Trimethoprim and Other Nonclassical Antifolates an Excellent Template for Searching Modifications of Dihydrofolate Reductase
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of Nanobiosensors in Therapeutic Drug Monitoring
Journal of Personalized Medicine Review Personalized Medicine for Antibiotics: The Role of Nanobiosensors in Therapeutic Drug Monitoring Vivian Garzón 1, Rosa-Helena Bustos 2 and Daniel G. Pinacho 2,* 1 PhD Biosciences Program, Universidad de La Sabana, Chía 140013, Colombia; [email protected] 2 Therapeutical Evidence Group, Clinical Pharmacology, Universidad de La Sabana, Chía 140013, Colombia; [email protected] * Correspondence: [email protected]; Tel.: +57-1-8615555 (ext. 23309) Received: 21 August 2020; Accepted: 7 September 2020; Published: 25 September 2020 Abstract: Due to the high bacterial resistance to antibiotics (AB), it has become necessary to adjust the dose aimed at personalized medicine by means of therapeutic drug monitoring (TDM). TDM is a fundamental tool for measuring the concentration of drugs that have a limited or highly toxic dose in different body fluids, such as blood, plasma, serum, and urine, among others. Using different techniques that allow for the pharmacokinetic (PK) and pharmacodynamic (PD) analysis of the drug, TDM can reduce the risks inherent in treatment. Among these techniques, nanotechnology focused on biosensors, which are relevant due to their versatility, sensitivity, specificity, and low cost. They provide results in real time, using an element for biological recognition coupled to a signal transducer. This review describes recent advances in the quantification of AB using biosensors with a focus on TDM as a fundamental aspect of personalized medicine. Keywords: biosensors; therapeutic drug monitoring (TDM), antibiotic; personalized medicine 1. Introduction The discovery of antibiotics (AB) ushered in a new era of progress in controlling bacterial infections in human health, agriculture, and livestock [1] However, the use of AB has been challenged due to the appearance of multi-resistant bacteria (MDR), which have increased significantly in recent years due to AB mismanagement and have become a global public health problem [2]. -
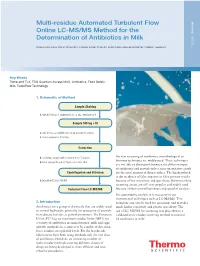
Multi-Residue Automated Turbulent Flow Online LC-MS/MS Method for the Determination of Antibiotics in Milk
Multi-residue Automated Turbulent Flow 63551 Method: Online LC-MS/MS Method for the Determination of Antibiotics in Milk Katerina Bousova, Klaus Mittendorf, Thermo Fisher Scientific Food Safety Response Center, Dreieich, Germany Key Words Transcend TLX, TSQ Quantum Access MAX, Antibiotics, Food Safety, Milk, TurboFlow Technology 1. Schematic of Method Sample Shaking 1. Weigh 500 mg of shaken milk into 2 mL centrifuge tube Sample 500 mg + IS 2. Add 450 µL acetonitrile and 50 µL working IS solution 3. Vortex sample for 5 minutes Extraction 4. Centrifuge sample with 12,000 rpm for 5 minutes For fast screening of antibiotics, microbiological or bioassay techniques are widely used. These techniques 5. Filter sample through 0.45 µm nylon microfilter are not able to distinguish between the different types of antibiotics and provide only a semi-quantitative result Centrifugation and Filtration for the total amount of drug residues. The big drawback is the incidence of false-negative or false-positive results 6. Inject into TLX-LC-MS/MS because of low sensitivity and specificity. However, these screening assays are still very popular and widely used Turbulent Flow LC-MS/MS because of their cost-effectiveness and speed of analysis. For quantitative analysis it is necessary to use instrumental techniques such as LC-MS/MS. This 2. Introduction technique can also be used for screening, and provides Antibiotics are a group of chemicals that are widely used much higher sensitivity and greater specificity. The in animal husbandry primarily for protection of animals use of LC-MS/MS for screening was described in a from disease but also as growth promoters. -

Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications
International Journal of Molecular Sciences Review Folic Acid Antagonists: Antimicrobial and Immunomodulating Mechanisms and Applications Daniel Fernández-Villa 1, Maria Rosa Aguilar 1,2 and Luis Rojo 1,2,* 1 Instituto de Ciencia y Tecnología de Polímeros, Consejo Superior de Investigaciones Científicas, CSIC, 28006 Madrid, Spain; [email protected] (D.F.-V.); [email protected] (M.R.A.) 2 Consorcio Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, 28029 Madrid, Spain * Correspondence: [email protected]; Tel.: +34-915-622-900 Received: 18 September 2019; Accepted: 7 October 2019; Published: 9 October 2019 Abstract: Bacterial, protozoan and other microbial infections share an accelerated metabolic rate. In order to ensure a proper functioning of cell replication and proteins and nucleic acids synthesis processes, folate metabolism rate is also increased in these cases. For this reason, folic acid antagonists have been used since their discovery to treat different kinds of microbial infections, taking advantage of this metabolic difference when compared with human cells. However, resistances to these compounds have emerged since then and only combined therapies are currently used in clinic. In addition, some of these compounds have been found to have an immunomodulatory behavior that allows clinicians using them as anti-inflammatory or immunosuppressive drugs. Therefore, the aim of this review is to provide an updated state-of-the-art on the use of antifolates as antibacterial and immunomodulating agents in the clinical setting, as well as to present their action mechanisms and currently investigated biomedical applications. Keywords: folic acid antagonists; antifolates; antibiotics; antibacterials; immunomodulation; sulfonamides; antimalarial 1. -

Pyrimethamine
Canterbury District Health Board Neonatal Services PYRIMETHAMINE Trade Name Daraprim (GlaxoSmithKlyne) Class Antiparasitic/antimalarial agent Mechanism of Action Inhibits parasitic dihydrofolate reductase resulting in inhibition of tetrahydrofolic acid synthesis Indications Congenital toxoplasmosis (Used in combination with sulfadiazine) Contraindications Known megaloblastic anaemia Supplied As Pyrimethamine suspension 1mg/mL (prepared by pharmacy) Dilution None required Dosage 1mg/kg/dose If the patient has difficulty tolerating pyrimathamine give each dose with a feed to reduce the incidence of vomiting Interval Once daily for the first 6 months, then Three times a week for the second 6 months Administration Oral Compatible With N/A Incompatible With N/A Interactions Pyrimethamine reduces the anti-epileptic effect of phenytoin Antifolate effects are increased when pyrimethamine is given in combination with sulphonamides, trimethoprim, zidovudine or methotrexate. Folic Acid may reduce the anti-parasitic effect of pyrimethamine and also increase the risk of pyrimethamine induced bone marrow suppression , for these reasons folinic acid is used to counteract the antifolate effect of pyrimethamine. Avoid brands of sunblock that contain PABA as this may reduce the effectiveness of sulfadiazine. Monitoring Full blood count Stability 30 days at 2 – 8 oC Storage In the fridge Adverse Reactions Skin rash (including Stevens Johnson Syndrome), nausea, vomiting, diarrhoea, blood dyscrasias, raised AST, sensory neuropathy Metabolism 15-40% metabolised by liver, approx 60% of dose excreted as Pyrimethamine Printed copies are not controlled and may not be the current version in use Ref.236799 Authorised by: Clinical Director Neonatal Page 1 of 2 March 2016 Canterbury District Health Board Neonatal Services unchanged drug by kidneys. -

A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre
A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sebastien Lefebvre To cite this version: Tessa Trouchon, Sebastien Lefebvre. A Review of Enrofloxacin for Veterinary Use. Open Journal of Veterinary Medicine, 2016, 6 (2), pp.40-58. 10.4236/ojvm.2016.62006. hal-01503397 HAL Id: hal-01503397 https://hal.archives-ouvertes.fr/hal-01503397 Submitted on 7 Apr 2017 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution - NoDerivatives| 4.0 International License Open Journal of Veterinary Medicine, 2016, 6, 40-58 Published Online February 2016 in SciRes. http://www.scirp.org/journal/ojvm http://dx.doi.org/10.4236/ojvm.2016.62006 A Review of Enrofloxacin for Veterinary Use Tessa Trouchon, Sébastien Lefebvre USC 1233 INRA-Vetagro Sup, Veterinary School of Lyon, Marcy l’Etoile, France Received 12 January 2016; accepted 21 February 2016; published 26 February 2016 Copyright © 2016 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract This review outlines the current knowledge on the use of enrofloxacin in veterinary medicine from biochemical mechanisms to the use in the field conditions and even resistance and ecotoxic- ity. -

9-20-08 Referral
Comparative studies with antibiotics: Why should we change the rules? Paul M. Tulkens, MD, PhD Cellular and Molecular Pharmacology & Centre for Clinical Pharmacy Louvain Drug Research Institute, Université catholique de Louvain, Brussels, Belgium 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 1 What its all about ? • We are in real need of novel antibiotics… but … most clinical studies with new compounds aim at equivalence or non-inferiority, failing to meet clinicians’ expectations and regulatory requirements for novelty. In parallel, safety issues are becoming an increasingly worrying hurdle for manufacturers Pricing make antibiotic unattractive • What are the possible solutions ? 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 2 The antibiotic crisis * * A pictorial view using 4 paintings of Van Gogh (who stayed briefly in Belgium when moving from Holland to France) and with selected Belgian and International data… 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 3 Are antibiotics following a path to madness ? discovery in soil bacteria and fungi 1928 - … 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 4 Are antibiotics following a path to madness ? and then we all saw the blooming tree of semi- synthetic and totally synthetic antibiotics 1950 – 1980 … 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 5 Are antibiotics following a path to madness ? and the US General Surgeon told us that the fight was over 1970 … 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 6 Are antibiotics following a path to madness ? But… 2012 … 10-10-2012 Late Phase Leaders Forum, Vienna, Austria 7 Extent of resistance of P. -

An Updated Review of Iclaprim
Open Forum Infectious Diseases REVIEW ARTICLE An Updated Review of Iclaprim: A Potent and Rapidly Bactericidal Antibiotic for the Treatment of Skin and Skin Structure Infections and Nosocomial Pneumonia Caused by Gram-Positive Including Multidrug-Resistant Bacteria David B. Huang,1 Catherine D. Strader,3 James S. MacDonald,3 Mark VanArendonk,2 Richard Peck,4 and Thomas Holland5 1Motif BioSciences, New York, New York; Rutgers New Jersey Medical School, 2Vermeer Pharma, Morristown, New Jersey, 3Synergy Partners R&D Solutions, Chester, New Jersey; 4Hemex, Liestal, Switzerland, 5Duke University Medical Center, Durham, North Carolina New antibiotics are needed because of the increased morbidity and mortality associated with multidrug-resistant bacteria. Iclaprim, a bacterial dihydrofolate reductase inhibitor, not currently approved, is being studied for the treatment of skin infections and noso- comial pneumonia caused by Gram-positve bacteria, including multidrug-resistant bacteria. Iclaprim showed noninferiority at –10% to linezolid in 1 of 2 phase 3 studies for the treatment of complicated skin and skin structure infections with a weight-based dose (0.8 mg/kg) but did not show noninferiority at –10% to linezolid in a second phase 3 study. More recently, iclaprim has shown noninferiority at –10% to vancomycin in 2 phase 3 studies for the treatment of acute bacterial skin and skin structure infections with an optimized fixed dose (80 mg). A phase 3 study for the treatment of hospital-acquired bacterial and ventilator-associated bacterial pneumonia is upcoming. If, as anticipated, iclaprim becomes available for the treatment of skin and skin structure infections, it will serve as an alternative to current antibiotics for treatment of severe infections. -

Antibiotic Use Guidelines for Companion Animal Practice (2Nd Edition) Iii
ii Antibiotic Use Guidelines for Companion Animal Practice (2nd edition) iii Antibiotic Use Guidelines for Companion Animal Practice, 2nd edition Publisher: Companion Animal Group, Danish Veterinary Association, Peter Bangs Vej 30, 2000 Frederiksberg Authors of the guidelines: Lisbeth Rem Jessen (University of Copenhagen) Peter Damborg (University of Copenhagen) Anette Spohr (Evidensia Faxe Animal Hospital) Sandra Goericke-Pesch (University of Veterinary Medicine, Hannover) Rebecca Langhorn (University of Copenhagen) Geoffrey Houser (University of Copenhagen) Jakob Willesen (University of Copenhagen) Mette Schjærff (University of Copenhagen) Thomas Eriksen (University of Copenhagen) Tina Møller Sørensen (University of Copenhagen) Vibeke Frøkjær Jensen (DTU-VET) Flemming Obling (Greve) Luca Guardabassi (University of Copenhagen) Reproduction of extracts from these guidelines is only permitted in accordance with the agreement between the Ministry of Education and Copy-Dan. Danish copyright law restricts all other use without written permission of the publisher. Exception is granted for short excerpts for review purposes. iv Foreword The first edition of the Antibiotic Use Guidelines for Companion Animal Practice was published in autumn of 2012. The aim of the guidelines was to prevent increased antibiotic resistance. A questionnaire circulated to Danish veterinarians in 2015 (Jessen et al., DVT 10, 2016) indicated that the guidelines were well received, and particularly that active users had followed the recommendations. Despite a positive reception and the results of this survey, the actual quantity of antibiotics used is probably a better indicator of the effect of the first guidelines. Chapter two of these updated guidelines therefore details the pattern of developments in antibiotic use, as reported in DANMAP 2016 (www.danmap.org). -

Transdermal Drug Delivery Device Including An
(19) TZZ_ZZ¥¥_T (11) EP 1 807 033 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61F 13/02 (2006.01) A61L 15/16 (2006.01) 20.07.2016 Bulletin 2016/29 (86) International application number: (21) Application number: 05815555.7 PCT/US2005/035806 (22) Date of filing: 07.10.2005 (87) International publication number: WO 2006/044206 (27.04.2006 Gazette 2006/17) (54) TRANSDERMAL DRUG DELIVERY DEVICE INCLUDING AN OCCLUSIVE BACKING VORRICHTUNG ZUR TRANSDERMALEN VERABREICHUNG VON ARZNEIMITTELN EINSCHLIESSLICH EINER VERSTOPFUNGSSICHERUNG DISPOSITIF D’ADMINISTRATION TRANSDERMIQUE DE MEDICAMENTS AVEC COUCHE SUPPORT OCCLUSIVE (84) Designated Contracting States: • MANTELLE, Juan AT BE BG CH CY CZ DE DK EE ES FI FR GB GR Miami, FL 33186 (US) HU IE IS IT LI LT LU LV MC NL PL PT RO SE SI • NGUYEN, Viet SK TR Miami, FL 33176 (US) (30) Priority: 08.10.2004 US 616861 P (74) Representative: Awapatent AB P.O. Box 5117 (43) Date of publication of application: 200 71 Malmö (SE) 18.07.2007 Bulletin 2007/29 (56) References cited: (73) Proprietor: NOVEN PHARMACEUTICALS, INC. WO-A-02/36103 WO-A-97/23205 Miami, FL 33186 (US) WO-A-2005/046600 WO-A-2006/028863 US-A- 4 994 278 US-A- 4 994 278 (72) Inventors: US-A- 5 246 705 US-A- 5 474 783 • KANIOS, David US-A- 5 474 783 US-A1- 2001 051 180 Miami, FL 33196 (US) US-A1- 2002 128 345 US-A1- 2006 034 905 Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Section 5: Enzymes, Equilibrium, Energy and the Metabolic Inhibitors
Small World Initiative Instructor Guide Section 5: Enzymes, Equilibrium, Energy and the Metabolic Inhibitors Section 5: Enzymes, Equilibrium, Energy and the Metabolic Inhibitors TOPICS Enzyme kinetics Binding equilibrium Free energy Metabolic reactions/energy production Molecular binding specificity Mechanism of action of metabolic inhibitors SUMMARY We continue our investigation of antibiotic specificity by introducing the metabolic inhibitors. The two different classes of metabolic inhibitors use two different mechanisms to achieve specificity. Like the β-lactams, the sulfonamides achieve specificity by binding to and inhibiting a target molecule not present in eukaryotes. In contrast, trimethoprim is representative of those antibiotics that target a specific region of a molecule present in both prokaryotes and eukaryotes. The subtle structural difference between the prokaryotic and eukaryotic version of the target is such that binding affinity of the antibiotic to the eukaryotic version is reduced relative to the prokaryotic version. We use the metabolic inhibitors as a context for discussing enzyme kinetics and energy. Instructors may also wish to include the key conserved metabolic pathways (glycolysis, tricarboxylic acid cycle, oxidative phosphorylation) as well as highlighting the metabolic diversity of the prokaryotes, although that content is not represented in the slides. LEARNING GOALS • Be able to explain the mechanism of action of metabolic inhibitors at the molecular level • Know the factors that determine rates of chemical reactions. • Know the factors that determine equilibrium of chemical reactions. • Explain how enzymes achieve substrate specificity • Describe the molecular basis for antibiotic-target “binding” (covalent, non- covalent bond formation) • Explain binding equilibrium as it pertains to antibiotic-target binding (and how it affects efficacy of an antibiotic) • Describe how metabolic inhibitors achieve prokaryotic specificity. -

Antimicrobial Resistance in Fecal Escherichia Coli and Salmonella
Varga et al. BMC Veterinary Research (2019) 15:464 https://doi.org/10.1186/s12917-019-2187-z RESEARCH ARTICLE Open Access Antimicrobial resistance in fecal Escherichia coli and Salmonella enterica isolates: a two- year prospective study of small poultry flocks in Ontario, Canada Csaba Varga1* , Michele T. Guerin2, Marina L. Brash3, Durda Slavic3, Patrick Boerlin4 and Leonardo Susta4 Abstract Background: Although keeping small poultry flocks is increasingly popular in Ontario, information on the antimicrobial susceptibility of enteric bacteria of such flocks is lacking. The current study was conducted on small poultry flocks in Ontario between October 2015 and September 2017, and samples were submitted on a voluntary basis to Ontario’s Animal Health Laboratory. From each submission, a pooled cecal sample was obtained from all the birds of the same species from the same flock and tested for the presence of two common enteric pathogens, E. coli and Salmonella. Three different isolates from each E. coli-positive sample and one isolate from each Salmonella- positive sample were selected and tested for susceptibility to 14 antimicrobials using a broth microdilution technique. Results: A total of 433 fecal E. coli isolates (358 chicken, 27 turkey, 24 duck, and 24 game bird) and 5 Salmonella isolates (3 chicken, 1 turkey, and 1 duck) were recovered. One hundred and sixty-seven chicken, 5 turkey, 14 duck, and 15 game bird E. coli isolates were pan-susceptible. For E. coli, a moderate to high proportion of isolates were resistant to tetracycline (43% chicken, 81% turkey, 42% duck, and 38% game bird isolates), streptomycin (29% chicken, 37% turkey, and 33% game bird isolates), sulfonamides (17% chicken, 37% turkey, and 21% duck isolates), and ampicillin (16% chicken and 41% turkey isolates). -

Session Ii. Test Models for the Effective Control of Chemotherapy Free Communication
SESSION II. TEST MODELS FOR THE EFFECTIVE CONTROL OF CHEMOTHERAPY FREE COMMUNICATION Chairman A M DHOPLE (USA) Lepr Rev (1986) 57, Supplement 3, 137-148 The use of rodent models in assessing antimicrobial activity against My cobacterium /eprae R H GELBER Seton Medical Center, Sullivan Avenue, Daly City, CA USA 1900 94015, Prior to the landmark discovery in 1960 of ' The Experimental disease that follows the injection of human leprosy bacilli into footpads of mice,' 1 the only means of searching for drugs active against human disease was to conduct clinical trials. Because clinical improvement of lepromatous patients is both very slow and variable, because the number of AFB (BI) in the skin falls extraordinarily slowly despite adequate therapy, and because the viability of solid-staining bacilli (MI) was not appreciated, early short-term clinical trials were difficultto conduct and the results even harder to interpret. Of the earlier studies on dapsone only the study of Lowe2 followed a stable population until bacteriological negativity, finding32 of 39 (83%) negative at 5 years, 31 of35 (89%) negative at 6 years, and 34 of 35 (97%) smear-negative at 7 years. The earliest studies on the effect of antimicrobial agents on My cobacterium leprae- infected mice utilized primarily drugs known to be effective against M. tuberculosis. These first studies utilized constant treatment from the time of mouse fo otpad infection, generally with 5 x 103 M. lepraejfootpad, either by incorporation of drug into mouse chow or daily (actually usually five times weekly) intraperitoneal injections. By these means Shepard3 found dapsone, clofazimine, isoniazid, para-aminosalicylic acid, streptomycin, and cycloserine active and ethambutal and pyrizinamide inactive.