Report to the General Assembly
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Request for FTC Enforcement Regarding False COVID-19 Disease
July 21, 2020 VIA ELECTRONIC MAIL The Honorable Joseph J. Simons, Chairman The Honorable Rohit Chopra, Commissioner The Honorable Joshua Phillips, Commissioner The Honorable Rebecca Slaughter, Commissioner The Honorable Christine Wilson, Commissioner Federal Trade Commission 600 Pennsylvania Avenue NW Washington, DC 20580 Re: Request for Enforcement Regarding False COVID-19 Claims by Mercola Group Dear Chairman Simons and Commissioners Chopra, Phillips, Slaughter, and Wilson: Justice Catalyst Law (“JCL”),1 the Center for Science in the Public Interest (“CSPI”),2 and People’s Parity Project (“PPP”)3 write to urge the Federal Trade Commission (“FTC”) to bring enforcement proceedings against Joseph Mercola, D.O. (“Dr. Mercola”) and his companies (collectively, “Mercola Group”) for false, misleading, and deceptive claims and advertising of products they falsely claim will treat, cure, or prevent COVID-19 infections. We are also sending a similar letter to the U.S. Food and Drug Administration (“FDA”) today. As we set forth in detail below, Mercola Group has been capitalizing on the coronavirus pandemic by advising consumers to purchase vitamins, supplements, and other products sold on its website to prevent or treat the virus. Mercola Group’s website contains many misleading articles, such as “Nutrition and Natural Strategies Offer Hope Against COVID-19,”4 and a “Coronavirus Resource Guide” compiling various unsubstantiated claims about the COVID- fighting properties of various supplements.5 It also offers “medical” advice, including the extraordinarily dangerous and unsubstantiated recommendation that individuals actually try to contract COVID-19 after using the supplements it sells to ameliorate the symptoms.6 Mercola Group and Dr. Mercola make multiple deceptive and unsubstantiated claims in marketing supplements and other products. -

Owner's Manual
DYN-6210-02 / DYN-6310-02 2 Person and 3 Person Saunas OWNER’S MANUAL FOR CARBON MODEL SAUNAS FOR INDOOR USE ONLY DYN-6210-02 requires 120V 15 AMP DEDICATED CIRCUIT DYN-6310-02 requires 120V 20 AMP DEDICATED CIRCUIT Sauna: Now you can enjoy the European secret for youthful vitality. Carefully and thoroughly read this manual before using the sauna. We recommend keeping this manual for regular review and future reference. 1 WHAT ARE INFRARED RAYS? Infrared is the band of light we perceive as heat. We cannot see this band of light with the naked eye, but we can feel this type of light in the form of heat. Our sun produces most of its energy output in the infrared segment of the spectrum. Infrared rays heat your body without having to heat the air in-between. This process is called conversion. The infrared is divided into 3 segments by wavelengths measured in microns: near infrared: 0.76-1.5 microns; middle infrared: 1.5-5.6 microns; and far infrared: 5.6-1000 microns. Among these segments, only far infrared penetrates organic substances such as the human body two to three inches so that the warming effect is very uniform. ARE INFRARED RAYS SAFE? Because infrared rays are part of sunlight, they are not only safe but also highly beneficial to our bodies on a cellular level. Health professionals have used infrared heat lamps for decades to treat muscle and joint problems. In hospital baby care units, incubators are often equipped with infrared heating systems to keep newborn babies warm. -
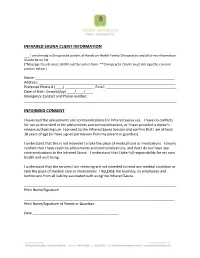
Infrared Sauna Consent Form
INFRARED SAUNA CLIENT INFORMATION ___ I am already a Chiropractic patient at Hands on Health Family Chiropractic and all of my information should be on file. (*Massage Clients must still fill out this entire form. **Chiropractic Clients must still sign the consent portion below.) Name: _______________________________________________________________________ Address: ______________________________________________________________________ Preferred Phone # (____) _______________ Email: ____________________________________ Date of Birth: (mm/dd/yy) ____/____/____ Emergency Contact and Phone number: ______________________________________________________________________________ INFORMED CONSENT I have read the advisements and contraindications for Infrared sauna use. I have no conflicts for use as described in the advisements and contraindications, or I have provided a doctor’s release authorizing use. I consent to the Infrared Sauna Session and confirm that I am at least 18 years of age (or have signed permission from my parent or guardian). I understand that this is not intended to take the place of medical care or medications. I clearly confirm that I have read the advisements and contraindications, and that I do not have any contraindications to the Infrared Sauna. I understand that I take full responsibility for my own health and well-being. I understand that the services I am receiving are not intended to treat any medical condition or take the place of medical care or medications. I RELEASE the business, its employees and technicians from all liability associated with using the Infrared Sauna. ______________________________________________________________________________ Print Name/Signature _____________________________________________________________________________ Print Name/Signature of Parent or Guardian Date ____________________________________________ ADVISEMENTS & CONTRAINDICATIONS Any of the below described contraindications will require you to use discretion for your own well being. -

Detoxification Protocol
Dr. Joel Cone/Dr. Alexis Dobson www.diagnosticnaturalmedicine.com (512) 577-7234 Detoxification Protocol Periodic detoxification makes sense in keeping your body as fine tuned and healthy as possible. We know many disease states, including heart disease, cancer, and chronic inflammatory disease states have a strong correlation with diet, lifestyle, and environmental factors. There are many different cleanse ideas, but if we start with the knowledge of the anatomy and physiology of the body we can make the best approach to a detoxification process possible. We know that there are several systems by which toxins and waste products are eliminated through the body. By having knowledge of these systems we can increase our ability to aggressively detoxify our body. There are four major detoxification systems our body uses. The first is the respiratory system which eliminates gaseous waste products such as carbon dioxide, a waste by product of glucose metabolism. Another system is the integumentary system, in which lactic acid and various other wastes are removed. We also use the digestive system, especially the hepatobiliary system to remove some cholesterol, bile secretions, and other toxins bound in bile. The liver is also the primary congugator of metabolic toxins into water soluble products which can be sent to the kidney for removal. The remaining system is the renal system, in which the kidney removed nitrogenous wastes, including urea, ammonia, creatinine, and other drug metabolites from the body. I have also added the lymphatic and circulatory system as an elimination component, as they play a crucial role in the mobilization of compounds that need to be removed from the body. -
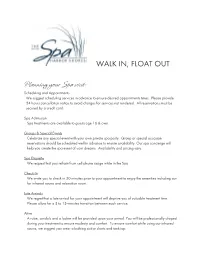
WALK IN, FLOAT out Planning Your Spa Visit
WALK IN, FLOAT OUT Planning your Spa visit: Scheduling and Appointments We suggest scheduling services in advance to ensure desired appointments times. Please provide 24 hours cancellation notice to avoid charges for services not rendered. All reservations must be secured by a credit card. Spa Admission Spa treatments are available to guests age 16 & over. Groups & Special Events Celebrate any special event with your own private spa party. Group or special occasion reservations should be scheduled well in advance to ensure availability. Our spa concierge will help you create the spa event of your dreams. Availability and pricing vary. Spa Etiquette We request that you refrain from cell phone usage while in the Spa. Check-In We invite you to check in 30 minutes prior to your appointment to enjoy the amenities including our far infrared sauna and relaxation room. Late Arrivals We regret that a late arrival for your appointment will deprive you of valuable treatment time. Please allow for a 5 to 15-minutes transition between each service. Attire A robe, sandals and a locker will be provided upon your arrival. You will be professionally draped during your treatment to ensure modesty and comfort. To ensure comfort while using our infrared sauna, we suggest you wear a bathing suit or shorts and tank top. Medical Please inform us of any medical or other special needs that require our attention. For your safety and well-being, we discourage alcohol consumption prior to your spa treatments, immediate sun exposure following skin care therapy and shaving after exfoliating treatments. Expectant mothers please bring doctor's permission for massage. -

Clinical Effects of Regular Dry Sauna Bathing: a Systematic Review
Hindawi Evidence-Based Complementary and Alternative Medicine Volume 2018, Article ID 1857413, 30 pages https://doi.org/10.1155/2018/1857413 Review Article Clinical Effects of Regular Dry Sauna Bathing: A Systematic Review Joy Hussain and Marc Cohen School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC, Australia Correspondence should be addressed to Joy Hussain; [email protected] Received 9 October 2017; Revised 14 December 2017; Accepted 8 January 2018; Published 24 April 2018 Academic Editor: Kieran Cooley Copyright © 2018 Joy Hussain and Marc Cohen. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Introduction. Many health benefts are claimed by individuals and facilities promoting sauna bathing; however the medical evidence to support these claims is not well established. Tis paper aims to systematically review recent research on the efects of repeated dry sauna interventions on human health. Methods. A systematic search was made of medical databases for studies reporting on the health efects of regular dry sauna bathing on humans from 2000 onwards. Risk of bias was assessed according to the Cochrane Collaboration guidelines. Results. Forty clinical studies involving a total of 3855 participants met the inclusion criteria. Only 13 studies were randomized controlled trials and most studies were small (� < 40). Reported outcome measures were heterogeneous with most studies reporting benefcial health efects. Only one small study (� = 10) reported an adverse health outcome of disrupted male spermatogenesis, demonstrated to be reversible when ceasing sauna activity. Conclusions. Regular dry sauna bathing has potential health benefts. -

Healing Power of Infrared Saunas
1 A Little History The health advantages of saunas are not a contemporary discovery. Historical confirmation and reports show that the Finns constructed the first wooden saunas over 2000 years ago. The primitive or first saunas were dug into a hill or mound. As tools and methods progressed, they were constructed above ground utilizing wooden logs. Rocks were heated in a stone fireplace with a wood fire. The smoke from the fire encompassed the room as the air warmed. As soon as the temperature reached preferred intensity, the smoke was permitted to clear and the patrons entered. The wood smoke scent still remained and was part of the healing ritual. This particular form of traditional smoke sauna was referred to as a savu, which translates into, “smoke” in Finnish. Sauna Evolution In time, the sauna developed where it utilized a metal woodstove, or kiuas (ke-wus), with a chimney. The temperature within the sauna was around 180 degrees Fahrenheit, but frequently surpassed 200 degrees in a traditional Finnish sauna. Steam vapor, also referred to as loyly (lou-lu), was generated by splashing water on the heated rocks. The steam and high heat triggered the users to perspire, therefore eliminating impurities and toxins from the body. In addition, the Finns also incorporated vihtas (veh-tas) or bunches of birch twigs to lightly smack the skin and generate further stimulation of the pores and cells. The Finnish culture also employed the sauna as a location to cleanse the mind, rejuvenate and refresh the spirit, and get ready the dead for burial. The sauna was a key part of their daily lives and families used it to bath together within the home. -

The Benefits of Infrared Sauna Therapy & Vibration Machine
The Benefits of Infrared Sauna Therapy & Vibration Machine (Must be 18 years of age or older to use the Sauna or Vibration Machine) Infrared saunas have proven very effective in reducing the stress response and creating balance in the autonomic nervous system. They improve circulation, help with weight loss, balance blood sugar, and improve detoxification—each of which improves your brain function. Infrared saunas have also been shown to reduce complications and improve cardiac performance in heart disease patients. Regular use of saunas has also been clinically shown to lower blood pressure with regular use, a key factor in heart health. Infrared saunas can also help your brain. In Dr. Mark Hyman book, The UltraMind Solution (www.drhyman.com), the health and resilience of your brain function are directly related to the complexity and variability of your heart rate. What is good for your heart is good for your brain. And since infrared saunas increase the variability and health of your nervous system, that means they are a great way to improve brain function. Saunas and sweat baths have been used by various cultures throughout history to flush out toxins and disease and maintain optimal physical and mental health. Saunas, and particularly infrared saunas, can also play a big role in preventing or reversing cancer. In a 2004 article in the Townsend Letter for Doctors and Patients, Lawrence Wilson, MD, wrote, “If I were to single out one method to combat cancer, it is the sauna. It assists removal of chemical toxins and heavy metals, increases oxygenation, enhances the immune system, and reduces the radiation burden in the body.” According to the National Cancer Institute, “Hyperthermia (also called thermal therapy or thermotherapy) is a type of cancer treatment in which body tissue is exposed to high temperatures. -

Downloads Hours/Contact Us
Calgary Chiropractor, Calgary NW, Airdrie, Cochrane AB: Infrared Sauna Page 1 of 2 HOME Meet Our Doctors Patient Care Team What To Expect Massage Therapy Naturopathic Medicine Services Forms/Downloads Hours/Contact Us PATIENT LOGIN Infrared Sauna All saunas are beneficial as sweating is one of the best ways to detoxify the body. The most comfortable and safest Search: GO sauna is the far-infrared sauna. The Today's Chiropractic heat from an infrared sauna penetrates 1.5-3 inches deep into the body to Why Patients See Us increase circulation, nourish damaged tissue and pull chemicals from fat Could Chiropractic Help You? storage directly into our sweat. What is True Health? Infrared sauna treatments are Chiropractic in 100 Words safe for people of all ages. Subluxation The infrared wavelength frequencies Adjustments stimulate our cells to vibrate which makes them permeable or leaky and Become a Patient promotes the purging of toxins out of "Getting Started" Video our cells, into circulation and out in our Free Newsletter Why X-rays? sweat. With the infrared sauna, a sweat volume 2-3 times higher than that of a Receive free professional For Skeptics Only regular sauna is achieved at a lower health tips on topics that Chiropractic Terms temperature. interest you. Practice Members Benefits of an infrared sauna: Name: Infrared sauna can aid in weight Email: Test Your Know How loss Select Topics: Take Our Stress Quiz A session in the infrared sauna can burn between 500 and 900 calories. Similar to Backaches & Sciatica Please Tell Others exercise, being in the infrared sauna increases your heart rate and metabolism and Headaches & Neck Pain uses a large amount of energy, while you just relax! The infrared sauna helps to Chiropractic Relief Strategies Wellness Topics decrease heavy metals, chemicals and pesticides in the body thereby helping to Diet & Nutrition Wellness Care Simplified correct metabolic imbalances that may be contributing to poor digestion and weight Exercise & Fitness "Making Choices" Video gain. -

Infrared Saunas in Regina Far Infrared Sauna Faqs
Dr. Julie Zepp Rutledge Doctor of Naturopathic Medicine www.drzepp.com Infrared Saunas in Regina Location Cost per session Session length A Balanced Approach $17 30 mins 2310 College Avenue 10 for $130 757-3200 Sugaring Oasis $15 45 mins 1856 Vic East Plaza 10 for $125 757-2221 20 for $200 60 mins Fit Zone $8 1818 Vic East 10 sessions for $60 757-9663 Chakari Spa $15 or free with a spa 45 mins (Sandman Inn) treatment Far Infrared Sauna FAQs Q: What is it? It’s a Low-Heat Sauna that operates at 40-50Celcius instead of 80-90 Celsius like a high-heat “regular” (finnish-style) dry sauna. Q: How does it work? It uses ceramic or carbon heaters which naturally penetrate your body very efficiently. It triggers your sweat glands to start functioning before your core body temperature goes up. That means you sweat profusely without feeling overly hot. Q: What are some of the benefits? Detoxification – removes stored toxins from the body Weight loss – up to 600 calories consumed in 30 minutes; and an increase in your daily resting total of 800 Heart health – stimulates gently the cardiovascular system supplying the conditioning benefits of continuous exercise 1 Dr. Julie Zepp Rutledge Doctor of Naturopathic Medicine www.drzepp.com Natural pain relief – for back pain, sprains, strains, bursitis, fibromyalgia, rheumatoid arthritis, headaches, etc. Relaxation and stress relief – balances the autonomic nervous system and hormones and reduce the negative impact of stress on the body Improved immune function – stimulates and strengthens your body’s immune system Improved skin conditions and helps treat cellulite – relieves acne, psoriasis, burns, eczema, and removes roughness and scarring Boost mood and helps fight SAD Q: What is the Far Infrared part? Far Infrared is simply the band of the light spectrum - Infrared means “Below Red” or just under the visible light part of the spectrum. -

Spa Packages
WELCOME The Spa at Naples Grande provides a Quiet Environment variety of services focused on overall health enrichment through our modern and We strive to provide a tranquil and private innovative offerings. Your mind will relax, escape. As a courtesy to you and the rest of body rejuvenate, and soul be transformed. our guests we ask that you turn off your cell A Grande spa experience awaits. phones, electronic devices and cameras upon entering the spa. Arrival SPA PACKAGES Gratuities We invite you to enjoy the spa amenities on the day of any confirmed spa treatment and For your convenience, a 22% service charge is added to all spa and salon treatments. ask that you arrive at least 30 minutes in Spa Essentials | 2 Hours | $295 advance to allow proper time for checking in, Additional gratuities are at your discretion showering and enjoying spa amenities. and may be added upon request. Escape and indulge in our unique treatments to reduce stress and tension, while These amenities include our labyrinth, sun restoring peace and tranquility. This package includes your choice of any two deck, whirlpool, sauna, steam room and Cancellation & Rescheduling 50-minute Spa Services. meditation lounge. Your treatment will As a courtesy to you, other guests and start at its scheduled time and arriving late | 3 Hours | $440 service providers, we strictly adhere to Golden Trio will limit the time that you can enjoy your the spa cancellation policy: If you must Remove, restore, and radiate. Begin your experience with a 50-minute service. Should you like to enjoy these reschedule or cancel an appointment, Signature Muscle Melt Massage to relax, followed by a 50-minute amenities without booking a treatment please advise us eight (8) hours in advance Fijian Coconut Scrub to gently exfoliate your skin, and conclude with there is a separate charge based on daily to avoid being charged 100% of the availability. -

Crystal Dove, Inc
MAY / JUNE 2014 3 Classes and Workshops 23 Living in Sufficiency Workshop: --------------------------------------------------------------- Transform Your Relationship to 4 Community Events Money and Life --------------------------------------------------------------- --------------------------------------------------------------- 7 From the Publisher 24 Big Versus Small Healthcare --------------------------------------------------------------- by Colleen von Kittel 8 Sowing COlOP Seeds: Co-ops --------------------------------------------------------------- Are you longing for your life Supporting Other Co-ops 25 Who Has Your Back? to be easier and more fun? --------------------------------------------------------------- by Inga Madsen Would you like to stop pushing, 9 Cannabidiols (CBD): Is it for Me? --------------------------------------------------------------- micromanaging, and forcing by Sunil Pai, MD 25 MyoRehab Has Moved things to happen so you can --------------------------------------------------------------- by Victoria L. Magown 10 Awakening Abundance Now! --------------------------------------------------------------- relax? What if you could stop Brain–Heart–Soul Balancing 26 Designing Our Lives with worrying about money and live by Louise Swartswalter, ND, CBS, CNHP Mother Earth Divine with more emotional ease at --------------------------------------------------------------- by Phaeryn Sheehan the moment? 11 Planting with Intention --------------------------------------------------------------- by Rhonda Owen 27 Local