Community-Based Ebola Care Centres
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

G U I N E a Liberia Sierra Leone
The boundaries and names shown and the designations Mamou used on this map do not imply official endorsement or er acceptance by the United Nations. Nig K o L le n o G UINEA t l e a SIERRA Kindia LEONEFaranah Médina Dula Falaba Tabili ba o s a g Dubréka K n ie c o r M Musaia Gberia a c S Fotombu Coyah Bafodia t a e r G Kabala Banian Konta Fandié Kamakwie Koinadugu Bendugu Forécariah li Kukuna Kamalu Fadugu Se Bagbe r Madina e Bambaya g Jct. i ies NORTHERN N arc Sc Kurubonla e Karina tl it Mateboi Alikalia L Yombiro Kambia M Pendembu Bumbuna Batkanu a Bendugu b Rokupr o l e Binkolo M Mange Gbinti e Kortimaw Is. Kayima l Mambolo Makeni i Bendou Bodou Port Loko Magburaka Tefeya Yomadu Lunsar Koidu-Sefadu li Masingbi Koundou e a Lungi Pepel S n Int'l Airport or a Matotoka Yengema R el p ok m Freetown a Njaiama Ferry Masiaka Mile 91 P Njaiama- Wellington a Yele Sewafe Tongo Gandorhun o Hastings Yonibana Tungie M Koindu WESTERN Songo Bradford EAS T E R N AREA Waterloo Mongeri York Rotifunk Falla Bomi Kailahun Buedu a i Panguma Moyamba a Taiama Manowa Giehun Bauya T Boajibu Njala Dambara Pendembu Yawri Bendu Banana Is. Bay Mano Lago Bo Segbwema Daru Shenge Sembehun SOUTHE R N Gerihun Plantain Is. Sieromco Mokanje Kenema Tikonko Bumpe a Blama Gbangbatok Sew Tokpombu ro Kpetewoma o Sh Koribundu M erb Nitti ro River a o i Turtle Is. o M h Sumbuya a Sherbro I. -
Local Council Ward Boundary Delimitation Report
April 2008 NATIONAL ELECTORAL COMMISSION Sierra Leone Local Council Ward Boundary Delimitation Report Volume One February 2008 This page is intentionally left blank TABLE OF CONTENTS Foreword 1 Executive Summary 3 Introduction 5 Stages in the Ward Boundary Delimitation Process 7 Stage One: Establishment of methodology including drafting of regulations 7 Stage Two: Allocation of Local Councils seats to localities 13 Stage Three: Drawing of Boundaries 15 Stage Four: Sensitization of Stakeholders and General Public 16 Stage Five: Implement Ward Boundaries 17 Conclusion 18 APPENDICES A. Database for delimiting wards for the 2008 Local Council Elections 20 B. Methodology for delimiting ward boundaries using GIS technology 21 B1. Brief Explanation of Projection Methodology 22 C. Highest remainder allocation formula for apportioning seats to localities for the Local Council Elections 23 D. List of Tables Allocation of 475 Seats to 19 Local Councils using the highest remainder method 24 25% Population Deviation Range 26 Ward Numbering format 27 Summary Information on Wards 28 E. Local Council Ward Delimitation Maps showing: 81 (i) Wards and Population i (ii) Wards, Chiefdoms and sections EASTERN REGION 1. Kailahun District Council 81 2. Kenema City Council 83 3. Kenema District Council 85 4. Koidu/New Sembehun City Council 87 5. Kono District Council 89 NORTHERN REGION 6. Makeni City Council 91 7. Bombali District Council 93 8. Kambia District Council 95 9. Koinadugu District Council 97 10. Port Loko District Council 99 11. Tonkolili District Council 101 SOUTHERN REGION 12. Bo City Council 103 13. Bo District Council 105 14. Bonthe Municipal Council 107 15. -
Summary of Recovery Requirements (Us$)
National Recovery Strategy Sierra Leone 2002 - 2003 EXECUTIVE SUMMARY TABLE OF CONTENTS EXECUTIVE SUMMARY 3 4. RESTORATION OF THE ECONOMY 48 INFORMATION SHEET 7 MAPS 8 Agriculture and Food-Security 49 Mining 53 INTRODUCTION 9 Infrastructure 54 Monitoring and Coordination 10 Micro-Finance 57 I. RECOVERY POLICY III. DISTRICT INFORMATION 1. COMPONENTS OF RECOVERY 12 EASTERN REGION 60 Government 12 1. Kailahun 60 Civil Society 12 2. Kenema 63 Economy & Infrastructure 13 3. Kono 66 2. CROSS CUTTING ISSUES 14 NORTHERN REGION 69 HIV/AIDS and Preventive Health 14 4. Bombali 69 Youth 14 5. Kambia 72 Gender 15 6. Koinadugu 75 Environment 16 7. Port Loko 78 8. Tonkolili 81 II. PRIORITY AREAS OF SOUTHERN REGION 84 INTERVENTION 9. Bo 84 10. Bonthe 87 11. Moyamba 90 1. CONSOLIDATION OF STATE AUTHORITY 18 12. Pujehun 93 District Administration 18 District/Local Councils 19 WESTERN AREA 96 Sierra Leone Police 20 Courts 21 Prisons 22 IV. FINANCIAL REQUIREMENTS Native Administration 23 2. REBUILDING COMMUNITIES 25 SUMMARY OF RECOVERY REQUIREMENTS Resettlement of IDPs & Refugees 26 CONSOLIDATION OF STATE AUTHORITY Reintegration of Ex-Combatants 38 REBUILDING COMMUNITIES Health 31 Water and Sanitation 34 PEACE-BUILDING AND HUMAN RIGHTS Education 36 RESTORATION OF THE ECONOMY Child Protection & Social Services 40 Shelter 43 V. ANNEXES 3. PEACE-BUILDING AND HUMAN RIGHTS 46 GLOSSARY NATIONAL RECOVERY STRATEGY - 3 - EXECUTIVE SUMMARY ▪ Deployment of remaining district officials, EXECUTIVE SUMMARY including representatives of line ministries to all With Sierra Leone’s destructive eleven-year conflict districts (by March). formally declared over in January 2002, the country is ▪ Elections of District Councils completed and at last beginning the task of reconstruction, elected District Councils established (by June). -
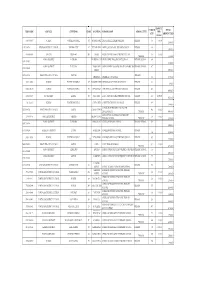
Emis Code Council Chiefdom Ward Location School Name
AMOUNT ENROLM TOTAL EMIS CODE COUNCIL CHIEFDOM WARD LOCATION SCHOOL NAME SCHOOL LEVEL PER ENT AMOUNT PAID CHILD 5103-2-09037 WARDC WATERLOO RURAL 391 ROGBANGBA ABDUL JALIL ACADEMY PRIMARY PRIMARY 369 10,000 3,690,000 1291-2-00714 KENEMA DISTRICT COUNCIL KENEMA CITY 67 FULAWAHUN ABDUL JALIL ISLAMIC PRIMARY SCHOOL PRIMARY 380 3,800,000 4114-2-06856 BO CITY TIKONKO 289 SAMIE ABDUL TAWAB HAIKAL PRIMARY SCHOOL 610 10,000 PRIMARY 6,100,000 KONO DISTRICT TANKORO DOWN BALLOP ABDULAI IBN ABASS PRIMARY SCHOOL PRIMARY SCHOOL 694 1391-2-02007 6,940,000 KONO DISTRICT TANKORO TAMBA ABU ABDULAI IBNU MASSOUD ANSARUL ISLAMIC MISPRIMARY SCHOOL 407 1391-2-02009 STREET 4,070,000 5208-2-10866 FREETOWN CITY COUNCIL WEST III PRIMARY ABERDEEN ABERDEEN MUNICIPAL 366 3,660,000 5103-2-09002 WARDC WATERLOO RURAL 397 KOSSOH TOWN ABIDING GRACE PRIMARY SCHOOL PRIMARY 62 620,000 5103-2-08963 WARDC WATERLOO RURAL 373 BENGUEMA ABNAWEE ISLAMIC PRIMARY SCHOOOL PRIMARY 405 4,050,000 4109-2-06695 BO DISTRICT KAKUA 303 KPETEMA ACEF / MOUNT HORED PRIMARY SCHOOL PRIMARY 411 10,000.00 4,110,000 Not found WARDC WATERLOO RURAL COLE TOWN ACHIEVERS PRIMARY TUTORAGE PRIMARY 388 3,880,000 ACTION FOR CHILDREN AND YOUTH 5205-2-09766 FREETOWN CITY COUNCIL EAST III CALABA TOWN 460 10,000 DEVELOPMENT PRIMARY 4,600,000 ADA GORVIE MEMORIAL PREPARATORY 320401214 BONTHE DISTRICT IMPERRI MORIBA TOWN 320 10,000 PRIMARY SCHOOL PRIMARY 3,200,000 KONO DISTRICT TANKORO BONGALOW ADULLAM PRIMARY SCHOOL PRIMARY SCHOOL 323 1391-2-01954 3,230,000 1109-2-00266 KAILAHUN DISTRICT LUAWA KAILAHUN ADULLAM PRIMARY -

Report on Country of Return Information
The Country of Return Information Project functions as a network of NGO’s for the collection and transfer of specific information on reintegration possibilities for potential returnees and their counsellors. All questions you may have on reintegration possibilities and on which you don’t find the answer in this country sheet, can be directed to the helpdesk “Country of Return Information”. E-mail: [email protected] COUNTRY SHEET SIERRA LEONE BO and KONO District The Country of Return Information Project runs until the end of 2007 and is funded by the European Community. August 2007 The European Commission is not responsible for any use that may be made of the information provided. Sole responsibility for its content lies with the author. DISCLAIMER This Country Sheet is for informational purposes only and no rights can be derived from its contents. The CRI-partners will do their utmost to include accurate, corroborated, transparent and up-to-date information, but make no warrants as to its accuracy or completeness. Consequently, the CRI- partners do not accept responsibility in any way for the information in this Country Sheet and accept no liability for damages of any kind arising from using the information in this Country Sheet. The information in this Country Sheet has been retrieved in collaboration with local partners. This Country Sheet contains links to websites that are created and maintained by other organizations. The CRI-project does not take any responsibility for the content of these websites. The CRI-partners are the partners who participate fully in the CRI- project: Vluchtelingenwerk Vlaanderen, Caritas International Belgium, Consiglio Italiano per i Rifugiati, Coordination et Initiatives pour les Réfugiés et Étrangers and Hungarian Helsinki Committee. -

The Chiefdoms of Sierra Leone
The Chiefdoms of Sierra Leone Tristan Reed1 James A. Robinson2 July 15, 2013 1Harvard University, Department of Economics, Littauer Center, 1805 Cambridge Street, Cambridge MA 02138; E-mail: [email protected]. 2Harvard University, Department of Government, IQSS, 1737 Cambridge Street., N309, Cambridge MA 02138; E-mail: [email protected]. Abstract1 In this manuscript, a companion to Acemoglu, Reed and Robinson (2013), we provide a detailed history of Paramount Chieftaincies of Sierra Leone. British colonialism transformed society in the country in 1896 by empowering a set of Paramount Chiefs as the sole authority of local government in the newly created Sierra Leone Protectorate. Only individuals from the designated \ruling families" of a chieftaincy are eligible to become Paramount Chiefs. In 2011, we conducted a survey in of \encyclopedias" (the name given in Sierra Leone to elders who preserve the oral history of the chieftaincy) and the elders in all of the ruling families of all 149 chieftaincies. Contemporary chiefs are current up to May 2011. We used the survey to re- construct the history of the chieftaincy, and each family for as far back as our informants could recall. We then used archives of the Sierra Leone National Archive at Fourah Bay College, as well as Provincial Secretary archives in Kenema, the National Archives in London and available secondary sources to cross-check the results of our survey whenever possible. We are the first to our knowledge to have constructed a comprehensive history of the chieftaincy in Sierra Leone. 1Oral history surveys were conducted by Mohammed C. Bah, Alimamy Bangura, Alieu K. -

Pauline Oosterhoff, Annie Wilkinson, Esther Yei-Mokuwa Ebola Response Anthropology Platform February 2015
POLICY BRIEFING ON Community-based Ebola Care Centres AUTHORS: Pauline Oosterhoff, Annie Wilkinson, Esther Yei-Mokuwa Ebola Response Anthropology Platform February 2015 A component of the Ebola epidemic control policy in Sierra Leone is triage and isolation in decentralised Community Care Centres (CCCs) or Holding Units, from where transfer to Ebola treatment units (ETUs) is arranged for those diagnosed as positive. The epidemic is currently waning, there are sufficient beds in the ETU, yet new micro-epidemics emerge, raising questions about the future role and relevance of the CCC. This briefing summarizes the preliminary findings of a formative evaluation conducted by the UK based Ebola Response Anthropology Platform in February 2015 on views of community leaders and residents towards 1) their engagement with the development and management of the CCC and 2) future usages of the CCCs physical structure, equipment and staff. A full data analysis is ongoing. We hope that the views presented here provide various options for the use of the CCCs during the bumpy road to zero. Methods: A Sierra Leonean research team with an appropriate mix of local language skills visited 14 villages in 7 chiefdoms in Port Loko, Kambia, Tonkolili and Kono. Two villages were selected in each chiefdom: one which was hosting the CCC (or closest to it) and one which was in the same chiefdom, so plausibly part of the CCC catchment area. We also conducted interviews with residents in one urban area close to an isolation centre in Maforkie chiefdom in Port Loko. Sites in each chiefdom were selected in consultation with the District Ebola Response Committee (DERC) and Paramount chiefs. -

In-Country Research and Data Collection on Forced Labor and Child Labor in the Production of Goods
In-country Research and Data Collection on Forced Labor and Child Labor in the Production of Goods Sierra Leone Submitted to: U.S. Department of Labor Bureau of International Labor Affairs Office of Child Labor, Forced Labor, and Human Trafficking Frances Perkins Building 200 Constitution Ave., NW Washington, D.C. 20210 Submitted by: Macro International Inc. 11785 Beltsville Drive, Suite 300 Calverton, MD 20705 Main Telephone: (301) 572-0200 Facsimile: (301) 572-0999 www.macrointernational.com Funding for this research was provided by the United States Department of Labor under Contract number DOLQ059622436. This research does not necessarily reflect the views or policies of the United States Department of Labor, nor does the mention of trade names, commercial products, or organizations imply endorsement by the United States Government. Table of Contents Summaries of Goods Researched .................................................................................... 4 Interview Type 1 ............................................................................................................... 6 Interview Type 2 ............................................................................................................. 75 Site Visit Note .................................................................................................................. 92 Annotated Bibliography: Sierra Leone....................................................................... 102 Comments on MACRO In Country Research –Sierra Leone ................................ -

Sierra Leone Unipsil
13o 30' 13o 00' 12o 30' 12o 00' 11o 30' 11o 00' 10o 30' Mamou The boundaries and names shown and the designations used on this map do not imply ger GUINEA official endorsemenNt ior acceptance by the UNIPSIL K L United Nations. o l o e l Deployment as of n a t e SeptemberKindia 2008 Faranah o o 10 00' Médina 10 00' National capital Dula Provincial capital Tabili s a Falaba ie ab o c K g Dubréka Town, village r n a o c M S Musaia International boundary t Gberia Coyah a Bafodia e Provincial boundary r Fotombu G Kabala Banian Konta Bendugu 9o 30' Fandié Kamakwie NORTHERN Koinadugu 9o 30' Forécariah Kamalu li Kukuna Fadugu Se s ie c Madina r r a Bagbe e c g Jct. e S i tl N Bambaya Lit Ribia Karina Alikalia Kurubonla Mateboi Kambia M Pendembu Yombiro ab Batkanuo Bendugu l e Bumbuna o o 9 00' Rokupr a 9 00' n Mamuka a Mange Gbinti p Binkolo m Kayima Mambolo a Port Baibunda Makeni P HQ UNIPSIL Loko Bendou Lungi Magburaka Tefeya Mape Yomadu Bodou Lol Rogberi Lunsar Matotoka Rokel Bridge Masingbi Koundou Lungi Koidu-Sefadu Pepel Yengema li Njaiama- e SIERRA LEONE M Freetown o 8o 30' Masiaka Sewafe Njaiama 8 30' Goderich Wellington Gandorhun a Yonibana Mile 91 Tungie o Magbuntuso Makite Yele M Koindu Hastings Songo EASTERN Buedu WESTERN Waterloo Mongeri York Bradford Falla AREA Tongo Giehun Kailahun Tolobo ia Boajibu Rotifunk a T Taiama Panguma Manowa Banana Is. Yawri Moyamba Dambara Bay Njala Lago Bendu Pendembu 8o 00' Mano Mano 8o 00' Sembehun Bo Gerihun Jct. -
2006 Report on Electoral Constituency
August 2006 Preface This part of the report on Electoral Constituency Boundaries Delimitation process is a detailed description of each approved constituency. It comprises the chiefdoms, streets and other prominent features defining constituency boundaries. It is the aspect that deals with the legal framework for the approved constituencies. Ms. Christiana A. M. Thorpe (Dr.) Chief Electoral Commissioner and Chairperson. I Table of Contents Page A. Eastern Region…………………..……………………1 1. Kailahun District ……………………………………1 2. Kenema District………………………..……………5 3. Kono District……………………….………………14 B. Northern Region………………………..……………19 1. Bombali District………………….………..………19 2. Kambia District………………………..…..………25 3. Koinadugu District………………………….……31 4. Port Loko District……………………….…………34 5. Tonkolili District……………………………………43 C. Southern District……………………………………47 1. Bo District…………………………..………………47 2. Bonthe District………………………………………54 3. Moyamba District……………….…………………56 4. Pujehun District……………………………………60 D. Western Region………………………….……………64 1. Western Rural …………………….…………….....64 2. Western Urban ………………………………………81 II EASTERN REGION KAILAHUN DISTRICT (01) DESCRIPTION OF CONSTITUENCIES Name & Code Description of Constituency Kailahun District This constituency comprises of part of Luawa chiefdom with the Constituency 1 following sections: Baoma, Gbela, Luawa Foguiya, ManoSewallu, Mofindo, and Upper Kpombali. (NEC Const. 001) The constituency boundary starts along the Guinea/Sierra Leone international boundary northeast where the chiefdom boundaries of Kissi Kama and Luawa meet. It follows the Kissi Kama Luawa chiefdom boundary north and generally southeast to the meeting point of Kissi Kama, Luawa and Kissi Tongi chiefdoms. It continues along the Luawa/Kissi Tongi boundary south, east then south to meet the Guinea boundary on the southeastern boundary of Upper Kpombali section in Luawa chiefdom. It continues west wards along the international boundary to the southern boundary of Upper Kpombali section. -

Sierra Leone Environment, Conflict and Peacebuilding Assessment Technical Report
Sierra Leone Environment, Conflict and Peacebuilding Assessment Technical Report United Nations Environment Programme UNEP post-conflict environmental assessments Since 1999, UNEP has operated in more than 34 crisis-affected countries, published 18 environmental assessment reports and, in many cases, implemented in-country follow-up projects. Based on this expertise, UNEP is providing technical assistance to the UN Peacebuilding Commission (PBC), the European Commission and member states in assessing the role of natural resources and the environment in conflict and peacebuilding. The Sierra Leone Environment, Conflict and Peacebuilding Assessment was completed as part of UNEP’s Environmental Cooperation for Peacebuilding project, which offers technical assistance to Member States and the UN system to sustainably manage natural resources and the environment in ways that contribute to peacebuilding, conflict prevention and transboundary cooperation. Like other UNEP post-conflict assessments, this document is intended to provide practical analysis and recommendations to the Government of Sierra Leone, the UN and international community, and partner organizations regarding natural resources, peace and development. February 2010 © 2010 United Nations Environment Programme This publication may be reproduced in whole or in part and in any form for educational or non-profit purposes without special permission from the copyright holder provided acknowledgment of the source is made. UNEP would appreciate receiving a copy of any publication that uses this -
2017 Constituency Boundary Delimitation Report, Vol. 2
NATIONAL ELECTORAL COMMISSION Republic of Sierra Leone Constituency Boundary Delimitation Report Volume 2 August, 2017 Foreword The National Electoral Commission (NEC) is submitting this report on the delimitation of constituency and ward boundaries in adherence to its constitutional mandate to delimit electoral constituency and ward boundaries, to be done “not less than five years and not more than seven years”; and complying with the timeline as stipulated in the NEC Electoral Calendar (2015-2019). The report is subject to Parliamentary approval, as enshrined in the 1991 Constitution of Sierra Leone (Act No 6 of 1991); which inter alia states delimitation of electoral boundaries to be done by NEC, while Section 38 (1) empowers the Commission to divide the country into constituencies for the purpose of electing Members of Parliament (MPs) using Single Member First- Past –the Post (FPTP) system. The Local Government Act of 2004, Part 1 –preliminary, assigns the task of drawing wards to NEC; while the Public Elections Act, 2012 (Section 14, sub-sections 1 &2) forms the legal basis for the allocation of council seats and delimitation of wards in Sierra Leone. The Commission appreciates the level of technical assistance, collaboration and cooperation it received from Statistics Sierra Leone (SSL), the Boundary Delimitation Technical Committee (BDTC), the Boundary Delimitation Monitoring Committee (BDMC), donor partners, line Ministries, Departments and Agencies and other key actors in the boundary delimitation exercise. The hiring of a Consultant, Dr Lisa Handley, an internationally renowned Boundary delimitation expert, added credence and credibility to the process as she provided professional advice which assisted in maintaining international standards and best practices.