8 in Anhui Province, 4 in Henan Province, 3 in Shandong Province and 2 in Jiangsu Province. The 5 provincial authorities involved in the project have conducted overall inspection and safety appraisal on the 17 dams in line with the Bank’s operational handbook of “Dam Safety” (OP 4.37) and the “Rule on Appraisal of the Dam Safety” issued by the Ministry of Water Resources in 1995. The inspection mainly covers the safety situation of the dams and their installed structures such as the gates and spillways. -

ANHUI EXPRESSWAY COMPANY LIMITED App.1A.1 (A Joint Stock Limited Company Incorporated in the People’S Republic of China with Limited Liability) App.1A 5
IMPORTANT If you are in any doubt about this prospectus, you should consult your stockbroker, bank manager, solicitor, professional accountant or other professional S38(1A) adviser. A copy of this prospectus, having attached thereto the documents specified in the section headed “Documents delivered to the Registrar of Companies in Hong Kong” in appendix X, has been registered by the Registrar of Companies in Hong Kong as required by section 342C of the Companies Ordinance of Hong S342C Kong. The Registrar of Companies in Hong Kong takes no responsibility for the contents of this prospectus or any of the documents referred to above. The Stock Exchange of Hong Kong Limited (the “Stock Exchange”) and Hong Kong Securities Clearing Company Limited (“Hongkong Clearing”) take no responsibility for the contents of this prospectus, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this prospectus. ANHUI EXPRESSWAY COMPANY LIMITED App.1A.1 (a joint stock limited company incorporated in the People’s Republic of China with limited liability) App.1A 5 Placing and New Issue of 493,010,000 H Shares of nominal value RMB1.00 each, App.1A at an issue price of RMB1.89 per H Share 15(2)(a)(c)(d) payableinfullonapplication 3rd Sch at HK$1.77 per H Share App.1Apara 9 15(2)(h) Sponsors and Lead Underwriters CEF Capital Limited The CEF Group Crosby Capital Markets (Asia) Limited Co-Underwriters DBS Asia Capital Limited Peregrine Capital Limited J&A Securities (Hong Kong) Limited Shanghai International Capital (H.K.) Limited Wheelock NatWest Securities Limited Seapower Securities Limited Amsteel Securities (H.K.) Limited China Southern Corporate Finance Ltd. -

Li Keqiang 李克强 Born 1955
Li Keqiang 李克强 Born 1955 Current Positions • Premier of the State Council (2013–present) • Member of the Politburo Standing Committee (2007–present) • Vice-Chairman of the National Security Committee (2013–present) • Deputy Head of the Central Leading Group for Comprehensively Deepening Reforms (2013–present) • Deputy Head of the Central Leading Group for Financial and Economic Work (2013–present) • Vice-Chairman of the Central Military and Civilian Integration Development Committee (2017– present) • Chairman of the Committee on Organizational Structure of the Central Committee of the CCP (2012–present) • Chairman of the National Defense Mobilization Committee (2013–present) • Director of the State Energy Commission (2013–present) • Head of the National Leading Group for Climate Change and for Energy Conservation and Reduction of Pollution Discharge (2013–present) • Head of the State Council Leading Group for Rejuvenating the Northeast Region and Other Old Industrial Bases (2013–present) • Head of the State Council Leading Group for Western Regional Development (2013–present) • Head of the State Council Three Gorges Project Construction Committee (2008–present) • Head of the State Council South-to-North Water Diversion Project Construction Committee (2008– present) • Head of the State Council Leading Group for Deepening Medical and Health System Reform (2008– present) • Member of the Politburo (2007–present) • Full member of the Central Committee of the CCP (1997–present) Personal and Professional Background Li Keqiang was born on July 1, 1955, in Dingyuan County, Anhui Province. Li joined the CCP in 1976. He was a “sent-down youth” at an agricultural commune in Fengyang County, Anhui (1974–76).1 He served as party secretary of a production brigade in the county (1976–78). -

Levi Strauss & Co. Factory List
Levi Strauss & Co. Factory List Published : November 2019 Total Number of LS&Co. Parent Company Name Employees Country Factory name Alternative Name Address City State Product Type (TOE) Initiatives (Licensee factories are (Workers, Staff, (WWB) blank) Contract Staff) Argentina Accecuer SA Juan Zanella 4656 Caseros Accessories <1000 Capital Argentina Best Sox S.A. Charlone 1446 Federal Apparel <1000 Argentina Estex Argentina S.R.L. Superi, 3530 Caba Apparel <1000 Argentina Gitti SRL Italia 4043 Mar del Plata Apparel <1000 Argentina Manufactura Arrecifes S.A. Ruta Nacional 8, Kilometro 178 Arrecifes Apparel <1000 Argentina Procesadora Serviconf SRL Gobernardor Ramon Castro 4765 Vicente Lopez Apparel <1000 Capital Argentina Spring S.R.L. Darwin, 173 Federal Apparel <1000 Asamblea (101) #536, Villa Lynch Argentina TEXINTER S.A. Texinter S.A. B1672AIB, Buenos Aires Buenos Aires <1000 Argentina Underwear M&S, S.R.L Levalle 449 Avellaneda Apparel <1000 Argentina Vira Offis S.A. Virasoro, 3570 Rosario Apparel <1000 Plot # 246-249, Shiddirgonj, Bangladesh Ananta Apparels Ltd. Nazmul Hoque Narayangonj-1431 Narayangonj Apparel 1000-5000 WWB Ananta KASHPARA, NOYABARI, Bangladesh Ananta Denim Technology Ltd. Mr. Zakaria Habib Tanzil KANCHPUR Narayanganj Apparel 1000-5000 WWB Ananta Ayesha Clothing Company Ltd (Ayesha Bangobandhu Road, Tongabari, Clothing Company Ltd,Hamza Trims Ltd, Gazirchat Alia Madrasha, Ashulia, Bangladesh Hamza Clothing Ltd) Ayesha Clothing Company Ltd( Dhaka Dhaka Apparel 1000-5000 Jamgora, Post Office : Gazirchat Ayesha Clothing Company Ltd (Ayesha Ayesha Clothing Company Ltd(Unit-1)d Alia Madrasha, P.S : Savar, Bangladesh Washing Ltd.) (Ayesha Washing Ltd) Dhaka Dhaka Apparel 1000-5000 Khejur Bagan, Bara Ashulia, Bangladesh Cosmopolitan Industries PVT Ltd CIPL Savar Dhaka Apparel 1000-5000 WWB Epic Designers Ltd 1612, South Salna, Salna Bazar, Bangladesh Cutting Edge Industries Ltd. -

Anhui Expressway Company Limited (A Joint Stock Company Incorporated in the People's Republic of China with Limited Liability) (Stock Code: 0995)
Anhui Expressway Company Limited (A joint stock company incorporated in the People's Republic of China with limited liability) (Stock Code: 0995) Annual Report 2019 CONTENTS Important Notice 2 Section I Definitions 4 Section II Corporate Profile and Main Financial Indicators 6 Section III Corporate Business Summary 14 Section IV Report of the Board of Directors 19 Section V Major Events 49 Section VI Change of Ordinary Shares and Shareholders 82 Section VII Directors, Supervisors, Senior Management and Staff 91 Section VIII Corporate Governance Structure and Governance 106 Report Section IX Environmental, Social and Governance Report 134 Section X Report of the Supervisory Committee 179 Section XI Independent Auditor’s Report and Consolidated 181 Financial Statements Section XII Documents Available for Inspection 286 Appendix 292 ——Information Disclosure Index 287 ——Profile of the Highways 292 ——Toll Rates for Expressways 295 ——Toll Rates for Standard Highways 297 ——National Trunk Highways 299 ——The Map of the Highway Network of Anhui Province 300 Important Notice 1. The Board of the Directors, the Supervisory Committee and the Directors, Supervisors and the Senior Management of the Company hereby warrant that the contents of the annual report are true, accurate and complete, and that there are no false accounts, misleading statements or significant omissions of information and jointly and severally accept the legal responsibility. 2. All the Directors of the Company attend the Board meeting. 3. PricewaterhouseCoopers Zhong Tian LLP (PRC Auditor) and PricewaterhouseCoopers (Hong Kong Auditor) have issued standard unqualified audit opinions on the consolidated financial statements of the Company. 4. Mr. Xiang Xiaolong, the Chairman, Mr. -

Energy Markets in China and the Outlook for CMM Project
U.S. EP.NSII Coalbed Methane Energy Markets in China and the Outlook for CMM Project Development in Anhui, Chongqing, Henan, Inner Mongolia, and Guizhou Provinces Energy Markets in China and the Outlook for CMM Project Development in Anhui, Chongqing, Henan, Inner Mongolia, and Guizhou Provinces Revised, April 2015 Acknowledgements This publication was developed at the request of the U.S. Environmental Protection Agency (USEPA), in support of the Global Methane Initiative (GMI). In collaboration with the Coalbed Methane Outreach Program (CMOP), Raven Ridge Resources, Incorporated team members Candice Tellio, Charlee A. Boger, Raymond C. Pilcher, Martin Weil and James S. Marshall authored this report based on feasibility studies performed by Raven Ridge Resources, Incorporated, Advanced Resources International, and Eastern Research Group. 2 Disclaimer This report was prepared for the U.S. Environmental Protection Agency (USEPA). This analysis uses publicly available information in combination with information obtained through direct contact with mine personnel, equipment vendors, and project developers. USEPA does not: (a) make any warranty or representation, expressed or implied, with respect to the accuracy, completeness, or usefulness of the information contained in this report, or that the use of any apparatus, method, or process disclosed in this report may not infringe upon privately owned rights; (b) assume any liability with respect to the use of, or damages resulting from the use of, any information, apparatus, method, or process -
Factory Name
Factory Name Factory Address BANGLADESH Company Name Address AKH ECO APPARELS LTD 495, BALITHA, SHAH BELISHWER, DHAMRAI, DHAKA-1800 AMAN GRAPHICS & DESIGNS LTD NAZIMNAGAR HEMAYETPUR,SAVAR,DHAKA,1340 AMAN KNITTINGS LTD KULASHUR, HEMAYETPUR,SAVAR,DHAKA,BANGLADESH ARRIVAL FASHION LTD BUILDING 1, KOLOMESSOR, BOARD BAZAR,GAZIPUR,DHAKA,1704 BHIS APPARELS LTD 671, DATTA PARA, HOSSAIN MARKET,TONGI,GAZIPUR,1712 BONIAN KNIT FASHION LTD LATIFPUR, SHREEPUR, SARDAGONI,KASHIMPUR,GAZIPUR,1346 BOVS APPARELS LTD BORKAN,1, JAMUR MONIPURMUCHIPARA,DHAKA,1340 HOTAPARA, MIRZAPUR UNION, PS : CASSIOPEA FASHION LTD JOYDEVPUR,MIRZAPUR,GAZIPUR,BANGLADESH CHITTAGONG FASHION SPECIALISED TEXTILES LTD NO 26, ROAD # 04, CHITTAGONG EXPORT PROCESSING ZONE,CHITTAGONG,4223 CORTZ APPARELS LTD (1) - NAWJOR NAWJOR, KADDA BAZAR,GAZIPUR,BANGLADESH ETTADE JEANS LTD A-127-131,135-138,142-145,B-501-503,1670/2091, BUILDING NUMBER 3, WEST BSCIC SHOLASHAHAR, HOSIERY IND. ATURAR ESTATE, DEPOT,CHITTAGONG,4211 SHASAN,FATULLAH, FAKIR APPARELS LTD NARAYANGANJ,DHAKA,1400 HAESONG CORPORATION LTD. UNIT-2 NO, NO HIZAL HATI, BAROI PARA, KALIAKOIR,GAZIPUR,1705 HELA CLOTHING BANGLADESH SECTOR:1, PLOT: 53,54,66,67,CHITTAGONG,BANGLADESH KDS FASHION LTD 253 / 254, NASIRABAD I/A, AMIN JUTE MILLS, BAYEZID, CHITTAGONG,4211 MAJUMDER GARMENTS LTD. 113/1, MUDAFA PASCHIM PARA,TONGI,GAZIPUR,1711 MILLENNIUM TEXTILES (SOUTHERN) LTD PLOTBARA #RANGAMATIA, 29-32, SECTOR ZIRABO, # 3, EXPORT ASHULIA,SAVAR,DHAKA,1341 PROCESSING ZONE, CHITTAGONG- MULTI SHAF LIMITED 4223,CHITTAGONG,BANGLADESH NAFA APPARELS LTD HIJOLHATI, -

Change Pattern and Driving Mechanism of Construction Land In
EARTH SCIENCES RESEARCH JOURNAL LAND USE Earth Sci. Res. J. Vol. 24, No. 2 (June, 2020): 215-223 Change pattern and driving mechanism of construction land in China’s undertaking industrial transfer demonstration area: Taking the Wanjiang City Belt along the Yangtze River as an Example Yuhong Cao1*, Meiyun Liu1, Yuandan Cao1, Chen Chen1, Dapeng Zhang2 1School of Environmental Science and Engineering, Anhui Normal University, Wuhu 241002, China 2School of Geography and Tourism, Anhui Normal University, Wuhu 241002, China * Corresponding author: [email protected] ABSTRACT Keywords: expansion intensity; land use; hotspot The construction land includes urban land, rural residential areas, and other construction lands. The Wanjiang City Belt analysis; the Wanjiang City Belt along the along the Yangtze River is a vital demonstration area for undertaking industrial transfer in China. With the accumulation Yangtze River. of factors relative to economic development, the construction land has increased sharply, and the regional ecological security pattern is facing new challenges. After collecting the image interpretation data of multi-period land use of the Wanjiang City Belt, this work studies the characteristics of construction land change patterns since 1995. The driving mechanism was also analyzed based on the GIS platform, land use transfer matrix, expansion intensity index, hotspot analysis, and mathematical statistics. The results showed that: (1) From 1995 to 2015, the urban land and other construction lands in the Wanjiang City Belt have increased, but the rural residential areas decreased in 2010- 2015. The three types of lands had the most significant changes in 2005-2010, and the other construction land was particularly prominent.