Oral Medicines for the Management of Urinary Incontinence, Frequency & Overactive Bladder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

The Effects of Oral Administration of the Novel Muscarinic Receptor
Choi et al. BMC Urology (2020) 20:41 https://doi.org/10.1186/s12894-020-00611-8 RESEARCH ARTICLE Open Access The effects of oral administration of the novel muscarinic receptor antagonist DA- 8010 on overactive bladder in rat with bladder outlet obstruction Jin Bong Choi1, Seung Hwan Jeon2, Eun Bi Kwon3, Woong Jin Bae4, Hyuk Jin Cho2, U-Syn Ha2, Sung-Hoo Hong2, Ji Youl Lee2 and Sae Woong Kim4* Abstract Background: DA-8010 is a novel compound developed for the treatment of overactive bladder (OAB) and urinary incontinence. The aims of this study were to investigate the effects of DA-8010 on OAB in a rat model. Methods: Study animals were divided into the following five groups of seven animals each: a sham-operated control group, a control group with partial bladder outlet obstruction (BOO) (OAB group), and three DA-8010 (doses of 0.3 mg/kg/day, 1 mg/kg/day, and 3 mg/kg/day, respectively) with partial BOO groups. Oral administration of the drugs was continued for 14 days after 2 weeks of partial BOO. After 4 weeks of partial BOO, cystometrography was performed in all groups. Additionally, pro-inflammatory cytokines, Rho-kinases, and histology of the bladder were analyzed. Results: There was a significant increase in the contraction interval and a decrease in contraction pressure in the 3 mg/kg/day DA-8010 group versus those in the OAB group. Rho kinase was also significantly decreased in the DA- 8010 3 mg/kg/day dosage treatment group. The increased ratio of collagen to smooth muscle after partial BOO was significantly attenuated in the DA-8010 3 mg/kg/day dosage group. -

Long Term Follow up of Mirabegron - a Real Life- Pragmatic Experience
Central Journal of Urology and Research Bringing Excellence in Open Access Research Article *Corresponding author Haitham Abdelmoteleb, Bristol Urological Institute, Southmead Hospital, Bristol, BS10 5NB, UK, Tel: 440-7884- Long Term Follow Up of 827995; Email: Submitted: 04 June 2016 Mirabegron - A Real Life- Accepted: 22 August 2016 Published: 24 August 2016 ISSN: 2379-951X Pragmatic Experience Copyright Haitham Abdelmoteleb*, Musaab Yassin, and Hashim Hashim © 2016 Abdelmoteleb et al. Bristol Urological Institute, South mead Hospital, UK OPEN ACCESS Abstract Keywords • Mirabegron Objectives: To evaluate the efficacy and tolerability of Mirabegron for the • Beta-3 agonist treatment of overactive bladder symptoms in a real life, long term follow up study • Overactive bladder syndrome conducted in a tertiary referral centre. • Long term Methods: A structured telephone questionnaire of patients was conducted in order to evaluate the efficacy and tolerability of Mirabegron. Patients who were initially prescribed and responded to Mirabegron 50mg once daily between 6/2013 and 9/2013, were interviewed to see if they were compliant with treatment, continue to respond to treatment and if they discontinued treatment. Results: Follow-up was for a mean of 11.7 months. At short-term follow-up, 20/39 patients responded to treatment. In the long term follow-up, 18/20 patients were still using Mirabegron. 2/20 patients discontinued because of lack of efficacy. Overall, the main reasons for discontinuation of Mirabegron after trying it for a mean of 5.3 months, was lack of efficacy and adverse events. The majority of AEs were mild in severity and few were serious. Other reasons include the lack of further prescription from general practitioners. -

Betmiga, INN-Mirabegron
EMA/591015/2015 EMEA/H/C/002388 EPAR summary for the public Betmiga mirabegron This is a summary of the European public assessment report (EPAR) for Betmiga. It explains how the Committee for Medicinal Products for Human Use (CHMP) assessed the medicine to reach its opinion in favour of granting a marketing authorisation and its recommendations on the conditions of use for Betmiga. What is Betmiga? Betmiga is a medicine containing the active substance mirabegron. It is available as prolonged-release tablets (25 mg, 50 mg). ‘Prolonged-release’ means that mirabegron is released slowly from the tablet over a few hours. What is Betmiga used for? Betmiga is used in adults with overactive bladder syndrome. It is used to treat certain symptoms of the condition: urgency (sudden urge to urinate), increased urinary frequency (the need to urinate frequently) and urge incontinence (involuntary leakage of urine from the bladder when a sudden strong need to urinate is felt). The medicine can only be obtained with a prescription. How is Betmiga used? The recommended dose of Betmiga is 50 mg once a day. In patients who have reduced kidney or liver function the doctor may need to prescribe a lower dose or avoid the use of Betmiga, especially in patients taking certain other medicines. For full details, see the package leaflet (also part of the EPAR). 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2015. -

Anticholinergic Drugs Improve Symptoms but Increase Dry Mouth in Adults with Overactive Bladder Syndrome
Source of funding: Evid Based Nurs: first published as 10.1136/ebn.6.2.49 on 1 April 2003. Downloaded from Review: anticholinergic drugs improve symptoms but Health Research Council of Aotearoa increase dry mouth in adults with overactive bladder New Zealand. syndrome For correspondence: Jean Hay-Smith, Hay-Smith J, Herbison P,Ellis G, et al. Anticholinergic drugs versus placebo for overactive bladder syndrome in adults. Dunedin School of Cochrane Database Syst Rev 2002;(3):CD003781 (latest version May 29 2002). Medicine, University of Otago, Dunedin, New QUESTION: What are the effects of anticholinergic drugs in adults with overactive Zealand. jean.hay-smith@ bladder syndrome? otago.ac.nz Data sources Parallel arm studies of anticholinergic drugs v placebo for overactive bladder syndrome in Studies were identified by searching the Cochrane adults at 12 days to 12 weeks* Incontinence Group trials register (to January 2002) Weighted event rates and reference lists of relevant papers. Anticholinergic Study selection Outcomes drugs Placebo RBI (95% CI) NNT (CI) Randomised or quasi-randomised controlled trials in Self reported cure or adults with symptomatic diagnosis of overactive bladder improvement (8 studies) 63% 45% 41% (29 to 54) 6 (5 to 8) syndrome, urodynamic diagnosis of detrusor overactiv- RRI (CI) NNH (CI) ity, or both, that compared an anticholinergic drug Dry mouth (20 studies) 36% 15% 138 (70 to 232) 5 (4 to 7) (given to decrease symptoms of overactive bladder) with Outcomes Weighted mean difference (CI) placebo or no treatment. Studies of darifenacin, emepronium bromide or carrageenate, dicyclomine Number of leakage episodes in 24 hours (9 − chloride, oxybutynin chloride, propiverine, propanthe- studies) 0.56 (–0.73 to –0.39) Number of micturitions in 24 hours (8 studies) −0.59 (–0.83 to –0.36) line bromide, tolterodine, and trospium chloride were Maximum cystometric volume (ml) (12 studies) 54.3 (43.0 to 65.7) included. -

Frailty & Cognihon: Management of OAB in Elderly & Frail Pahents
Frailty & Cogni.on: Management of OAB in Elderly & Frail Pa.ents MR. RAHUL MISTRY CONSULTANT UROLOGICAL SURGEON POGP CONFERENCE NOVEMBER 2016 Topics • What are LUTS? • Symptom definiDons • The impact of OAB on paents • Management of OAB • The challenge of treang OAB • The Ancholinergic burden • Novel treatment of OAB Change of Terminology • LUTS = Lower urinary tract symptoms • LUTS instead of “prostasm” • Storage instead of “irritave” • Voiding instead of “obstrucDve” What are LUTS Post-micturion Storage symptoms Voiding symptoms symptoms DayDme frequency Slow stream Post-micturiDon Nocturia Spraying dribbling Incomplete Urgency IntermiUency emptying Urinary Hesitancy inconnence Straining Terminal dribbling Definions • Urgency - sudden compelling desire to pass urine which is difficult to defer • Urinary inconnence • any involuntary leakage of urine (urge / stress) • may need to be disDnguished from sweang or vaginal discharge • Increased dayme frequency - the complaint by the paent who considers that he/she voids too o]en by day • Nocturia - individual has to wake at night one or more Dmes to void • ICS DefiniDons, Abrams P et al. Neurourol Urodyn; 21:167-178 (2002) Defini.on of Overac.ve Bladder (OAB) (Internaonal Connence Society) 1. Abrams P et al. Neurourol Urodyn 2002;21:167-178 Mrs W. E. Terrible, your classic pa.ent? Age: 64 year old woman Occupaon: Recently reDred from an office job Symptoms: • Urinary frequency (14−15 Dmes a day) • Urge inconDnence (daily) • Nocturia (3 Dmes a night) THe impact of OAB on pa.ents How do OAB symptoms affect pa.ents? haven’t slept depressing like a baby negave lose control locked in embarrassing exhausted no control terrible so red I keep it xxx secret Quotes from a video of real-life OAB paents talking about how OAB has affected their lives. -

Package Leaflet
Version 4, 02/2016 Propigen 5 mg coated tablets v005common PACKAGE LEAFLET 1 PACKAGE LEAFLET: INFORMATION FOR THE USER PROPIGEN 5 MG COATED TABLETS (PROPIVERINE HYDROCHLORIDE) Read all of this leaflet carefully before you or your child start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or your pharmacist. - This medicine has been prescribed for you or your child, respectively, only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours or your child’s. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet (see section 4). The name of your medicine is Propigen 5 mg. The active substance is propiverine hydrochloride and the other ingredients are listed at the end of the leaflet (section 6, Contents of the pack and other information). What is in this leaflet: 1. What Propigen 5 mg is and what it is used for 2. What you need to know before you or your child take Propigen 5 mg 3. How to take Propigen 5 mg 4. Possible side effects 5. How to store Propigen 5 mg 6. Contents of the pack and other information 1. WHAT PROPIGEN 5 MG IS AND WHAT IT IS USED FOR Propigen 5 mg is used for the treatment of adults and children who have difficulty in controlling their bladder due to bladder overactivity or, in some cases, problems with the spinal cord. -

Urinary Antispasmodics TCO 02.2018
Therapeutic Class Overview Urinary antispasmodics INTRODUCTION • Overactive bladder (OAB) is defined as urinary urgency, with or without urge incontinence, usually with frequency and nocturia, in the absence of a causative infection or pathological conditions. Urinary incontinence has been shown to greatly reduce quality of life in areas such as mental and general health in addition to physical and social functioning (American Urological Association 2019, Coyne et al 2008, Haab 2014, International Continence Society 2015). Children with OAB usually have detrusor overactivity as diagnosed through cystometric evaluation. Neurogenic detrusor overactivity is predominantly caused by a congenital neural tube defect in children (Austin et al 2016, Franco ○ et al 2020). • Behavioral therapies (eg, bladder training, bladder control strategies, pelvic floor muscle training and fluid management) are considered first-line treatment in all patients with OAB (American Urological Association 2019). • Urinary antispasmodics are used as first-line pharmacological therapy in OAB (American College of Obstetricians and Gynecologists 2015, American Urological Association 2019, Blok et al 2020, Burkhard et al 2018). Anticholinergic therapy has been frequently used in patients with neurogenic detrusor overactivity, but there are limited data in this specific population (Haab 2014). • The○ urinary antispasmodics used for the treatment of OAB belong to 2 classes of drugs, which include anticholinergic compounds known as muscarinic receptor antagonists, and the beta-3 adrenergic agonist (AR), mirabegron. The anticholinergic agents act as antagonists of acetylcholine at muscarinic cholinergic receptors, thereby relaxing smooth muscle in the bladder and decreasing bladder contractions. ○ . Oral immediate-release (IR) and extended-release (ER) formulations (LA, XL, and XR) are available for oxybutynin (Ditropan), tolterodine (Detrol), and trospium. -
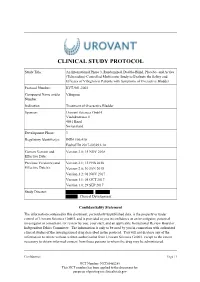
Study Protocol
CLINICAL STUDY PROTOCOL Study Title: An International Phase 3, Randomized, Double-Blind, Placebo- and Active (Tolterodine)-Controlled Multicenter Study to Evaluate the Safety and Efficacy of Vibegron in Patients with Symptoms of Overactive Bladder Protocol Number: RVT-901-3003 Compound Name and/or Vibegron Number: Indication Treatment of Overactive Bladder Sponsor: Urovant Sciences GmbH Viaduktstrasse 8 4051 Basel Switzerland Development Phase: 3 Regulatory Identifier(s): IND# 106,410 EudraCT# 2017-003293-14 Current Version and Version 3.0; 15 NOV 2018 Effective Date: Previous Version(s) and Version 2.1; 12 FEB 2018 Effective Date(s): Version 2.0; 30 JAN 2018 Version 1.2; 01 NOV 2017 Version 1.1; 05 OCT 2017 Version 1.0; 29 SEP 2017 Study Director: , , Clinical Development Confidentiality Statement The information contained in this document, particularly unpublished data, is the property or under control of Urovant Sciences GmbH, and is provided to you in confidence as an investigator, potential investigator or consultant, for review by you, your staff, and an applicable Institutional Review Board or Independent Ethics Committee. The information is only to be used by you in connection with authorized clinical studies of the investigational drug described in the protocol. You will not disclose any of the information to others without written authorization from Urovant Sciences GmbH. except to the extent necessary to obtain informed consent from those persons to whom the drug may be administered. Confidential Page | 1 NCT Number: NCT03492281 This NCT number has been applied to the document for purposes of posting on clinicaltrials.gov Clinical Study Protocol RVT-901-3003 Urovant Sciences GmbH Effective: 15 NOV 2018 SUMMARY OF CHANGES Version Location Description of Change 3.0 Global Minor typographical/formatting errors were corrected. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Solifenacin-Induced Delirium and Hallucinations☆
General Hospital Psychiatry 35 (2013) 682.e3–682.e4 Contents lists available at ScienceDirect General Hospital Psychiatry journal homepage: http://www.ghpjournal.com Case Report Solifenacin-induced delirium and hallucinations☆ Matej Štuhec, Pharm.D. ⁎ Ormoz Psychiatric Hospital, Department for Clinical Pharmacy, Slovenia, Ptujska Cesta 33, Ormoz, Slovenia article info abstract Article history: Solifenacin-induced cognitive adverse effects have not been reported frequently, but solifenacin-induced Received 11 April 2013 delirium and hallucinations with successful switching to darifenacin, without additional drug, have not been Revised 5 June 2013 reported in the literature. In this case report, we present an 80-year-old Caucasian male with insomnia and Accepted 5 June 2013 anxiety symptoms and overactive bladder who developed delirium and hallucinations when treated with Keywords: solifenacin and trazodone. After solifenacin discontinuation and switching to darifenacin, symptoms significantly improved immediately. Such a case has not yet been described in literature; however, an Solifenacin Delirium adverse effect associated with solifenacin can occur, as this report clearly demonstrates. Hallucinations © 2013 Elsevier Inc. All rights reserved. Darifenacin Antimuscarinic adverse effect Case report 1. Introduction tion of Diseases, 10th Revision (ICD-10)], and depression with psychotic features was ruled out with differential diagnosis. Patient reported Solifenacin is a competitive muscarinic receptor antagonist, which insomnia, fear, fatigue, nausea, chest pain, shortness of breath and is used for overactive bladder (OAB) treatment. It acts as an headache. Solifenacin (Vesicare) 5 mg daily in morning dose was antimuscarinic agent, showing the highest affinity for the muscarinic prescribed to him 1 week earlier by his physicians because of OAB. M(3) receptor, which mediates urinary bladder contraction. -

3 Drugs That May Cause Delirium Or Problem Behaviors CARD 03 19 12 JUSTIFIED.Pub
Drugs that May Cause Delirium or Problem Behaviors Drugs that May Cause Delirium or Problem Behaviors This reference card lists common and especially problemac drugs that may Ancholinergics—all drugs on this side of the card. May impair cognion cause delirium or contribute to problem behaviors in people with demena. and cause psychosis. Drugs available over‐the‐counter marked with * This does not always mean the drugs should not be used, and not all such drugs are listed. If a paent develops delirium or has new problem Tricyclic Andepressants Bladder Anspasmodics behaviors, a careful review of all medicaons is recommended. Amitriptyline – Elavil Darifenacin – Enablex Be especially mindful of new medicaons. Clomipramine – Anafranil Flavoxate – Urispas Desipramine – Norpramin Anconvulsants Psychiatric Oxybutynin – Ditropan Doxepin – Sinequan Solifenacin – VESIcare All can cause delirium, e.g. All psychiatric medicaons should be Imipramine – Tofranil Tolterodine – Detrol Carbamazepine – Tegretol reviewed as possible causes, as Nortriptyline – Aventyl, Pamelor Gabapenn – Neuronn effects are unpredictable. Trospium – Sanctura Anhistamines / Allergy / Leveracetam – Keppra Notable offenders include: Insomnia / Sleep Valproic acid – Depakote Benzodiazepines e.g. Cough & Cold Medicines *Diphenhydramine – Sominex, ‐Alprazolam – Xanax *Azelasne – Astepro Pain Tylenol‐PM, others ‐Clonazepam – Klonopin *Brompheniramine – Bromax, All opiates can cause delirium if dose *Doxylamine – Unisom, Medi‐Sleep ‐Lorazepam – Avan Bromfed, Lodrane is too high or