Molecular and Cellular Mechanisms Underlying the Antidepressant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RAP-MD-05 GLYX13-C-203 Protocol Amendment 3 Final-R
NCT02192099 Study ID: GLYX13‐C‐203 Title: Open Label Extension for Subjects with Inadequate/Partial Response to Antidepressants during the Current Episode of Major Depressive Disorder Previously Treated with Rapastinel (GLYX‐13) (Extension of GLYX13‐C‐202, NCT01684163) Protocol Amendment 3 Date: 23 Nov 2016 Clinical Study Protocol Protocol Number: GLYX13-C-203 Study Drug: Rapastinel (GLYX-13) Injection (rapastinel Injection) FDA ID: 107,974 Clinicaltrials.gov: Title: Open Label Extension for Subjects with Inadequate/Partial Response to Antidepressants during the Current Episode of Major Depressive Disorder Previously Treated with Rapastinel (GLYX-13) (Extension of GLYX13-C-202, NCT01684163) Study Phase: 2 Sponsor: Naurex, Inc, an affiliate of Allergan, plc. Date: Amendment 3 dated 23 November 2016 Replaces Amendment 2 dated 20 January 2015 This document is a confidential communication from Naurex, Inc, an affiliate of Allergan, plc.. Acceptance of this document constitutes an agreement by the recipient(s) that no information contained herein will be published or disclosed without prior written approval from Allergan, plc., except that this document may be disclosed to appropriate Institutional Review Boards (IRBs) under the condition that they are also required to maintain confidentiality. Naurex, Inc, an affiliate of Allergan, plc. Protocol GLYX13-C-203 INVESTIGATOR SIGNATURE PAGE The signature of the investigator below constitutes his/her approval of this protocol and provides the necessary assurances that this study will be conducted according to all stipulations of the protocol as specified in both the clinical and administrative sections, including all statements regarding confidentiality. This trial will be conducted in compliance with the protocol and all applicable regulatory requirements, in accordance with Good Clinical Practices (GCPs), including International Conference on Harmonization (ICH) Guidelines, and in general conformity with the most recent version of the Declaration of Helsinki. -

Sciatica and Chronic Pain
Sciatica and Chronic Pain Past, Present and Future Robert W. Baloh 123 Sciatica and Chronic Pain Robert W. Baloh Sciatica and Chronic Pain Past, Present and Future Robert W. Baloh, MD Department of Neurology University of California, Los Angeles Los Angeles, CA, USA ISBN 978-3-319-93903-2 ISBN 978-3-319-93904-9 (eBook) https://doi.org/10.1007/978-3-319-93904-9 Library of Congress Control Number: 2018952076 © Springer International Publishing AG, part of Springer Nature 2019 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The publisher, the authors, and the editors are safe to assume that the advice and information in this book are believed to be true and accurate at the date of publication. Neither the publisher nor the authors or the editors give a warranty, express or implied, with respect to the material contained herein or for any errors or omissions that may have been made. The publisher remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. -

A Human Stem Cell-Derived Test System for Agents Modifying Neuronal N
Archives of Toxicology (2021) 95:1703–1722 https://doi.org/10.1007/s00204-021-03024-0 IN VITRO SYSTEMS A human stem cell‑derived test system for agents modifying neuronal 2+ N‑methyl‑D‑aspartate‑type glutamate receptor Ca ‑signalling Stefanie Klima1,2 · Markus Brüll1 · Anna‑Sophie Spreng1,3 · Ilinca Suciu1,3 · Tjalda Falt1 · Jens C. Schwamborn4 · Tanja Waldmann1 · Christiaan Karreman1 · Marcel Leist1,5 Received: 28 October 2020 / Accepted: 4 March 2021 / Published online: 13 March 2021 © The Author(s) 2021 Abstract Methods to assess neuronal receptor functions are needed in toxicology and for drug development. Human-based test systems that allow studies on glutamate signalling are still scarce. To address this issue, we developed and characterized pluripotent stem cell (PSC)-based neural cultures capable of forming a functional network. Starting from a stably proliferating neu- roepithelial stem cell (NESC) population, we generate “mixed cortical cultures” (MCC) within 24 days. Characterization by immunocytochemistry, gene expression profling and functional tests (multi-electrode arrays) showed that MCC contain various functional neurotransmitter receptors, and in particular, the N-methyl-D-aspartate subtype of ionotropic glutamate receptors (NMDA-R). As this important receptor is found neither on conventional neural cell lines nor on most stem cell- derived neurons, we focused here on the characterization of rapid glutamate-triggered Ca2+ signalling. Changes of the intra- 2+ cellular free calcium ion concentration ([Ca ]i) were measured by fuorescent imaging as the main endpoint, and a method to evaluate and quantify signals in hundreds of cells at the same time was developed. We observed responses to glutamate in the low µM range. -

Poster Session III, December 6, 2017
Neuropsychopharmacology (2017) 42, S476–S652 © 2017 American College of Neuropsychopharmacology. All rights reserved 0893-133X/17 www.neuropsychopharmacology.org Poster Session III a high-resolution research tomograph (HRRT), and struc- Palm Springs, California, December 3–7, 2017 tural (T1) MRI using a 3-Tesla scanner. PET data analyses were carried out using the validated 2-tissue compartment Sponsorship Statement: Publication of this supplement is model to determine the total volume of distribution (VT) of sponsored by the ACNP. [18F]FEPPA. Individual contributor disclosures may be found within the Results: Results show significant inverse associations (con- abstracts. Part 1: All Financial Involvement with a pharma- trolling for rs6971 genotype) between neuroinflammation ceutical or biotechnology company, a company providing (VTs) and cortical thickness in the right medial prefrontal clinical assessment, scientific, or medical products or compa- cortex [r = -.562, p = .029] and the left dorsolateral nies doing business with or proposing to do business with prefrontal cortex [r = -.629, p = .012](p values are not ACNP over past 2 years (Calendar Years 2014–Present); Part 2: corrected for multiple comparisons). No significant associa- Income Sources & Equity of $10,000 per year or greater tions were found with surface area. (Calendar Years 2014 - Present): List those financial relation- Conclusions: These results, while preliminary, suggest links ships which are listed in part one and have a value greater than between the microglial activation/neuroinflammation and $10,000 per year, OR financial holdings that are listed in part cortical thickness in the dorsolateral prefrontal cortex and one and have a value of $10,000 or greater as of the date of medial prefrontal cortex in AD patients. -
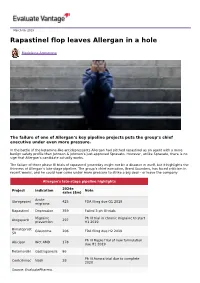
Rapastinel Flop Leaves Allergan in a Hole
March 06, 2019 Rapastinel flop leaves Allergan in a hole Madeleine Armstrong The failure of one of Allergan’s key pipeline projects puts the group’s chief executive under even more pressure. In the battle of the ketamine-like antidepressants Allergan had pitched rapastinel as an agent with a more benign safety profile than Johnson & Johnson’s just-approved Spravato. However, unlike Spravato, there is no sign that Allergan’s candidate actually works. The failure of three phase III trials of rapastinel yesterday might not be a disaster in itself, but it highlights the thinness of Allergan’s late-stage pipeline. The group’s chief executive, Brent Saunders, has faced criticism in recent weeks, and he could now come under more pressure to strike a big deal – or leave the company. Allergan's late-stage pipeline highlights 2024e Project Indication Note sales ($m) Acute Ubrogepant 425 FDA filing due Q1 2019 migraine Rapastinel Depression 359 Failed 3 ph III trials Migraine Ph III trial in chronic migraine to start Atogepant 297 prevention H1 2019 Bimatoprost Glaucoma 206 FDA filing due H2 2019 SR Ph III Maple trial of new formulation Abicipar Wet AMD 178 due H1 2019 Relamorelin Gastroparesis 86 Ph III Aurora trial due to complete Cenicriviroc Nash 28 2020 Source: EvaluatePharma. Activist shareholders have long been agitating for change at Allergan, and the latest failure will only provide more ammunition to those who want to split the roles of chairman and chief exec amid dissatisfaction with the group's acquisition strategy, and with its stock hovering around a five-year low. -

WO 2017/066590 Al 20 April 2017 (20.04.2017) P O P CT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2017/066590 Al 20 April 2017 (20.04.2017) P O P CT (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 38/06 (2006.01) A61K 31/519 (2006.01) kind of national protection available): AE, AG, AL, AM, A61 38/07 (2006.0V) A61K 31/551 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, A61K 31/13 (2006.01) A61K 31/5513 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, A61K 31/135 (2006.01) A61P 25/24 (2006.01) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, A61K 31/496 (2006.01) A61P 25/18 (2006.01) HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, (21) International Application Number: MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, PCT/US20 16/057071 OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (22) International Filing Date: SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, 14 October 2016 (14.10.201 6) TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, zw. (25) Filing Language: English (84) Designated States (unless otherwise indicated, for every (26) Publication Language: English kind of regional protection available): ARIPO (BW, GH, (30) Priority Data: GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, ST, SZ, 62/242,633 16 October 2015 (16. -

Advances in Non-Dopaminergic Treatments for Parkinson's Disease
REVIEW ARTICLE published: 22 May 2014 doi: 10.3389/fnins.2014.00113 Advances in non-dopaminergic treatments for Parkinson’s disease Sandy Stayte 1,2 and Bryce Vissel 1,2* 1 Neuroscience Department, Neurodegenerative Disorders Laboratory, Garvan Institute of Medical Research, Sydney, NSW, Australia 2 Faculty of Medicine, University of New South Wales, Sydney, NSW, Australia Edited by: Since the 1960’s treatments for Parkinson’s disease (PD) have traditionally been directed Eero Vasar, University of Tartu, to restore or replace dopamine, with L-Dopa being the gold standard. However, chronic Estonia L-Dopa use is associated with debilitating dyskinesias, limiting its effectiveness. This has Reviewed by: resulted in extensive efforts to develop new therapies that work in ways other than Andrew Harkin, Trinity College Dublin, Ireland restoring or replacing dopamine. Here we describe newly emerging non-dopaminergic Sulev Kõks, University of Tartu, therapeutic strategies for PD, including drugs targeting adenosine, glutamate, adrenergic, Estonia and serotonin receptors, as well as GLP-1 agonists, calcium channel blockers, iron Pille Taba, Universoty of Tartu, chelators, anti-inflammatories, neurotrophic factors, and gene therapies. We provide a Estonia Pekka T. Männistö, University of detailed account of their success in animal models and their translation to human clinical Helsinki, Finland trials. We then consider how advances in understanding the mechanisms of PD, genetics, *Correspondence: the possibility that PD may consist of multiple disease states, understanding of the Bryce Vissel, Neuroscience etiology of PD in non-dopaminergic regions as well as advances in clinical trial design Department, Neurodegenerative will be essential for ongoing advances. We conclude that despite the challenges ahead, Disorders Laboratory, Garvan Institute of Medical Research, patients have much cause for optimism that novel therapeutics that offer better disease 384 Victoria Street, Darlinghurst, management and/or which slow disease progression are inevitable. -

Therapy Focus – J&J Confirms Hope for New Mechanism in Depression
May 09, 2018 Therapy focus – J&J confirms hope for new mechanism in depression Amy Brown The first look at late-stage data on Johnson & Johnson’s hotly-tipped novel antidepressant esketamine came at a medical conference last weekend, and the results were not quite as strong as many were hoping to see. Encouraging signals could be certainly be found, however, and J&J seems undeterred from trying to seek regulatory approval. Others pursing NMDA modulation in depression are also likely to draw comfort in the results, which provide the first phase III validation of this mechanism, and a clear bar to beat (see table below). Hopes for esketamine and other products like it lie in their similarity to ketamine, which at low doses displays antidepressant effects that kick in very quickly. Traditional antidepressants which act via the serotonergic system – selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) – can take weeks to have an effect; a large proportion of patients fail to respond at all. Hence the need for both faster acting agents – for example in suicidal patients – and novel mechanisms to treat those who need different options. A new target NMDA receptor modulation is a novel mechanism in depression. Over the last decade researchers have become increasingly convinced that dysregulation of glutamate, a neurotransmitter which signals through NMDA, plays an important role in the condition. This system is already known to be a factor in cognitive function and neurodegeneration and Namenda, the NMDA antagonist mematine, has been available as a treatment for Alzheimer’s dementia for several years. -

Gottlieb's Shock Resignation Leaves Ripples in the Industry
15 March 2019 No. 3946 Scripscrip.pharmaintelligence.informa.com Pharma intelligence | informa time, which is difficult. He also used the office in a “forward-leaning way” not seen often. “He kind of drove the conversation through very good communication exter- nally,” Myers said. “He was able to use a lot of the ideas percolating in the agency, pack- age them and get them moved forward.” Gottlieb pushed FDA to the forefront of the drug pricing debate, a position the agency had not sought in the past. In his first speech to staff after confir- mation, he said that even though the agency cannot set drug prices, it can promote competition. Gottlieb was vocal in chastising the brand industry for blocking generic Credit: FDA Credit: competition, warning that Congress could make more drastic changes if it did not stop employing pay-for-delay and licensing tactics intended to pre- Gottlieb’s Shock Resignation vent patent challenges. (Also see “Got- tlieb: Real Risk Of Congressional Action If Leaves Ripples In The Industry Anti-Competitive Actions Continue” - Pink Sheet, 3 May, 2018.) DERRICK GINGERY [email protected] He also publicly released a list of com- panies thought to be using the Risk Evalu- S FDA Commissioner Scott Gott- being apart from my family for these past ation and Mitigation Strategy system to lieb, one of the most popular and two years and missing my wife and three prevent generic companies from purchas- Uvisible commissioners in decades, young children.” ing samples for testing, although it is not will end his tenure as head of FDA in about clear the move had much impact. -

Sustained Antidepressant Action of the N‑Methyl‑D‑Aspartate Receptor Antagonist MK‑801 in a Chronic Unpredictable Mild Stress Model
5376 EXPERIMENTAL AND THERAPEUTIC MEDICINE 16: 5376-5383, 2018 Sustained antidepressant action of the N‑methyl‑D‑aspartate receptor antagonist MK‑801 in a chronic unpredictable mild stress model BANG-KUN YANG1, JUN QIN2, YING NIE3 and JIN-CAO CHEN1 1Department of Neurosurgery, Zhongnan Hospital of Wuhan University, Wuhan, Hubei 430071; Departments of 2Neurosurgery and 3Children's Medical Center, Taihe Hospital, Hubei University of Medicine, Shiyan, Hubei 442600, P.R. China Received December 29, 2016; Accepted November 29, 2017 DOI: 10.3892/etm.2018.6876 Abstract. (5S,10R)-5-methyl-10,11-dihydro-5H-dibenzo(A,D) mice. Therefore, the present study revealed the sustained cyclohepten-5,10-imine hydrogen maleate (MK-801) is antidepressant effects of MK-801 in the CUMS model. an N-methyl-D-aspartate non-competitive antagonist that Furthermore, synaptogenesis and neuronal regeneration in the possesses useful biological properties, including anticon- prelimbic regions of mPFC, DG and CA3 of the hippocampus vulsant and anesthetic activities. Studies have indicated the may be implicated as mechanisms that promote a sustained rapid antidepressant effects of MK-801 in animal models. antidepressant response. However, there are no reports concerning a sustained anti- depressant effect in the chronic unpredictable mild stress Introduction (CUMS) model. Furthermore, the antidepressant mechanism remains unclear. The aim of the present study was to examine In addition to being the most prevalent mental disorder, the effects of MK-801 (0.1 mg/kg) and rapastinel (10 mg/kg) depression is one of the leading causes of disability across on depression-like behavior in CUMS mice and measure the world (1). -

Changes in Glutamate Levels Measured by Glutamate
Changes in glutamate levels measured by glutamate voltammetry in the rat medial prefrontal cortex after treatment with N-methyl-D-aspartate receptor antagonists (P.1.g.023) Irina Ionescu, Kelly Allers, Roberto Arban, Cornelia Dorner-Ciossek and Lothar Kussmaul Boehringer Ingelheim, CNS Diseases Research Background Hypothesized antidepressant MoA of NMDA-R antagonists: Disinhibition of glutamatergic neurons in the PFC N-methyl-D-aspartate receptor (NMDA-R) have been described as potential novel treatment options in the therapy of treatment-reistant depression (TRD). A single sub-anesthetic dose of the noncompetitive NMDA-R antagonist GABA ketamine has been shown to exert rapid-onset and long-lasting antidepressant Glutamate Glutamate NMDA-R effects in TRD patients; these effects were accompanied by brief psychotic Increased glutamate release episodes. Fast-onset antidepressant effects without psychotic side effects have also been described in the clinic for the NR2B-selective negative allosteric modulator (NAM) traxoprodil. However, other unspecific NMDA-R blockers, Synaptic plasticity such as lanicemine, failed to show fast-onset long-lasting antidepressant NMDA-R antagonists (ketamine, traxoprodil) effects in the clinic after single application. Here, we used glutamate AMPA-R AMPA-R voltammetry in rats in order to identify a preclinical predictor of clinical efficacy The increase in glutamate release as proof of circuit by circuit engagement in the prefrontal cortex (PFC). engagement and antidepressant activity can be measured by glutamate voltammetry. Using glutamate voltammetry to show circuit engagement by clinically active NMDA-R antagonists in the PFC Glutamate biosensor (Pinnacle Technology Inc., USA) Advantages of glutamate voltammetry Experimental design - fast response time Experiments were performed in Wistar Han rats implanted with Recording site: PFC - fast sampling time (1 Hz) guide cannulae at the specified coordinates. -

Ketamine: a Novel Antidepressant with a Fast Onset of Action?† COMMENTARY ON… COCHRANE CORNER Katharine Smith & Mary Jane Attenburrow
BJPsych Advances (2016), vol. 22, 216–221 doi: 10.1192/apt.22.4.216 ROUND THE CORNER Ketamine: a novel antidepressant with a fast onset of action?† COMMENTARY ON… COCHRANE CORNER Katharine Smith & Mary Jane Attenburrow Katharine Smith is an honorary For bipolar depression, the treatment challenge SUMMARY consultant psychiatrist at the is even greater. There is scarce evidence that National Institute for Health Glutamate receptor modulators, including antidepressants are effective as a first-line Research (NIHR) Oxford cognitive ketamine, are possible candidates for new health Clinical Research Facility treatment (Sidor 2012), and mood instability is an antidepressants with a novel mode of action. and Oxford University Department additional challenge. Current recommendations The pair of reviews discussed in this month’s of Psychiatry. Mary Jane (Kendall 2014) focus on the use of quetiapine; Attenburrow is Clinical Lead at Round the Corner considered their use in treating the NIHR Oxford cognitive health unipolar major depression and bipolar depression. lamotrigine, fluoxetine plus olanzapine and Clinical Research Facility, a Senior Promising results were seen for ketamine, but lithium are also recommended. A recent trial Research Fellow at Oxford University further studies are needed, in particular to (CEQUEL) demonst ra ted that there may be benefit Department of Psychiatry and an investigate whether the benefits are sustained in the combination of lamotrigine with quetiapine honorary consultant psychiatrist. Correspondence Dr Katharine or can be extended by repeated or adjunctive (Geddes 2016). Smith, NIHR Oxford cognitive health treatment, whether ketamine is effective in Although the differences in treatment response Clinical Research Facility, Warneford treatment resistance, whether other modes of between unipolar and bipolar depression Hospital, Oxford OX3 7JX, UK.