Federal Register/Vol. 85, No. 232/Wednesday, December 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Copy of 2020-2021 Semi-Monthly Calendar.Xlsx
Employee Time Sheet/Leave Sheet Schedule Supervisor Approval Deadline/ Pay Period Employee Submittal Deadline Paper Leave Request Due to HR by 11:59 PM 12 Noon Pay Day Wednesday, July 1, 2020 to Wednesday, July 15, 2020 Thursday, July 16, 2020 Friday, July 17, 2020 Friday, July 31, 2020 Thursday, July 16, 2020 to Friday, July 31, 2020 Monday, August 3, 2020 Tuesday, August 4, 2020 Friday, August 14, 2020 Saturday, August 1, 2020 to Saturday, August 15, 2020 Monday, August 17, 2020 Tuesday, August 18, 2020 Monday, August 31, 2020 Sunday, August 16, 2020 to Monday, August 31, 2020 Tuesday, September 1, 2020 Wednesday, September 2, 2020 Tuesday, September 15, 2020 Tuesday, September 1, 2020 to Tuesday, September 15, 2020 Wednesday, September 16, 2020 Thursday, September 17, 2020 Wednesday, September 30, 2020 Wednesday, September 16, 2020 to Wednesday, September 30, 2020 Thursday, October 1, 2020 Friday, October 2, 2020 Thursday, October 15, 2020 Thursday, October 1, 2020 to Thursday, October 15, 2020 Friday, October 16, 2020 Monday, October 19, 2020 Friday, October 30, 2020 Friday, October 16, 2020 to Saturday, October 31, 2020 Monday, November 2, 2020 Tuesday, November 3, 2020 Friday, November 13, 2020 Sunday, November 1, 2020 to Sunday, November 15, 2020 Monday, November 16, 2020 Tuesday, November 17, 2020 Monday, November 30, 2020 Monday, November 16, 2020 to Monday, November 30, 2020 Tuesday, December 1, 2020 Wednesday, December 2, 2020 Tuesday, December 15, 2020 Tuesday, December 1, 2020 to Tuesday, December 15, 2020 Wednesday, December -

Peoria Unified School District 6-Day Rotation Schedule
Peoria Unified School District 2020 – 2021 School Year Six-Day Rotation Schedule August 2020 January 2021 Day 1: August 17, 19 AM, 26 PM and 27 Day 1: January 6 PM, 11 and 22 Day 2: August 18 and 28 Day 2: January 12, 13 AM, 20 PM and 25 Day 3: August 23 and 31 Day 3: January 4, 14, 26 and 27 AM Day 4: August 21 Day 4: January 5, 15 and 28 Day 5: August 24 Day 5: January 7, 19 and 29 Day 6: August 25 Day 6: January 8 and 21 September 2020 February 2021 Day 1: September 8, 18 and 29 Day 1: February 2, 12 and 25 Day 2: September 2 AM, 9 PM, and 21 Day 2: February 4, 16 and 26 Day 3: September 11, 16 AM and 23 PM Day 3: February 3 PM, 5 and 18 Day 4: September 1, 14, 24 and 30 AM Day 4: February 8, 10 AM, 17 PM and 19 Day 5: September 3, 15 and 25 Day 5: February 9, 22 and 24 AM Day 6: September 4, 17 and 28 Day 6: February 1, 11 and 23 October 2020 March 2021 Day 1: October 9 and 22 Day 1: March 8, 25 and 31 AM Day 2: October 1, 13 and 23 Day 2: March 9 and 26 Day 3: October 2, 15 and 26 Day 3: March 1, 11 and 29 Day 4: October 5, 7 PM, 16 and 27 Day 4: March 2, 12 and 30 Day 5: October 6, 14 AM, 21 PM and 29 Day 5: March 3 PM, 4 and 22 Day 6: October 8, 20, 28 AM and 30 Day 6: March 5, 10 AM, 23 and 24 PM November 2020 April 2021 Day 1: November 2, 12 and 20 Day 1: April 5, 7 PM, 15 and 27 Day 2: November 3, 13 and 30 Day 2: April 6, 14 AM, 16, 21 PM and 29 Day 3: November 5 and 16 Day 3: April 8, 19, 28 AM and 30 Day 4: November 6 and 17 Day 4: April 9 and 20 Day 5: November 9 and 18 Day 5: April 1, 12 and 22 Day 6: November 4 PM, 10 and 19 Day 6: April 2, 13 and 26 December 2020 May 2021 Day 1: December 7, 15 and 16 AM Day 1: May 7 and 18 Day 2: December 8 and 17 Day 2: May 10 and 19 Day 3: December 1 and 9 Day 3: May 5 PM, 11 and 20 Day 4: December 2 and 10 Day 4: May 3, 12 AM, 13 Day 5: December 3 and 11 Day 5: May 4 and 14 Day 6: December 4 and 14 Day 6: May 6 and 17 EARLY RELEASE or MODIFIED WEDNESDAY • Elementary schools starting at 8 a.m. -

2021 7 Day Working Days Calendar
2021 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Friday, January 1, 2021 133 Saturday, January 2, 2021 134 Sunday, January 3, 2021 135 Monday, January 4, 2021 136 Tuesday, January 5, 2021 137 Wednesday, January 6, 2021 138 Thursday, January 7, 2021 139 Friday, January 8, 2021 140 Saturday, January 9, 2021 141 Sunday, January 10, 2021 142 Monday, January 11, 2021 143 Tuesday, January 12, 2021 144 Wednesday, January 13, 2021 145 Thursday, January 14, 2021 146 Friday, January 15, 2021 147 Saturday, January 16, 2021 148 Sunday, January 17, 2021 149 Monday, January 18, 2021 150 Tuesday, January 19, 2021 151 Wednesday, January 20, 2021 152 Thursday, January 21, 2021 153 Friday, January 22, 2021 154 Saturday, January 23, 2021 155 Sunday, January 24, 2021 156 Monday, January 25, 2021 157 Tuesday, January 26, 2021 158 Wednesday, January 27, 2021 159 Thursday, January 28, 2021 160 Friday, January 29, 2021 161 Saturday, January 30, 2021 162 Sunday, January 31, 2021 163 Monday, February 1, 2021 164 Tuesday, February 2, 2021 165 Wednesday, February 3, 2021 166 Thursday, February 4, 2021 167 Date Number of the Calendar Date Friday, February 5, 2021 168 Saturday, February 6, 2021 169 Sunday, February -
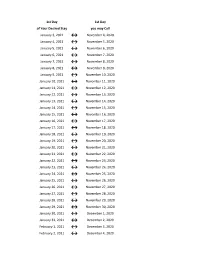
Flex Dates.Xlsx
1st Day 1st Day of Your Desired Stay you may Call January 3, 2021 ↔ November 4, 2020 January 4, 2021 ↔ November 5, 2020 January 5, 2021 ↔ November 6, 2020 January 6, 2021 ↔ November 7, 2020 January 7, 2021 ↔ November 8, 2020 January 8, 2021 ↔ November 9, 2020 January 9, 2021 ↔ November 10, 2020 January 10, 2021 ↔ November 11, 2020 January 11, 2021 ↔ November 12, 2020 January 12, 2021 ↔ November 13, 2020 January 13, 2021 ↔ November 14, 2020 January 14, 2021 ↔ November 15, 2020 January 15, 2021 ↔ November 16, 2020 January 16, 2021 ↔ November 17, 2020 January 17, 2021 ↔ November 18, 2020 January 18, 2021 ↔ November 19, 2020 January 19, 2021 ↔ November 20, 2020 January 20, 2021 ↔ November 21, 2020 January 21, 2021 ↔ November 22, 2020 January 22, 2021 ↔ November 23, 2020 January 23, 2021 ↔ November 24, 2020 January 24, 2021 ↔ November 25, 2020 January 25, 2021 ↔ November 26, 2020 January 26, 2021 ↔ November 27, 2020 January 27, 2021 ↔ November 28, 2020 January 28, 2021 ↔ November 29, 2020 January 29, 2021 ↔ November 30, 2020 January 30, 2021 ↔ December 1, 2020 January 31, 2021 ↔ December 2, 2020 February 1, 2021 ↔ December 3, 2020 February 2, 2021 ↔ December 4, 2020 1st Day 1st Day of Your Desired Stay you may Call February 3, 2021 ↔ December 5, 2020 February 4, 2021 ↔ December 6, 2020 February 5, 2021 ↔ December 7, 2020 February 6, 2021 ↔ December 8, 2020 February 7, 2021 ↔ December 9, 2020 February 8, 2021 ↔ December 10, 2020 February 9, 2021 ↔ December 11, 2020 February 10, 2021 ↔ December 12, 2020 February 11, 2021 ↔ December 13, 2020 -

2020-2021 Academic Calendar Revised 9.18.20
FRANCISCAN UNIVERSITY OF STEUBENVILLE 2020-2021 ACADEMIC CALENDAR REVISED 9.18.20 FALL 2020 SEMESTER SPRING 2021 SEMESTER August 24 25-December 11 January 11-May 5 New Student Orientation August 20-23 (Thurs-Sun) January 7-10 (Thurs-Sun) Convocation & Opening of School Mass August 24 (Mon) (4 pm; 3 pm classes January 11 (Mon) (mass only, 10:30 am) shortened & 4:30 pm classes cancelled) Classes begin August 24 (Mon) January 11 (Mon) (10 a.m. classes shortened) Last day for late registration August 28 (Fri) January 15 (Fri) Last day for adding/dropping courses September 2 (Wed) January 20 (Wed) Labor Day (class day) September 7 (Mon) (class day) N/A March for Life N/A January 29 (no day classes) Last day for audit changes September 11 (Fri) January 22 (Fri) Incomplete grades due to registrar September 25 (Fri) February 12 (Fri) Feast of St. Francis October 4 (Sun) N/A Homecoming weekend October 2-4 (Fri-Sun) N/A Midterm deficiencies due to registrar October 14 (Wed) March 5 (Fri) Spring Break N/A March 8-12 (Mon-Fri) (classes resume Mon, March 15) Last day for course withdrawal November 2 (Mon) March 26 (Fri) Tentative Class Make-up Days November 14, 21 (Sat) Thanksgiving vacation November 25-29 (Wed-Sun) N/A (classes resume Mon, Nov 30) Holy Thursday April 1 (no evening classes) Easter recess (Friday & Monday day classes N/A April 2-April 5 (day) canceled; *Monday evening classes do meet) (classes resume Mon evening, April 5, Tuesday day, April 6) Classes Resume Evening: Mon, April 5; Day: Tues, April 6 Last day of classes December 1 (Tues) -
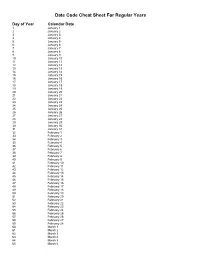
Julian Date Cheat Sheet for Regular Years
Date Code Cheat Sheet For Regular Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 March 1 61 March 2 62 March 3 63 March 4 64 March 5 65 March 6 66 March 7 67 March 8 68 March 9 69 March 10 70 March 11 71 March 12 72 March 13 73 March 14 74 March 15 75 March 16 76 March 17 77 March 18 78 March 19 79 March 20 80 March 21 81 March 22 82 March 23 83 March 24 84 March 25 85 March 26 86 March 27 87 March 28 88 March 29 89 March 30 90 March 31 91 April 1 92 April 2 93 April 3 94 April 4 95 April 5 96 April 6 97 April 7 98 April 8 99 April 9 100 April 10 101 April 11 102 April 12 103 April 13 104 April 14 105 April 15 106 April 16 107 April 17 108 April 18 109 April 19 110 April 20 111 April 21 112 April 22 113 April 23 114 April 24 115 April -
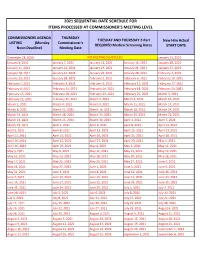
2021 Sequential Date List
2021 SEQUENTIAL DATE SCHEDULE FOR ITEMS PROCESSED AT COMMISSIONER'S MEETING LEVEL COMMISSIONERS AGENDA THURSDAY TUESDAY AND THURSDAY 2-Part New Hire Actual LISTING (Monday Commissioner's REQUIRED Medical Screening Dates START DATE Noon Deadline) Meeting Date December 28, 2020 NO MEETING SCHEDULED January 13, 2021 January 4, 2021 January 7, 2021 January 12, 2021 January 14, 2021 January 20, 2021 January 11, 2021 January 14, 2021 January 19, 2021 January 21, 2021 January 27, 2021 January 18, 2021 January 21, 2021 January 26, 2021 January 28, 2021 February 3, 2021 January 25, 2021 January 28, 2021 February 2, 2021 February 4, 2021 February 10, 2021 February 1, 2021 February 4, 2021 February 9, 2021 February 11, 2021 February 17, 2021 February 8, 2021 February 11, 2021 February 16, 2021 February 18, 2021 February 24, 2021 February 15, 2021 February 18, 2021 February 23, 2021 February 25, 2021 March 3, 2021 February 22, 2021 February 25, 2021 March 2, 2021 March 4, 2021 March 10, 2021 March 1, 2021 March 4, 2021 March 9, 2021 March 11, 2021 March 17, 2021 March 8, 2021 March 11, 2021 March 16, 2021 March 18, 2021 March 24, 2021 March 15, 2021 March 18, 2021 March 23, 2021 March 25, 2021 March 31, 2021 March 22, 2021 March 25, 2021 March 30, 2021 April 1, 2021 April 7, 2021 March 29, 2021 April 1, 2021 April 6, 2021 April 8, 2021 April 14, 2021 April 5, 2021 April 8, 2021 April 13, 2021 April 15, 2021 April 21, 2021 April 12, 2021 April 15, 2021 April 20, 2021 April 22, 2021 April 28, 2021 April 19, 2021 April 22, 2021 April 27, 2021 April -

Date of Close Contact Exposure
Date of Close Contact Exposure 7 days 10 days 14 days Monday, November 16, 2020 Tuesday, November 24, 2020 Friday, November 27, 2020 Tuesday, December 1, 2020 Tuesday, November 17, 2020 Wednesday, November 25, 2020 Saturday, November 28, 2020 Wednesday, December 2, 2020 Wednesday, November 18, 2020 Thursday, November 26, 2020 Sunday, November 29, 2020 Thursday, December 3, 2020 Thursday, November 19, 2020 Friday, November 27, 2020 Monday, November 30, 2020 Friday, December 4, 2020 Friday, November 20, 2020 Saturday, November 28, 2020 Tuesday, December 1, 2020 Saturday, December 5, 2020 Saturday, November 21, 2020 Sunday, November 29, 2020 Wednesday, December 2, 2020 Sunday, December 6, 2020 Sunday, November 22, 2020 Monday, November 30, 2020 Thursday, December 3, 2020 Monday, December 7, 2020 Monday, November 23, 2020 Tuesday, December 1, 2020 Friday, December 4, 2020 Tuesday, December 8, 2020 Tuesday, November 24, 2020 Wednesday, December 2, 2020 Saturday, December 5, 2020 Wednesday, December 9, 2020 Wednesday, November 25, 2020 Thursday, December 3, 2020 Sunday, December 6, 2020 Thursday, December 10, 2020 Thursday, November 26, 2020 Friday, December 4, 2020 Monday, December 7, 2020 Friday, December 11, 2020 Friday, November 27, 2020 Saturday, December 5, 2020 Tuesday, December 8, 2020 Saturday, December 12, 2020 Saturday, November 28, 2020 Sunday, December 6, 2020 Wednesday, December 9, 2020 Sunday, December 13, 2020 Sunday, November 29, 2020 Monday, December 7, 2020 Thursday, December 10, 2020 Monday, December 14, 2020 Monday, November -

Dates for Student-Run Credit Unions 15-16 Northville Schools Northern Schools Novi & Livonia Schools
Dates for Student-Run Credit Unions 15-16 Northville Schools Northern Schools Novi & Livonia Schools Plymouth-Canton Elementary Schools: Bentley Bird Dodson Eriksson Credit Union Credit Union Credit Union Credit Union Tuesdays: Thursdays: October 6 Wednesdays: Tuesdays: October 13 October 20 October 7 October 20 October 27 November 10 October 28 November 10 November 17 November 24 November 18 December 1 December 8 December 8 December 16 December 15 January 5 January 12 January 5 January 6 January 19 January 26 January 19 January 27 February 2 February 9 February 2 February 10 February 23 March 1 February 23 March 2 March 8 March 15 March 8 March 23 March 22 April 5 March 22 April 13 April 12 April 5 May 4 April 19 April 26 April 19 May 25 May 3 May 10 May 17 May 3 Farrand Field Gallimore Hoben Credit Union Credit Union Credit Union Credit Union Wednesdays: Tuesdays: Thursdays: Thursdays: October 21 October 20 October 8 October 15 November 11 November 17 October 22 November 12 December 9 December 1 November 12 December 10 January 6 December 15 December 3 January 14 February 3 January 12 January 7 February 11 February 24 January 26 March 10 March 16 February 4 February 9 April 14 April 6 February 25 February 23 May 12 May 4 March 8 March 10 March 22 April 7 April 12 April 28 April 26 May 12 May 10 June 2 Hulsing Isbister Credit Miller Smith Credit Union Union Credit Union Credit Union Thursdays: Wednesdays: October 1 Thursdays: Thursdays: September 30 October 15 October 8 October 1 October 14 November 19 November 5 October 22 October 28 -

Download PDF File November 26 – December 2, 2018 Eudaly Public
November 2018 December 2018 November 26, 2018 - SuMo TuWe Th Fr Sa SuMo TuWe Th Fr Sa 123 1 45678910 2345678 11 12 13 14 15 16 17 9101112131415 December 2, 2018 18 19 20 21 22 23 24 16 17 18 19 20 21 22 25 26 27 28 29 30 23 24 25 26 27 28 29 30 31 Monday, November 26 Tuesday, November 27 9:00am - 10:45am Weekly Staff Meeting (Office of Commissioner 9:30am - 11:30am Portland Oregon Website Refresh/3-1-1 Eudaly, 1221 SW 4th Avenue Suite 210 - Conference Room) - Eudaly, Recommendations Work Session (City Hall Council Chambers) - Chloe Wheeler, Ted 1:00pm - 1:45pm Rally at Wimbledon Square Apartments (2837 SE 1:20pm - 2:00pm MEET: New Civic Life Staff (Office of Commissioner Colt Dr, Portland, OR 97202) - Eudaly, Chloe Eudaly, 1221 SW 4th Ave, STE 210, Conference Room) - Eudaly, Chloe 2:00pm - 2:30pm MEET: Kimberly Branam, Mark Falcone & Nolan 1:20pm - 2:00pm MEET: New Civic Life Staff (Office of Commissioner Lienhart , Prosper Portland (City Hall) - Branam, Kimberly Eudaly, 1221 SW 4th Ave, STE 210, Conference Room) - Eudaly, Chloe 3:00pm - 4:00pm Weekly Policy Meeting (Conf, Commissioner 2:00pm - 3:00pm Council Prep (Office of Commissioner Eudaly, 1221 Eudaly) - Eudaly, Chloe SW 4th Avenue Suite 210 - Conference Room) - Eudaly, Chloe 4:00pm - 5:00pm MEET: Chief Outlaw, Portland Police (Office of 3:30pm - 4:00pm MEET: Kaiser Permanente/Sunday Parkways Commissioner Eudaly) - Eudaly, Chloe partnership (Office of Commissioner Eudaly, 1221 SW 4th Ave, STE 210, Conference Room) - Eudaly, Chloe Wednesday, November 28 Thursday, November 29 9:30am -

Lesson Plans: Ms. Orama Week Of: November 28-December 2 Grade: 7Th
Lesson Plans: Ms. Orama Week of: November 28-December 2 Grade: 7th Monday, November 28 Word Literature Knowledge Purpose/Relevance I can understand I can read and discuss a novel and retell important parts. how to use prefixes, roots, and suffixes to help me understand new words. Lesson Discuss definition Students will choose six important events from ch. 1-10 to draw and examples of pictures of and write one sentences summaries. ambi-, med/medi, Students will read and discuss ch. 10 of The Hunger Games. -ty Assessment Affix quiz Fri RetellinG pictures and summaries Homework Tuesday, November 29 Word Language Arts Knowledge Purpose/Relevance I can write a persuasive essay Lesson MetriTech Writing Test Assessment Affix quiz Fri. Homework Wednesday, November 30 Word Literature Knowledge Purpose/Relevance I can read and discuss a novel and identify character traits. Lesson Students will design a Facebook page for either Katniss or Peeta. Students will update their pages after each chapter. Students will read and discuss ch. 11 of The Hunger Games. Assessment Affix Quiz Fri. Homework Thursday, December 1 Word Literature Knowledge Purpose/Relevance I can read and discuss a novel and answer comprehension questions. Lesson Students will read and discuss ch. 12 of The Hunger Games. Students will answer comprehension questions from ch.11-12. Assessment Affix quiz Fri. Comprehension questions Homework Friday, December 2 Word Literature Knowledge Purpose/Relevance I can review and write an extended response Lesson Students will read a passage and write a practice extended response Assessment Affix quiz Fri. ERR Homework . -
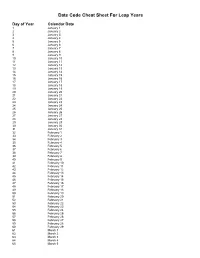
Julian Date Cheat Sheet for Leap Years
Date Code Cheat Sheet For Leap Years Day of Year Calendar Date 1 January 1 2 January 2 3 January 3 4 January 4 5 January 5 6 January 6 7 January 7 8 January 8 9 January 9 10 January 10 11 January 11 12 January 12 13 January 13 14 January 14 15 January 15 16 January 16 17 January 17 18 January 18 19 January 19 20 January 20 21 January 21 22 January 22 23 January 23 24 January 24 25 January 25 26 January 26 27 January 27 28 January 28 29 January 29 30 January 30 31 January 31 32 February 1 33 February 2 34 February 3 35 February 4 36 February 5 37 February 6 38 February 7 39 February 8 40 February 9 41 February 10 42 February 11 43 February 12 44 February 13 45 February 14 46 February 15 47 February 16 48 February 17 49 February 18 50 February 19 51 February 20 52 February 21 53 February 22 54 February 23 55 February 24 56 February 25 57 February 26 58 February 27 59 February 28 60 February 29 61 March 1 62 March 2 63 March 3 64 March 4 65 March 5 66 March 6 67 March 7 68 March 8 69 March 9 70 March 10 71 March 11 72 March 12 73 March 13 74 March 14 75 March 15 76 March 16 77 March 17 78 March 18 79 March 19 80 March 20 81 March 21 82 March 22 83 March 23 84 March 24 85 March 25 86 March 26 87 March 27 88 March 28 89 March 29 90 March 30 91 March 31 92 April 1 93 April 2 94 April 3 95 April 4 96 April 5 97 April 6 98 April 7 99 April 8 100 April 9 101 April 10 102 April 11 103 April 12 104 April 13 105 April 14 106 April 15 107 April 16 108 April 17 109 April 18 110 April 19 111 April 20 112 April 21 113 April 22 114 April 23 115 April