Captain Dies from Hyperthermia and Exertional Heatstroke While Performing Advanced Survival Training - Texas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Motion Sickness: Definition
Clinical and physiological characteristics of cybersickness Submitted in fulfilment of the requirements for the degree of Doctor of Philosophy (Human Physiology) School of Biomedical Sciences and Pharmacy Faculty of Health and Medicine University of Newcastle, Australia This research was supported by an Australian Government Research Training Program (RTP) Scholarship. 1 STATEMENT OF ORIGINALITY I hereby certify that the work embodied in the thesis is my own work, conducted under normal supervision. The thesis contains no material which has been accepted, or is being examined, for the award of any other degree or diploma in any university or other tertiary institution and, to the best of my knowledge and belief, contains no material previously published or written by another person, except where due reference has been made. I give consent to the final version of my thesis being made available worldwide when deposited in the University’s Digital Repository, subject to the provisions of the Copyright Act 1968 and any approved embargo. Alireza Mazloumi Gavgani 2 ACKNOWLEDGMENT OF AUTHORSHIP I hereby certify that the work embodied in this thesis contains published paper/s/scholarly work of which I am a joint author. I have included as part of the thesis a written declaration endorsed in writing by my supervisor, attesting to my contribution to the joint publication/s/scholarly work. Alireza Mazloumi Gavgani 3 STATEMENT OF COLLABORATION I hereby certify that some parts of the work embodied in this thesis have been done in collaboration with other researchers. I have included as part of the thesis a statement clearly outlining the extent of collaboration, with whom and under what auspices. -

SURVIVAL SKILLS Activity Plan – Hiking Series Actpa015
Backpacking and Hiking SURVIVAL SKILLS Activity Plan – Hiking Series ACTpa015 BACKGROUND Project Skills: Learning how to survive in an emergency situation is important for everyone. • Learn the seven basic Although wilderness-based survival situations are most common, survival situations survival needs of our can occur in urban and rural environments, too. The following activities will help bodies participants learn about the definition of a survival situation, what basic needs must be • Discover what materials met to ensure survival, and creative solutions for survival situations. will help us meet these needs to survive The three mini-activities in this lesson will work well for school conservation days, in emergency situations class presentations, after school activity, Boys and Girls Clubs, camp nature session, and many other learning situations. Life Skills: • Teamwork WHAT TO DO Academic Standards: Activity: Introduction to • Science: H.8.3. Survival Skills Understand the Bring the group together and consequences of facilitate a discussion about decisions affecting their current ideas on the topic personal health and of “survival skills.” safety. Ask them to name a “survival Grade Levels: 4-7 situation.” Typically, they will identify situations like a plane Time: 30-45 minutes crash or hurricane that has a remote chance of happening to Supplies Needed: them. Then ask them to describe an event that could happen to them. What events • Writing utensils and could quickly turn into survival situations? Some possibilities include: paper -
Training Orientation Packet
Basic Training Orientation Packet For additional information, please visit our website at http://www.kcesar.org or email ESAR training at [email protected] Version 06/29/21 Basic Training at a Glance Overview ESAR Basic Training is a comprehensive program designed to prepare new members for the challenges that they will face in the field. As a trainee, you will receive instruction and demonstrate proficiency in Wilderness Navigation & Survival skills, Search Method Theory, and First Aid & CPR. You will also receive instruction on Helicopter Safety, Legal Issues, and Crime Scene Awareness. After basic training, many of these certifications must be maintained through ongoing training. Some can be renewed by going on missions, whereas others will need to be maintained through continuing education every two to five years. Advanced Courses Basic Training prepares you to serve on missions that do not require technical skills or snow/avalanche hazards. Advanced training is available for selected individuals who wish to gain skills for missions involving technical rescue and snow. Courses such as Basic Snow, AIARE 1, Emergency Medical Technician, and Rope Rescue are offered periodically following Basic Training. Schedule Basic Training begins in September and runs through April; it is purposefully scheduled during the winter months to give trainees experience working in the worst conditions they could encounter on a mission. Training may involve snow, ice, wind, rain and other unpleasant situations. Trainees are expected to understand how to prevent hypothermia, to be aware of the conditions around them, and to take care of themselves and their team. Inclement Weather Training is rarely cancelled due to weather. -

Hyperthermia & Heat Stroke: Heat-Related Conditions
Hyperthermia & Heat Stroke: Heat-Related Conditions Joseph Rampulla, MS, APRN,BC eat-related conditions occur when excess heat taxes or overwhelms the body’s thermoregulatory mechanisms. Heat illness is preventable and occurs more Hcommonly than most clinicians realize. Heat illness most seriously affects the poor, urban-dwellers, young children, those with chronic physical and mental illnesses, substance abusers, the elderly, and people who engage in excessive physical The exposure to activity under harsh conditions. While considerable overlap occurs, the important the heat and the concrete during the syndromes are: heat stroke, heat exhaustion, and heat cramps. Heat stroke is a life- hot summer months places many rough threatening emergency and occurs when the loss of thermoregulatory control results sleepers at great risk in hyperpyrexia (very high fever) and severe damage to many internal organs. for heat stroke and hyperthermia. Photo by Epidemiology Sharon Morrison RN Heat illness is generally underreported, and the deaths than all other natural disasters combined in true incidence is unknown. Death rates from other the USA. The elderly, the very poor, and socially causes (e.g. cardiovascular, respiratory) increase isolated individuals are disproportionately affected during heat waves but are generally not reflected in by heat waves. For example, death records during the morbidity and mortality statistics related to heat heat waves invariably include many elders who died illness. Nonetheless, heat waves account for more alone in hot apartments. Age 65 years, chronic The Health Care of Homeless Persons - Part II - Hyperthermia and Heat Stroke 199 illness, and residence in a poor neighborhood are greater than 65. -

Hypothermia Hyperthermia Normothemic
Means normal body temperature. Normal body core temperature ranges from 99.7ºF to 99.5ºF. A fever is a Normothemic body temperature of 99.5 to 100.9ºF and above. Humans are warm-blooded mammals who maintain a constant body temperature (euthermia). Temperature regulation is controlled by the hypothalamus in the base of the brain. The hypothalamus functions as a thermostat for the body. Temperature receptors (thermoreceptors) are located in the skin, certain mucous membranes, and in the deeper tissues of the body. When an increase in body temperature is detected, the hypothalamus shuts off body mechanisms that generate heat (for example, shivering). When a decrease in body temperature is detected, the hypothalamus shuts off body mechanisms designed to cool the body (for example, sweating). The body continuously adjusts the metabolic rate in order to maintain a constant CORE Hypothermia Core body temperatures of 95ºF and lower is considered hypothermic can cause the heart and nervous system to begin to malfunction and can, in many instances, lead to severe heart, respiratory and other problems that can result in organ damage and death.Hannibal lost nearly half of his troops while crossing the Pyrenees Alps in 218 B.C. from hypothermia; and only 4,000 of Napoleon Bonaparte’s 100,000 men survived the march back from Russia in the winter of 1812 - most dying of starvation and hypothermia. During the sinking of the Titanic most people who entered the 28°F water died within 15–30 minutes. Symptoms: First Aid : Mild hypothermia: As the body temperature drops below 97°F there is Call 911 or emergency medical assistance. -

Malignant Hyperthermia.Pdf
Malignant Hyperthermia Matthew Alcusky PharmD, MS Student University of Rhode Island July, 2013 Financial Disclosure I have no financial obligations to disclose. Outline • Introduce malignant hyperthermia including its causes and implications • Describe the underlying pathophysiology • Detail the clinical presentation of MH • Summarize the necessary pharmacological and non-pharmacological treatment of MH • Highlight necessary considerations with the use of dantrolene • Discuss recrudescence Malignant Hyperthermia • A life threatening reaction that is most often triggered by the use of inhalational anesthetics • Estimated incidence of 1 in 5,000 to 1 in 100,000 anesthesia inductions • Early recognition and treatment is essential in reducing morbidity and mortality • Screening patients for past anesthesia history and family history, as well as conducting testing on at risk individuals is necessary to reduce MH occurrence Rosenberg H, Davis M, James D, Pollock N, Stowell K. Malignant hyperthermia. Orphanet J Rare Dis. 2007 Apr 24;2:21. Review. Drugs Triggering Malignant Hyperthermia • Desflurane • Succinylcholine- • Enflurane only non-inhalational • Halothane anesthetic that triggers MH • Isoflurane • Nitrous Oxide- only • Methoxyflurane inhalational anesthetic • Sevoflurane that does not cause MH Hopkins PM. Malignant hyperthermia: pharmacology of triggering. Br J Anaesth. 2011 Jul;107(1):48-56. doi: 10.1093/bja/aer132. Epub 2011 May 30. Review. Pathophysiology • MH partially attributed to a dominant mutation in the ryanodine receptror 1 (RYR1) – Ryanodine receptors are activated by elevated Ca2+ levels, known as store overload induced calcium release (SOICR) – Mutant receptors are activated by lower Ca2+ levels – Volatile anesthetics further lower the SOICR threshold MacLennan DH, Chen SR. Store overload-induced Ca2mutations + release as a triggering mechanism for CPVT and MH episodes caused by in RYR and CASQ genes. -

Guidelines for Management of a Malignant Hyperthermia (MH) Crisis
Guidelines for the management of a Malignant Hyperthermia Crisis Successful treatment of a Malignant Hyperthermia (MH) crisis depends on early diagnosis and aggressive treatment. The onset of a reaction can be within minutes of induction or may be more insidious. Previous uneventful anaesthesia does not exclude MH. The steps below are intended as an aide memoire. Presentation may vary and treatment should be modified accordingly. Know where the dantrolene is stored in your theatre. Treatment can be optimised by teamwork. Call for help Diagnosis - consider MH if: 1 1. Unexplained, unexpected increase in end-tidal CO2 together with 2. Unexplained, unexpected tachycardia together with 3. Unexplained, unexpected increased in oxygen consumption Masseter muscle spasm, and especially more generalised muscle rigidity after suxamethonium, indicate a high risk of MH susceptibility but are usually self-limiting. Take measures to halt the MH process: 2 1. Remove trigger drugs, turn off vaporisers, use high fresh gas flows (oxygen), use a new, clean non-rebreathing circuit, hyperventilate. Maintain anaesthesia with intravenous agents such as propofol until surgery completed. 2. Dantrolene; give 2-3 mg.kg-1 i.v. initially and then 1 mg.kg-1 PRN. 3. Use active body cooling but avoid vasoconstriction. Convert active warming devices to active cooling, give cold 3 intravenous infusions, cold peritoneal lavage, extracorporeal heat exchange. Monitor: 4 ECG, SpO2, end-tidal CO2, invasive arterial BP, CVP, core and peripheral temperature, urine output and pH, arterial blood gases, potassium, haematocrit, platelets, clotting indices, creatine kinase (peaks at 12-24h). Treat the effects of MH: 5 1. Hypoxaemia and acidosis: 100% O2, hyperventilate, sodium bicarbonate. -
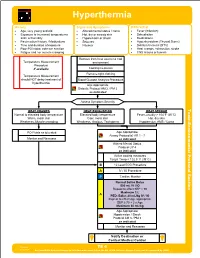
TE 04 Hyperthermia Protocol Final 2017 Editable.Pdf
Hyperthermia History Signs and Symptoms Differential • Age, very young and old • Altered mental status / coma • Fever (Infection) • Exposure to increased temperatures • Hot, dry or sweaty skin • Dehydration and / or humidity • Hypotension or shock • Medications • Past medical history / Medications • Seizures • Hyperthyroidism (Thyroid Storm) • Time and duration of exposure • Nausea • Delirium tremens (DT's) • Poor PO intake, extreme exertion • Heat cramps, exhaustion, stroke • Fatigue and / or muscle cramping • CNS lesions or tumors Remove from heat source to cool Temperature Measurement environment Procedure if available Cooling measures Remove tight clothing Temperature Measurement should NOT delay treatment of Blood Glucose Analysis Procedure hyperthermia Age Appropriate Diabetic Protocol AM 2 / PM 2 as indicated Assess Symptom Severity Toxic HEAT CRAMPS HEAT EXHAUSTION HEAT STROKE Normal to elevated body temperature Elevated body temperature Fever, usually > 104°F (40°C) Warm, moist skin Cool, moist skin Hot, dry skin - Weakness, Muscle cramping Weakness, Anxious, Tachypnea Hypotension, AMS / Coma Section Environmental Protocol PO Fluids as tolerated Age Appropriate Airway Protocol(s) AR 1 - 7 Monitor and Reassess as indicated Altered Mental Status Protocol UP 4 as indicated Active cooling measures Target Temp < 102.5° F (39°C) B 12 Lead ECG Procedure A IV / IO Procedure P Cardiac Monitor A Age Appropriate Hypotension / Shock Protocol AM 5 / PM 3 as indicated Monitor and Reassess Notify Destination or Contact Medical Control Revised TE 4 09/29/2017 Any local EMS System changes to this document must follow the NC OEMS Protocol Change Policy and be approved by OEMS Hyperthermia Toxic - Environmental Protocol Environmental Section Protocol Pearls • Recommended Exam: Mental Status, Skin, HEENT, Heart, Lungs, Neuro • Extremes of age are more prone to heat emergencies (i.e. -

How to Improve the Antioxidant Defense in Asphyxiated Newborns—Lessons from Animal Models
antioxidants Review How to Improve the Antioxidant Defense in Asphyxiated Newborns—Lessons from Animal Models Hanna Kletkiewicz 1 , Maciej Klimiuk 1, Alina Wo´zniak 2, Celestyna Mila-Kierzenkowska 2 , Karol Dokladny 3 and Justyna Rogalska 1,* 1 Department of Animal Physiology and Neurobiology, Faculty of Biological and Veterinary Sciences, Nicolaus Copernicus University, 87-100 Torun, Poland; [email protected] (H.K.); [email protected] (M.K.) 2 Department of Medical Biology and Biochemistry, Faculty of Medicine, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University, 87-100 Torun, Poland; [email protected] (A.W.); [email protected] (C.M.-K.) 3 Department of Internal Medicine, School of Medicine, University of New Mexico, Albuquerque, NM 87131, USA; [email protected] * Correspondence: [email protected]; Tel.: +48-56-611-26-31 Received: 24 August 2020; Accepted: 15 September 2020; Published: 21 September 2020 Abstract: Oxygen free radicals have been implicated in brain damage after neonatal asphyxia. In the early phase of asphyxia/reoxygenation, changes in antioxidant enzyme activity play a pivotal role in switching on and off the cascade of events that can kill the neurons. Hypoxia/ischemia (H/I) forces the brain to activate endogenous mechanisms (e.g., antioxidant enzymes) to compensate for the lost or broken neural circuits. It is important to evaluate therapies to enhance the self-protective capacity of the brain. In animal models, decreased body temperature during neonatal asphyxia has been shown to increase cerebral antioxidant capacity. However, in preterm or severely asphyxiated newborns this therapy, rather than beneficial seems to be harmful. Thus, seeking new therapeutic approaches to prevent anoxia-induced complications is crucial. -

An Updated Narrative Review on Ergometric Systems Applied to Date in Assessing Divers’ Fitness
healthcare Review An Updated Narrative Review on Ergometric Systems Applied to Date in Assessing Divers’ Fitness Sven Dreyer 1, Johannes Schneppendahl 1, Fabian Moeller 2, Andreas Koch 3, Thomas Muth 4 and Jochen D Schipke 5,* 1 Hyperbaric Oxygen Therapy, University Hospital Düsseldorf, Moorenstrasse 5, 40225 Düsseldorf, Germany; [email protected] (S.D.); [email protected] (J.S.) 2 Department of Exercise Physiology, Institute of Exercise Training and Sport Informatics, German Sport University Cologne, 50933 Cologne, Germany; [email protected] 3 German Naval Medical Institute, Maritime Medicine, 24119 Kronshagen, Germany; [email protected] 4 Institute of Occupational, Social and Environmental Medicine, Medical Faculty and University Hospital Düsseldorf, Heinrich-Heine-University, 40225 Düsseldorf, Germany; [email protected] 5 Forschungsgruppe Experimentelle Chirurgie, Universitäts-Klinikum Düsseldorf, Moorenstrasse 5, 40225 Düsseldorf, Germany * Correspondence: [email protected]; Tel.: +49-211-57-99-94 Abstract: Many recreational divers suffer medical conditions, potentially jeopardizing their safety. To scale down risks, medical examinations are mandatory and overwhelmingly performed using bicycle ergometry, which overlooks some important aspects of diving. Searching ergometric systems that better address the underwater environment, a systematic literature search was conducted using the keywords ‘diving’, ‘fitness’, ‘ergometry’, and ‘exertion’. All presented alternative systems Citation: Dreyer, S.; Schneppendahl, found convincingly describe a greatly reduced underwater physical performance. Thus, if a diver’s J.; Moeller, F.; Koch, A.; Muth, T.; workload in air should already be limited, he/she will suffer early from fatigue, risking a diving Schipke, J.D. An Updated Narrative incident. How to assess fitness? Performance diagnostics in sports is always specific for a modality Review on Ergometric Systems or movement. -

Care of the Addicted Patient
CARE OF THE ADDICTED PATIENT Andrew Linnaus, MD DISCLOSURE • No financial relationships or conflicts of interest to disclose. GOALS • Review Traditional Toxidromes and associated drugs of abuse • Review Emerging Drugs of Abuse • Discuss the Current Opiate Epidemic • Discuss care for the recovering/addicted patient. SYMPATHOMIMETIC SYMPATHOMIMETIC • Cocaine, Amphetamines, LSD, Ectasy (MDMA) SYMPATHETIC RESPONSE • Eyes (Alpha 1): Pupil Dilation/Mydriasis • Heart (Beta 1): Increased HR, Contraction, irritability • Often sinus tachycardia but at risk for arrythmias. • Lungs (Beta2): Dilation of bronchial tree • Skin (Alpha 1): Sweating, goose bumps • Muscles (Beta2): Vasodilation-increased blood flow. • Tachycardia, Hypertension, Hyperthermia SYMPATHETIC RESPONSE • Physical Exam • Tremor, warm skin, diaphoresis, hypoactive bowel sounds. • Sympathetic stimulation Epinephrine (adrenalin) release form the adrenal glands • “Fight or flight” SYMPATHOMIMETIC-HYPERTHERMIA • Hyperthermia • Increased motor tone generates heat • Can be exacerbated by dehydration and vasoconstriction • Temp >106 F documented DIC and multisystem organ failure • Treatment • Aggressive use of fluid and benzodiazepines. • Neuromuscular paralysis and intubation as needed. • Continuous monitoring of core temperature-rectal probe. • Wet sheets with large fans, pack groin and axilla with ice packs • Goal of 102 or less within 20 minutes SYMPATHOMIMETIC-HYPERTENSION • Hypertensive Emergencies • Aortic Dissection, Pulmonary Edema, Myocardial Ischemia/Infarction, Intracranial Hemorrhage, -

Cold Water Safety & Survival
Cold Water Safety and Survival: Volume 2 Surviving Outdoor Adventures Written by Alaska Marine Safety Education Association staff: Marian Allen, Steven Campbell, Jerry Dzugan, Dan Falvey, Michael Jones, Rick McElrath, and Shawn Newell Edited by Marian Allen, Susan Jensen, Shawn Newell, Dan Walker, and Madelyn Walker Published by University of Alaska Sea Grant Fairbanks, Alaska SG-ED-37 This publication is a product of the Alaska Marine Safety Education Association (AMSEA) whose mission is to reduce injury and the loss of life, due to drowning and hypothermia, through education and training. AMSEA is supported by the following organizations: Alaska Vocational Technical Center (AVTEC); University of Alaska Marine Advisory Program; North Pacific Fishermen’s Association; North Pacific Fisheries Observer Training Center; Alaska Native Tribal Health Consortium; Southeast Alaska Regional Health Consortium, Environmental Health; Alaska Department of Fish and Game; Petersburg Vessel Owners Association; Alaska Department of Health and Human Services, Community Health and Emergency Medical Services Section; National Institute of Occupational Safety and Health, Division of Safety Research; U.S. Coast Guard 17th District, Maritime Office of Compliance (MOC). This publication was made possible by funding from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Rural Health Outreach; the Alaska Department of Community and Regional Affairs; the Alaska Department of Health and Social Services, Division of Public Health; the Reuben E. Crossett Endowed Alaskan Fund; and the Sitka, Alaska, School District Migrant Education Program. New lesson plans and additional teaching resources can be found on AMSEA’s Web site www.amsea.org. Elmer E.