Genetic Renal Diseases: the Emerging Role of Zebrafish Models
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rnase a Cleanup of DNA Samples Version Number: 1.0 Version 1.0 Date: 12/21/2016 Author(S): Yuko Yoshinaga, Eileen Dalin Reviewed/Revised By
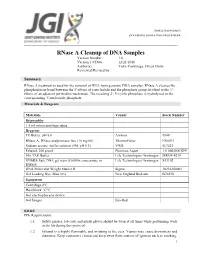
SAMPLE MANAGEMENT STANDARD OPERATING PROCEDURE RNase A Cleanup of DNA Samples Version Number: 1.0 Version 1.0 Date: 12/21/2016 Author(s): Yuko Yoshinaga, Eileen Dalin Reviewed/Revised by: Summary RNase A treatment is used for the removal of RNA from genomic DNA samples. RNase A cleaves the phosphodiester bond between the 5'-ribose of a nucleotide and the phosphate group attached to the 3'- ribose of an adjacent pyrimidine nucleotide. The resulting 2', 3'-cyclic phosphate is hydrolyzed to the corresponding 3'-nucleoside phosphate. Materials & Reagents Materials Vendor Stock Number Disposables 1.5 ml microcentrifuge tubes Reagents TE Buffer, pH 8.0 Ambion 9849 RNase A, DNase and protease-free (10 mg/ml) ThermoFisher EN0531 Sodium acetate buffer solution (3M, pH 5.2) VWR 567422 Ethanol, 200 proof Pharmco-Aaper 111000200CSPP 50x TAE Buffer Life Technologies/ Invitrogen MRGF-4210 SYBR® Safe DNA gel stain (10,000x concentrate in Life Technologies/ Invitrogen S33102 DMSO) DNA Molecular Weight Marker II Sigma 10236250001 Gel Loading Dye, Blue (6x) New England BioLabs B7021S Equipment Centrifuge 4°C Heat block 37°C Gel electrophoresis device Gel Imager Bio-Rad EH&S PPE Requirements: 1.1 Safety glasses, lab coat, and nitrile gloves should be worn at all times while performing work in the lab during this protocol. 1.2 Ethanol is a highly flammable and irritating to the eyes. Vapors may cause drowsiness and dizziness. Keep containers closed and keep away from sources of ignition such as smoking. 1 SAMPLE MANAGEMENT STANDARD OPERATING PROCEDURE Avoid contact with skin and eyes. In case of contact with eyes, rinse immediately with plenty of water and seek medical advice. -

Protein Interaction Network of Alternatively Spliced Isoforms from Brain Links Genetic Risk Factors for Autism
ARTICLE Received 24 Aug 2013 | Accepted 14 Mar 2014 | Published 11 Apr 2014 DOI: 10.1038/ncomms4650 OPEN Protein interaction network of alternatively spliced isoforms from brain links genetic risk factors for autism Roser Corominas1,*, Xinping Yang2,3,*, Guan Ning Lin1,*, Shuli Kang1,*, Yun Shen2,3, Lila Ghamsari2,3,w, Martin Broly2,3, Maria Rodriguez2,3, Stanley Tam2,3, Shelly A. Trigg2,3,w, Changyu Fan2,3, Song Yi2,3, Murat Tasan4, Irma Lemmens5, Xingyan Kuang6, Nan Zhao6, Dheeraj Malhotra7, Jacob J. Michaelson7,w, Vladimir Vacic8, Michael A. Calderwood2,3, Frederick P. Roth2,3,4, Jan Tavernier5, Steve Horvath9, Kourosh Salehi-Ashtiani2,3,w, Dmitry Korkin6, Jonathan Sebat7, David E. Hill2,3, Tong Hao2,3, Marc Vidal2,3 & Lilia M. Iakoucheva1 Increased risk for autism spectrum disorders (ASD) is attributed to hundreds of genetic loci. The convergence of ASD variants have been investigated using various approaches, including protein interactions extracted from the published literature. However, these datasets are frequently incomplete, carry biases and are limited to interactions of a single splicing isoform, which may not be expressed in the disease-relevant tissue. Here we introduce a new interactome mapping approach by experimentally identifying interactions between brain-expressed alternatively spliced variants of ASD risk factors. The Autism Spliceform Interaction Network reveals that almost half of the detected interactions and about 30% of the newly identified interacting partners represent contribution from splicing variants, emphasizing the importance of isoform networks. Isoform interactions greatly contribute to establishing direct physical connections between proteins from the de novo autism CNVs. Our findings demonstrate the critical role of spliceform networks for translating genetic knowledge into a better understanding of human diseases. -

Secretariat of the CBD Technical Series No. 82 Convention on Biological Diversity
Secretariat of the CBD Technical Series No. 82 Convention on Biological Diversity 82 SYNTHETIC BIOLOGY FOREWORD To be added by SCBD at a later stage. 1 BACKGROUND 2 In decision X/13, the Conference of the Parties invited Parties, other Governments and relevant 3 organizations to submit information on, inter alia, synthetic biology for consideration by the Subsidiary 4 Body on Scientific, Technical and Technological Advice (SBSTTA), in accordance with the procedures 5 outlined in decision IX/29, while applying the precautionary approach to the field release of synthetic 6 life, cell or genome into the environment. 7 Following the consideration of information on synthetic biology during the sixteenth meeting of the 8 SBSTTA, the Conference of the Parties, in decision XI/11, noting the need to consider the potential 9 positive and negative impacts of components, organisms and products resulting from synthetic biology 10 techniques on the conservation and sustainable use of biodiversity, requested the Executive Secretary 11 to invite the submission of additional relevant information on this matter in a compiled and synthesised 12 manner. The Secretariat was also requested to consider possible gaps and overlaps with the applicable 13 provisions of the Convention, its Protocols and other relevant agreements. A synthesis of this 14 information was thus prepared, peer-reviewed and subsequently considered by the eighteenth meeting 15 of the SBSTTA. The documents were then further revised on the basis of comments from the SBSTTA 16 and peer review process, and submitted for consideration by the twelfth meeting of the Conference of 17 the Parties to the Convention on Biological Diversity. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

U6 Small Nuclear RNA Is Transcribed by RNA Polymerase III (Cloned Human U6 Gene/"TATA Box"/Intragenic Promoter/A-Amanitin/La Antigen) GARY R
Proc. Nati. Acad. Sci. USA Vol. 83, pp. 8575-8579, November 1986 Biochemistry U6 small nuclear RNA is transcribed by RNA polymerase III (cloned human U6 gene/"TATA box"/intragenic promoter/a-amanitin/La antigen) GARY R. KUNKEL*, ROBIN L. MASERt, JAMES P. CALVETt, AND THORU PEDERSON* *Cell Biology Group, Worcester Foundation for Experimental Biology, Shrewsbury, MA 01545; and tDepartment of Biochemistry, University of Kansas Medical Center, Kansas City, KS 66103 Communicated by Aaron J. Shatkin, August 7, 1986 ABSTRACT A DNA fragment homologous to U6 small 4A (20) was screened with a '251-labeled U6 RNA probe (21, nuclear RNA was isolated from a human genomic library and 22) using a modified in situ plaque hybridization protocol sequenced. The immediate 5'-flanking region of the U6 DNA (23). One of several positive clones was plaque-purified and clone had significant homology with a potential mouse U6 gene, subsequently shown by restriction mapping to contain a including a "TATA box" at a position 26-29 nucleotides 12-kilobase-pair (kbp) insert. A 3.7-kbp EcoRI fragment upstream from the transcription start site. Although this containing U6-hybridizing sequences was subcloned into sequence element is characteristic of RNA polymerase II pBR322 for further restriction mapping. An 800-base-pair promoters, the U6 gene also contained a polymerase III "box (bp) DNA fragment containing U6 homologous sequences A" intragenic control region and a typical run of five thymines was excised using Ava I and inserted into the Sma I site of at the 3' terminus (noncoding strand). The human U6 DNA M13mp8 replicative form DNA (M13/U6) (24). -

Guidelines on Paediatric Urology S
Guidelines on Paediatric Urology S. Tekgül (Chair), H.S. Dogan, E. Erdem (Guidelines Associate), P. Hoebeke, R. Ko˘cvara, J.M. Nijman (Vice-chair), C. Radmayr, M.S. Silay (Guidelines Associate), R. Stein, S. Undre (Guidelines Associate) European Society for Paediatric Urology © European Association of Urology 2015 TABLE OF CONTENTS PAGE 1. INTRODUCTION 7 1.1 Aim 7 1.2 Publication history 7 2. METHODS 8 3. THE GUIDELINE 8 3A PHIMOSIS 8 3A.1 Epidemiology, aetiology and pathophysiology 8 3A.2 Classification systems 8 3A.3 Diagnostic evaluation 8 3A.4 Disease management 8 3A.5 Follow-up 9 3A.6 Conclusions and recommendations on phimosis 9 3B CRYPTORCHIDISM 9 3B.1 Epidemiology, aetiology and pathophysiology 9 3B.2 Classification systems 9 3B.3 Diagnostic evaluation 10 3B.4 Disease management 10 3B.4.1 Medical therapy 10 3B.4.2 Surgery 10 3B.5 Follow-up 11 3B.6 Recommendations for cryptorchidism 11 3C HYDROCELE 12 3C.1 Epidemiology, aetiology and pathophysiology 12 3C.2 Diagnostic evaluation 12 3C.3 Disease management 12 3C.4 Recommendations for the management of hydrocele 12 3D ACUTE SCROTUM IN CHILDREN 13 3D.1 Epidemiology, aetiology and pathophysiology 13 3D.2 Diagnostic evaluation 13 3D.3 Disease management 14 3D.3.1 Epididymitis 14 3D.3.2 Testicular torsion 14 3D.3.3 Surgical treatment 14 3D.4 Follow-up 14 3D.4.1 Fertility 14 3D.4.2 Subfertility 14 3D.4.3 Androgen levels 15 3D.4.4 Testicular cancer 15 3D.5 Recommendations for the treatment of acute scrotum in children 15 3E HYPOSPADIAS 15 3E.1 Epidemiology, aetiology and pathophysiology -

Transcriptomic Analysis of Native Versus Cultured Human and Mouse Dorsal Root Ganglia Focused on Pharmacological Targets Short
bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Transcriptomic analysis of native versus cultured human and mouse dorsal root ganglia focused on pharmacological targets Short title: Comparative transcriptomics of acutely dissected versus cultured DRGs Andi Wangzhou1, Lisa A. McIlvried2, Candler Paige1, Paulino Barragan-Iglesias1, Carolyn A. Guzman1, Gregory Dussor1, Pradipta R. Ray1,#, Robert W. Gereau IV2, # and Theodore J. Price1, # 1The University of Texas at Dallas, School of Behavioral and Brain Sciences and Center for Advanced Pain Studies, 800 W Campbell Rd. Richardson, TX, 75080, USA 2Washington University Pain Center and Department of Anesthesiology, Washington University School of Medicine # corresponding authors [email protected], [email protected] and [email protected] Funding: NIH grants T32DA007261 (LM); NS065926 and NS102161 (TJP); NS106953 and NS042595 (RWG). The authors declare no conflicts of interest Author Contributions Conceived of the Project: PRR, RWG IV and TJP Performed Experiments: AW, LAM, CP, PB-I Supervised Experiments: GD, RWG IV, TJP Analyzed Data: AW, LAM, CP, CAG, PRR Supervised Bioinformatics Analysis: PRR Drew Figures: AW, PRR Wrote and Edited Manuscript: AW, LAM, CP, GD, PRR, RWG IV, TJP All authors approved the final version of the manuscript. 1 bioRxiv preprint doi: https://doi.org/10.1101/766865; this version posted September 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Renal Agenesis, Renal Tubular Dysgenesis, and Polycystic Renal Diseases
Developmental & Structural Anomalies of the Genitourinary Tract DR. Alao MA Bowen University Teach Hosp Ogbomoso Picture test Introduction • Congenital Anomalies of the Kidney & Urinary Tract (CAKUT) Objectives • To review the embryogenesis of UGS and dysmorphogenesis of CAKUT • To describe the common CAKUT in children • To emphasize the role of imaging in the diagnosis of CAKUT Introduction •CAKUT refers to gross structural anomalies of the kidneys and or urinary tract present at birth. •Malformation of the renal parenchyma resulting in failure of normal nephron development as seen in renal dysplasia, renal agenesis, renal tubular dysgenesis, and polycystic renal diseases. Introduction •Abnormalities of embryonic migration of the kidneys as seen in renal ectopy (eg, pelvic kidney) and fusion anomalies, such as horseshoe kidney. •Abnormalities of the developing urinary collecting system as seen in duplicate collecting systems, posterior urethral valves, and ureteropelvic junction obstruction. Introduction •Prevalence is about 3-6 per 1000 births •CAKUT is one of the commonest anomalies found in human. •It constitute approximately 20 to 30 percent of all anomalies identified in the prenatal period •The presence of CAKUT in a child raises the chances of finding congenital anomalies of other organ-systems Why the interest in CAKUT? •Worldwide, CAKUT plays a causative role in 30 to 50 percent of cases of end-stage renal disease (ESRD), •The presence of CAKUT, especially ones affecting the bladder and lower tract adversely affects outcome of kidney graft after transplantation Why the interest in CAKUT? •They significantly predispose the children to UTI and urinary calculi •They may be the underlying basis for urinary incontinence Genes & Environment Interact to cause CAKUT? • Tens of different genes with role in nephrogenesis have been identified. -

Autophagy Suppresses Ras-Driven Epithelial Tumourigenesis by Limiting the Accumulation of Reactive Oxygen Species
OPEN Oncogene (2017) 36, 5576–5592 www.nature.com/onc ORIGINAL ARTICLE Autophagy suppresses Ras-driven epithelial tumourigenesis by limiting the accumulation of reactive oxygen species This article has been corrected since Advance Online Publication and a corrigendum is also printed in this issue. J Manent1,2,3,4,5,12, S Banerjee2,3,4,5, R de Matos Simoes6, T Zoranovic7,13, C Mitsiades6, JM Penninger7, KJ Simpson4,5, PO Humbert3,5,8,9,10 and HE Richardson1,2,5,8,11 Activation of Ras signalling occurs in ~ 30% of human cancers; however, activated Ras alone is not sufficient for tumourigenesis. In a screen for tumour suppressors that cooperate with oncogenic Ras (RasV12)inDrosophila, we identified genes involved in the autophagy pathway. Bioinformatic analysis of human tumours revealed that several core autophagy genes, including GABARAP, correlate with oncogenic KRAS mutations and poor prognosis in human pancreatic cancer, supporting a potential tumour- suppressive effect of the pathway in Ras-driven human cancers. In Drosophila, we demonstrate that blocking autophagy at any step of the pathway enhances RasV12-driven epithelial tissue overgrowth via the accumulation of reactive oxygen species and activation of the Jun kinase stress response pathway. Blocking autophagy in RasV12 clones also results in non-cell-autonomous effects with autophagy, cell proliferation and caspase activation induced in adjacent wild-type cells. Our study has implications for understanding the interplay between perturbations in Ras signalling and autophagy in tumourigenesis, -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

On the Move : Endocytic Trafficking in Cell Migration
Erschienen in: Cellular and Molecular Life Sciences ; 72 (2015), 11. - S. 2119-2134 https://dx.doi.org/10.1007/s00018-015-1855-9 On the move: endocytic trafficking in cell migration Tanja Maritzen • Hannah Schachtner • Daniel F. Legler Abstract Directed cell migration is a fundamental process unraveling the contribution of cellular trafficking pathways underlying diverse physiological and pathophysiological to cell migration. phenomena ranging from wound healing and induction of immune responses to cancer metastasis. Recent advances Keywords Endocytosis Á Cellular motility Á Clathrin Á reveal that endocytic trafficking contributes to cell migration Chemotaxis Á Signal transduction Á Vesicular transport in multiple ways. (1) At the level of chemokines and che- mokine receptors: internalization of chemokines by scavenger receptors is essential for shaping chemotactic Introduction gradients in tissue, whereas endocytosis of chemokine re- ceptors and their subsequent recycling is key for maintaining Diverse physiological processes ranging from embryonic a high responsiveness of migrating cells. (2) At the level of development to the induction of immune responses require integrin trafficking and focal adhesion dynamics: endosomal coordinated cell migration within the organism. In addi- pathways do not only modulate adhesion by delivering in- tion, migratory abilities of cells also represent a tegrins to their site of action, but also by supplying factors determining factor in pathological settings such as metas- for focal adhesion disassembly. (3) At the level of extra- tasis and inflammatory diseases. The term cell migration cellular matrix reorganization: endosomal transport comprises a number of different migration modes with contributes to tumor cell migration not only by targeting different mechanistic requirements. -

Genetic and Developmental Basis of Renal Coloboma (Papillorenal) Syndrome
Perspective Genetic and developmental basis of renal coloboma (papillorenal) syndrome Expert Rev. Ophthalmol. 4(2), 135–xxx (2009) Lisa A Schimmenti Renal coloboma syndrome, also known as papillorenal syndrome, is characterized by optic Department of Pediatrics and nerve anomalies and kidney hypodysplasia. Autosomal dominant mutations in the gene Ophthalmology, University of encoding the paired box transcription factor PAX2 can be identified in nearly half of all Minnesota Medical School, 420 patients with this phenotype. The primary ophthalmologic findings include congenital central Delaware Street Southeast, retinal vasculature absence associated with abnormalities in retinal blood vessel patterning MMC 730, Minnesota, and deeply excavated optic discs. Other published findings include optic nerve hypoplasia, MN 55455, USA optic nerve cyst, optic nerve pits, retinal coloboma, microphthalmia and scleral staphyloma. Tel.: +1 612 624 5613 Visual acuity ranges from normal to severe impairment. Up to one third of affected patients Fax: +1 612 626 2993 will develop end-stage renal disease. Mouse and zebrafish withPax2/pax2a mutations provide [email protected] developmentally based explanations for the observed phenotypic observations in affected patients. KEYWORDS: optic nerve coloboma • optic nerve dysplasia • papillorenal syndrome • PAX2 • renal coloboma syndrome The clinical presentation of optic nerve anomalies total of 10 years later, Weaver et al. reported a case associated with renal hypodysplasia should alert the of two brothers, both with optic nerve colobomas, clinician to the possibility that a patient may have interstitial nephritis and renal failure [3]. Weaver renal coloboma syndrome, a condition also known noted the similarity of the optic nerve colobomas as papillorenal syndrome (OMIM#120330). The in his patients with the ‘morning glory anomaly’, optic nerve findings could be described as a ‘dys- previously reported by Karcher et al.