Zolpidem and Driving Impairment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ON ATTRACTION of SLIME MOULD PHYSARUM POLYCEPHALUM to PLANTS with SEDATIVE PROPERTIES 1. Introduction Physarum Polycephalum Belo
ON ATTRACTION OF SLIME MOULD PHYSARUM POLYCEPHALUM TO PLANTS WITH SEDATIVE PROPERTIES ANDREW ADAMATZKY Abstract. A plasmodium of acellular slime mould Physarum polycephalum is a large single cell with many nuclei. Presented to a configuration of attracting and repelling stimuli a plasmodium optimizes its growth pattern and spans the attractants, while avoiding repellents, with efficient network of protoplasmic tubes. Such behaviour is interpreted as computation and the plasmodium as an amorphous growing biologi- cal computer. Till recently laboratory prototypes of slime mould computing devices (Physarum machines) employed rolled oats and oat powder to represent input data. We explore alternative sources of chemo-attractants, which do not require a sophis- ticated laboratory synthesis. We show that plasmodium of P. polycephalum prefers sedative herbal tablets and dried plants to oat flakes and honey. In laboratory experi- ments we develop a hierarchy of slime-moulds chemo-tactic preferences. We show that Valerian root (Valeriana officinalis) is strongest chemo-attractant of P. polycephalum outperforming not only most common plants with sedative activities but also some herbal tablets. Keywords: Physarum polycephalum, slime mould, valerian, passion flower, hops, ver- vain, gentian, wild lettuce, chemo-attraction 1. Introduction Physarum polycephalum belongs to the species of order Physarales, subclass Myxo- gastromycetidae, class Myxomycetes, division Myxostelida. It is commonly known as a true, acellular or multi-headed slime mould. Plasmodium is a `vegetative' phase, single cell with a myriad of diploid nuclei. The plasmodium looks like an amorphous yellowish mass with networks of protoplasmic tubes. The plasmodium behaves and moves as a giant amoeba. It feeds on bacteria, spores and other microbial creatures and micro- particles (Stephenson & Stempen, 2000). -

Yerevan State Medical University After M. Heratsi
YEREVAN STATE MEDICAL UNIVERSITY AFTER M. HERATSI DEPARTMENT OF PHARMACY Balasanyan M.G. Zhamharyan A.G. Afrikyan Sh. G. Khachaturyan M.S. Manjikyan A.P. MEDICINAL CHEMISTRY HANDOUT for the 3-rd-year pharmacy students (part 2) YEREVAN 2017 Analgesic Agents Agents that decrease pain are referred to as analgesics or as analgesics. Pain relieving agents are also called antinociceptives. An analgesic may be defined as a drug bringing about insensibility to pain without loss of consciousness. Pain has been classified into the following types: physiological, inflammatory, and neuropathic. Clearly, these all require different approaches to pain management. The three major classes of drugs used to manage pain are opioids, nonsteroidal anti-inflammatory agents, and non opioids with the central analgetic activity. Narcotic analgetics The prototype of opioids is Morphine. Morphine is obtained from opium, which is the partly dried latex from incised unripe capsules of Papaver somniferum. The opium contains a complex mixture of over 20 alkaloids. Two basic types of structures are recognized among the opium alkaloids, the phenanthrene (morphine) type and the benzylisoquinoline (papaverine) type (see structures), of which morphine, codeine, noscapine (narcotine), and papaverine are therapeutically the most important. The principle alkaloid in the mixture, and the one responsible for analgesic activity, is morphine. Morphine is an extremely complex molecule. In view of establish the structure a complicated molecule was to degrade the: compound into simpler molecules that were already known and could be identified. For example, the degradation of morphine with strong base produced methylamine, which established that there was an N-CH3 fragment in the molecule. -

Chronic Use of Opioid Medications Before and After Bariatric Surgery
Supplementary Online Content Raebel MA, Newcomer SR, Reifler LM, et al. Chronic use of opioid medications before and after bariatric surgery. JAMA. doi:10.1001/jama.2013.278344 eFigure. Opioid Dispensings in 60 Days Before and 60 Days After Bariatric Surgery eTable 1. Opioid Classification and Morphine Equivalents Conversion Factors for Opioids Administered by Tablet, Capsule, Liquid, Transdermal Patch, and Transmucosal Formulations eTable 2. ICD-9 Codes for Comorbid Diagnosis of Substance Abuse, Anxiety, Posttraumatic Stress Disorder, and/or Depression eTable 3. ICD-9 Codes for Inclusion and Exclusion of Chronic Pain Diagnoses eTable 4. Therapeutic Classes, Generic Names, and Selected Brand Names of Covariate Medications eTable 5. Types of Opioids Dispensed During the Year Before and the Year After Bariatric Surgery Among Presurgery Chronic Opioid Users eTable 6. Types of Opioids Used Before and After Bariatric Surgery Among 933 Individuals With Chronic Opioid Use Before Bariatric Surgery eTable 7. Unadjusted Characteristics of Chronic Opioid Users According to Whether or Not Both Presurgery and Postsurgery Body Mass Indexes (BMIs) Data Were Available eTable 8. Presurgery and Postsurgery Use of Opioids and Selected Other Analgesic and Adjunctive Pain Medication Classes Among Presurgery Chronic Opioid Users With Presurgery Chronic Pain Diagnoses This supplementary material has been provided by the authors to give readers additional information about their work. © 2013 American Medical Association. All rights reserved. Downloaded From: -

BUTALBITAL ANALGESICS Allzital (Butalbital-Acetaminophen
BUTALBITAL ANALGESICS Allzital (butalbital-acetaminophen), butalbital-aspirin-caffeine, butalbital-aspirin-caffeine- codeine, butalbital-acetaminophen, butalbital-acetaminophen-caffeine, butalbital- acetaminophen-caffeine-codeine, Vanatol LQ (butalbital-acetaminophen-caffeine liquid oral solution) RATIONALE FOR INCLUSION IN PA PROGRAM Background Butalbital containing products are non-opioid analgesics that contain a combination of different drug products indicated for the relief of the symptom complex of tension (or muscle contraction) headache pain. Butalbital is a short to intermediate-acting barbiturate that works in concert with acetaminophen, an antipyretic non-salicylate agent, aspirin, a pain-relieving NSAID, and caffeine, a stimulant that works in the CNS, to decrease pain via a mechanism that isn’t well understood. Butalbital is a habit-forming drug that potentiates the effects of other commonly abuse drugs or substances like alcohol. Caffeine might help increase vasodilation and smooth muscle relaxation, while butalbital is thought to help balance the CNS stimulation caused by caffeine and produces depressant effects (1). Regulatory Status FDA approved indication: Butalbital containing products are used in the relief of the symptom complex of tension or muscle contraction headaches (2-8). Frequent use of acute medications is generally thought to cause medication-overuse headache. To decrease the risk of medication-overuse headache (“rebound headache” or “drug-induced headache”) many experts limit acute therapy to two headache days per week on a regular basis. Based on concerns of overuse, medication-overuse headache, and withdrawal, the use of butalbital-containing analgesics should be limited and carefully monitored. The Allzital limit is set to the maximum of 12 doses per day for acute treatment of 8 headaches per month as this product contains less butalbital than other products. -

Receives Fda Approval for the Treatment of Insomnia
AMBIEN CR™ (ZOLPIDEM TARTRATE EXTENDED-RELEASE TABLETS) CIV RECEIVES FDA APPROVAL FOR THE TREATMENT OF INSOMNIA First and Only Extended-Release Prescription Sleep Medication Indicated for Sleep Induction and Maintenance Covers Broad Insomnia Population Paris, France, September 6, 2005 - Sanofi-aventis (EURONEXT: SAN and NYSE: SNY) announced today that the U.S. Food and Drug Administration (FDA) has approved AMBIEN CR™ (zolpidem tartrate extended-release tablets) CIV, a new extended-release formulation of the number ® one prescription sleep aid, AMBIEN (zolpidem tartrate) CIV, for the treatment of insomnia. AMBIEN CR is non-narcotic and a non-benzodiazepine, formulated to offer a similar safety profile to AMBIEN with a new indication for sleep maintenance, in addition to sleep induction. AMBIEN CR is the first and only extended-release prescription sleep medication to help people with insomnia fall asleep fast and maintain sleep with no significant decrease in next day performance. AMBIEN CR, a bi-layered tablet, is delivered in two stages. The first layer dissolves quickly to induce sleep. The second layer is released more gradually into the body to help provide more continuous sleep. “Insomnia is a significant public health problem, affecting millions of Americans. Insomnia impacts daily activities and is associated with increased health care costs,” said James K. Walsh, PhD, Executive Director and Senior Scientist, Sleep Medicine and Research Center at St. Luke's Hospital in St. Louis, Missouri. “Helping patients stay asleep is recognized as being as important as helping them fall asleep,” said Walsh. “Ambien CR has shown evidence of promoting sleep onset and more continuous sleep". -

Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules
Medication Guide Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules, C III Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules are: • A strong prescription pain medicine that contains an opioid (narcotic) that is indicated for the relief of the symptom complex of tension (or muscle contraction) headache, when other pain treatments such as non-opioid pain medicines do not treat your pain well enough or you cannot tolerate them. • An opioid pain medicine that can put you at risk for overdose and death. Even if you take your dose correctly as prescribed you are at risk for opioid addiction, abuse, and misuse that can lead to death. Important information about Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules: • Get emergency help right away if you take too much Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules (overdose). When you first start taking Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules, when your dose is changed, or if you take too much (overdose), serious or life-threatening breathing problems that can lead to death may occur. • Taking Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules with other opioid medicines, benzodiazepines, alcohol, or other central nervous system depressants (including street drugs) can cause severe drowsiness, decreased awareness, breathing problems, coma, and death. • Never give anyone else your Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules. They could die from taking it. Store Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules away from children and in a safe place to prevent stealing or abuse. Selling or giving away Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate Capsules is against the law. • Get emergency help right away if you take more than 4,000 mg of acetaminophen in 1 day. -

Herbal Remedies and Their Possible Effect on the Gabaergic System and Sleep
nutrients Review Herbal Remedies and Their Possible Effect on the GABAergic System and Sleep Oliviero Bruni 1,* , Luigi Ferini-Strambi 2,3, Elena Giacomoni 4 and Paolo Pellegrino 4 1 Department of Developmental and Social Psychology, Sapienza University, 00185 Rome, Italy 2 Department of Neurology, Ospedale San Raffaele Turro, 20127 Milan, Italy; [email protected] 3 Sleep Disorders Center, Vita-Salute San Raffaele University, 20132 Milan, Italy 4 Department of Medical Affairs, Sanofi Consumer HealthCare, 20158 Milan, Italy; Elena.Giacomoni@sanofi.com (E.G.); Paolo.Pellegrino@sanofi.com (P.P.) * Correspondence: [email protected]; Tel.: +39-33-5607-8964; Fax: +39-06-3377-5941 Abstract: Sleep is an essential component of physical and emotional well-being, and lack, or dis- ruption, of sleep due to insomnia is a highly prevalent problem. The interest in complementary and alternative medicines for treating or preventing insomnia has increased recently. Centuries-old herbal treatments, popular for their safety and effectiveness, include valerian, passionflower, lemon balm, lavender, and Californian poppy. These herbal medicines have been shown to reduce sleep latency and increase subjective and objective measures of sleep quality. Research into their molecular components revealed that their sedative and sleep-promoting properties rely on interactions with various neurotransmitter systems in the brain. Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter that plays a major role in controlling different vigilance states. GABA receptors are the targets of many pharmacological treatments for insomnia, such as benzodiazepines. Here, we perform a systematic analysis of studies assessing the mechanisms of action of various herbal medicines on different subtypes of GABA receptors in the context of sleep control. -
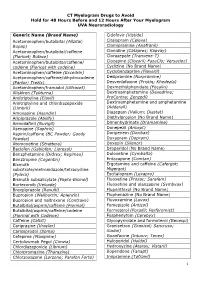
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -

Drug Plasma Half-Life and Urine Detection Window | January 2019
500 Chipeta Way | Salt Lake City, UT 84108-1221 Phone: (800) 522-2787 | Fax: (801) 583-2712 www.aruplab.com | www.arupconsult.com DRUG PLASMA HALF-LIFE AND URINE DETECTION WINDOW | JANUARY 2019 URINE- PLASMA DRUG, DRUG METABOLITE(S)* COMMON TRADE AND STREET NAMES, NOTES DETECTION HALF-LIFEt WINDOWt STIMULANTS Benzedrine, dexedrine, Adderall, Vyvanse, speed; could be methamphetamine Amphetamine 7–34 hours 1–5 days metabolite; if so, typically < 30 percent of parent Cocaine Coke, crack; parent drug rarely observed due to short half-life 0.7–1.5 hours < 1 day Benzoylecgonine Cocaine metabolite 5.5–7.5 hours 1–2 days Desoxyn, methedrine, Vicks inhaler (D- and L-isomers not resolved; low concentrations Methamphetamine expected if the source is Vicks); selegeline (Atapryl, Carbex, Eldepryl, Zelapar) 6–17 hours 1–5 days metabolite Methylenedioxyamphetamine (MDA) MDA 11–17 hours 1–3 days Methylenedioxyethylamphetamine (MDEA) MDEA, MDE, Eve 6–11 hours 1–3 days Methylenedioxymethamphetamine (MDMA) MDMA, XTC, ecstasy, Molly 6–10 hours 1–3 days Methylphenidate Ritalin, Concerta, Focalin, Metadate, Methylin 1.4–4.2 hours < 1 day Ritalinic acid Methylphenidate metabolite 1.8–2.5 hours < 1 day Phentermine Adipex-P, Lomaira, Qsymia 19–24 hours 1–5 days OPIOIDS Buprenorphine Belbuca, Buprenex, Butrans, Suboxone, Subutex, Sublocade, Zubsolv 26–42 hours 1–7 days Norbuprenorphine, Glucuronides Buprenorphine metabolites 15–150 hours 1–14 days Included in many preparations; morphine metabolite; may be a contaminant if < 2 Codeine 1.9–3.9 hours 1–3 days percent of morphine Fentanyl Actiq, Duragesic, Fentora, Lazanda, Sublimaze, Subsys, Ionsys 3–12 hours 1–3 days Norfentanyl Fentanyl metabolite 9–10 hours 1–3 days Heroin Diacetylmorphine, dope, smack, dust; parent drug not detected. -

Insomnia in the Elderly: Update on Assessment and Management
To see other CME articles, go to: www.cmegeriatrics.ca www.geriatricsjournal.ca If you are interested in receiving this publication on a regular basis, please consider becoming a member. INSOMNIA IN THE ELDERLY: UPDATE ON ASSESSMENT AND MANAGEMENT Canadian Geriatrics Society Abstract Insomnia disorder is one of the most common sleep-wake disorders seen Soojin Chun in the geriatric population, and is associated with multiple psychiatric MSc., MD FRCP(C) and medical consequences. Insomnia is a subjective complaint of Geriatric Psychiatry difficulty falling and/or staying asleep, or experiencing non-restorative Subspecialty Resident sleep, associated with significant daytime consequences including (PGY-6), University of difficulty concentrating, fatigue and mood disturbances. There is no Ottawa single diagnostic tool to assess insomnia. Consequently, an insomnia assessment requires thorough history taking including a sleep inquiry, Elliott Kyung Lee medical history, psychiatric history, substance use history and a relevant MD, FRCP(C), D. ABPN physical examination. Insomnia is often multifactorial in origin, and Sleep Med, Addiction routinely is associated with multiple other psychiatric and medical Psych, D. ABSM, F. AASM, disorders. Therefore, predisposing, precipitating and perpetuating factors F. APA, Sleep Specialist, must be carefully examined in the context of an evaluation of insomnia Royal Ottawa Mental symptoms. Other specific sleep assessments (e.g., overnight Health Centre, Assistant polysomnography) can be completed to rule out other sleep-wake Professor, University of disorders. For management, a cognitive-behavioural approach (including Ottawa sleep restriction therapy, stimulus control therapy) is commonly accepted as an effective, first-line treatment for insomnia disorder. Corresponding Author: A brief version of CBT-I focusing on behavioural interventions (Brief Elliott Kyung Lee Behavioural Treatment of Insomnia, BBT-I) has also demonstrated efficacy in the geriatric patient population. -

CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (Also Belong to Psychiatric Medication Category) • Codeine (In 222® Tablets, Tylenol® No
CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (also belong to psychiatric medication category) • codeine (in 222® Tablets, Tylenol® No. 1/2/3/4, Fiorinal® C, Benzodiazepines Codeine Contin, etc.) • heroin • alprazolam (Xanax®) • hydrocodone (Hycodan®, etc.) • chlordiazepoxide (Librium®) • hydromorphone (Dilaudid®) • clonazepam (Rivotril®) • methadone • diazepam (Valium®) • morphine (MS Contin®, M-Eslon®, Kadian®, Statex®, etc.) • flurazepam (Dalmane®) • oxycodone (in Oxycocet®, Percocet®, Percodan®, OxyContin®, etc.) • lorazepam (Ativan®) • pentazocine (Talwin®) • nitrazepam (Mogadon®) • oxazepam ( Serax®) Alcohol • temazepam (Restoril®) Inhalants Barbiturates • gases (e.g. nitrous oxide, “laughing gas”, chloroform, halothane, • butalbital (in Fiorinal®) ether) • secobarbital (Seconal®) • volatile solvents (benzene, toluene, xylene, acetone, naptha and hexane) Buspirone (Buspar®) • nitrites (amyl nitrite, butyl nitrite and cyclohexyl nitrite – also known as “poppers”) Non-Benzodiazepine Hypnotics (also belong to psychiatric medication category) • chloral hydrate • zopiclone (Imovane®) Other • GHB (gamma-hydroxybutyrate) • Rohypnol (flunitrazepam) CENTRAL NERVOUS SYSTEM STIMULANTS Amphetamines Caffeine • dextroamphetamine (Dexadrine®) Methelynedioxyamphetamine (MDA) • methamphetamine (“Crystal meth”) (also has hallucinogenic actions) • methylphenidate (Biphentin®, Concerta®, Ritalin®) • mixed amphetamine salts (Adderall XR®) 3,4-Methelynedioxymethamphetamine (MDMA, Ecstasy) (also has hallucinogenic actions) Cocaine/Crack -

A Acetylcholine Anticholinergic Drugs, 49 Cholinergic Wake-Promoting
Index A C Acetylcholine Cataplexy anticholinergic drugs, 49 GHB, 37 cholinergic wake-promoting system, 48 narcolepsy type 1, 215 cholinesterase inhibitors, 48–49 narcolepsy type 2, 215 milameline, 49 sleep-promoting orexinergic inhibitors, 46 nicotine, 49 SXB, 238–240 receptors, 48 tricyclic antidepressants, 253 sleep-promoting cholinergic Cell replacement therapy, 253 inhibitors, 49 Central sleep apnea (CSA) syndrome, 76 Adenosine Cheyne–Stokes breathing (CSB), 76 adenosine-mediated sleep-promoting Cholinesterase inhibitors system, 41 donepezil, 49 receptors, 42 physostigmine, 48 sleep-promoting adenosine receptor Chronic insomnia agonists, 42 dose discrimination, lack of, 168 wake-promoting adenosine receptor psychiatric comorbidities, 169 antagonists, 42 short-term efficacy and long-term safety, Amantadine, 77 167–168 Armodafinil sleep induction and maintenance, 168–169 chemical structure, 212 Chronic obstructive sleep apnea multiple sclerosis, 222 (OSA), 178–179 narcolepsy, 218 Chronic primary insomnia obstructive sleep apnea, 219–221 adverse effects, 165, 167 pharmacokinetics, 214 comorbid psychiatric disorders, 164 R enantiomer, 213 double-blind trial, 164 safety, 224–225 efficacy, 165 shift work disorder, 223 long-term trial, 165 open-label extension phase, 165 post hoc analysis, 165–166 B psychomotor performance, 164–165 Benzodiazepine Withdrawal Symptom rebound insomnia, 164 Questionnaire (BWSQ), 183 WASO, 164–165 © Springer International Publishing Switzerland 2015 289 A. Guglietta (ed.), Drug Treatment of Sleep Disorders, Milestones