Corneal Remodeling for Refractive Errors – (0141)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Refractive Error Changes in Cortical, Nuclear and Posterior Subcapsular Cataracts
1524 Refractive error changes in cortical, nuclear and posterior subcapsular cataracts. D.B. Elliott & K. Pesudovs . Department of Optometry, University of Bradford, Bradford, United Kingdom.. Purpose • To determine the effect of the three main morphological types of age-related cataract on refractive error. Background • The increase in myopia in some patients with age-related nuclear cataract is well known (Brown & Hill, 1987). This change accounts for the “second sight of the elderly” in which the myopic shift provides normal reading ability without the need for spectacles. Distance vision, however, worsens. • Planter (1981) suggested that cortical opacity can induce hyperopic shifts. However, this claim has not been repeated since and no firm evidence is available. • Review papers suggest that cortical opacity can induce astigmatic changes (Brown, 1993). However, these reports were based on clinical impression with no supporting data. • . The prevalence of uncorrected refractive error in the elderly population is high (Wormald et al., 1992). It is likely that a reasonable proportion of these patients have refractive error changes induced by cataract. • It has been suggested that a delay in operating on age-related cataract of 10 years could reduce the number of patients requiring cataract surgery (Kupfer, 1985). The possible role of correcting cataract-induced refractive error to delay the need for surgery should be explored. Subjects • 98 elderly subjects (mean age 67 ± 8 years) were recruited. • 77 subjects had one type of morphological cataract: 34 subjects had cortical cataract, 21 had nuclear cataract and 21 had posterior subcapsular cataract (PSC). • 22 subjects had normal, healthy eyes. • Ocular screening excluded amblyopia, strabismus, eye disease or surgery. -
Development of in Vitro Corneal Models: Opportunity for Pharmacological Testing
Review Development of In Vitro Corneal Models: Opportunity for Pharmacological Testing Valentina Citi 1, Eugenia Piragine 1, Simone Brogi 1,* , Sara Ottino 2 and Vincenzo Calderone 1 1 Department of Pharmacy, University of Pisa, Via Bonanno 6, 56126 Pisa, Italy; [email protected] (V.C.); [email protected] (E.P.); [email protected] (V.C.) 2 Farmigea S.p.A., Via G.B. Oliva 6/8, 56121 Pisa, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-050-2219-613 Received: 24 October 2020; Accepted: 30 October 2020; Published: 2 November 2020 Abstract: The human eye is a specialized organ with a complex anatomy and physiology, because it is characterized by different cell types with specific physiological functions. Given the complexity of the eye, ocular tissues are finely organized and orchestrated. In the last few years, many in vitro models have been developed in order to meet the 3Rs principle (Replacement, Reduction and Refinement) for eye toxicity testing. This procedure is highly necessary to ensure that the risks associated with ophthalmic products meet appropriate safety criteria. In vitro preclinical testing is now a well-established practice of significant importance for evaluating the efficacy and safety of cosmetic, pharmaceutical, and nutraceutical products. Along with in vitro testing, also computational procedures, herein described, for evaluating the pharmacological profile of potential ocular drug candidates including their toxicity, are in rapid expansion. In this review, the ocular cell types and functionality are described, providing an overview about the scientific challenge for the development of three-dimensional (3D) in vitro models. -
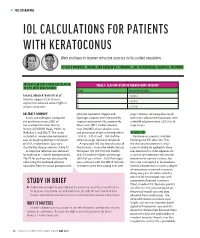
Iol Calculations for Patients with Keratoconus
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Fact Sheet: Refractive Errors
Fact Sheet: Refractive Errors More than 11 million Americans have common vision problems that can be corrected with the use of prescriptive eyewear such as glasses or contact lenses.1 These conditions are known as refractive errors and they occur when the eye doesn’t correctly bend, or ―refract,‖ light as it enters the eye. Common refractive errors include the following: o Nearsightedness (also called myopia)—A condition where objects up close appear clearly, while objects far away appear blurry. With nearsightedness, light comes to focus in front of the retina instead of on the retina. o Farsightedness (also called hyperopia)—A common type of refractive error where distant objects may be seen more clearly than objects that are near. However, people experience farsightedness differently. Some people may not notice any problems with their vision, especially when they are young. For people with significant farsightedness, vision can be blurry for objects at any distance, near or far. o Astigmatism—A condition in which the eye does not focus light evenly onto the retina, the light-sensitive tissue at the back of the eye. This can cause images to appear blurry and stretched out. o Presbyopia—An age-related condition in which the ability to focus up close becomes more difficult. As the eye ages, the lens can no longer change shape enough to allow the eye to focus close objects clearly. Refractive errors are one of the most common—and correctable—causes of visual impairment in the United States. According to a recent study led by the National Eye Institute (NEI), approximately half of all American adults don’t have the 20/20 vision physicians consider optimal due to refractive errors.2 Women experience refractive error more frequently than men: Twenty-six percent more women aged 12 and older have uncorrected visual impairment due to refractive error compared with men aged 12 and older. -

Hyperopia Hyperopia
Hyperopia Hyperopia hyperopia hyperopia • Farsightedness, or hyperopia, • Farsightedness occurs if your eyeball is too as it is medically termed, is a short or the cornea has too little curvature, so vision condition in which distant objects are usually light entering your eye is not focused correctly. seen clearly, but close ones do • Its effect varies greatly, depending on the not come into proper focus. magnitude of hyperopia, the age of the individual, • Approximately 25% of the the status of the accommodative and general population is hyperopic (a person having hyperopia). convergence system, and the demands placed on the visual system. By Judith Lee and Gretchyn Bailey; reviewed by Dr. Vance Thompson; Flash illustration by Stephen Bagi 1. Cornea is too flap. hyperopia • In theory, hyperopia is the inability to focus and see the close objects clearly, but in practice many young hyperopics can compensate the weakness of their focusing ability by excessive use of the accommodation functions of their eyes. Hyperopia is a refractive error in • But older hyperopics are not as lucky as them. By which parallel rays of light aging, accommodation range diminishes and for 2. Axial is too short. entering the eye reach a focal older hyperopics seeing close objects becomes point behind the plane of the retina, while accommodation an impossible mission. is maintained in a state of relaxation. 1 Amplitude of Accommodation hyperopia Maximum Amplitude= 25-0.4(age) • An emmetropic eye for reading and other near Probable Amplitude= 18.5-.3(age) work, at distance of 16 in (40cm), the required amount of acc. -

Improved Preservation of Human Corneal Basement Membrane
BritishJournal ofOphthalmology 1994; 78: 863-870 863 Improved preservation ofhuman corneal basement membrane following freezing of donor tissue for Br J Ophthalmol: first published as 10.1136/bjo.78.11.863 on 1 November 1994. Downloaded from epikeratophakia Robert D Young, W John Armitage, Paul Bowerman, Stuart D Cook, David L Easty Abstract States, good results continue to be achieved by Current methods for the production of the small number ofBritish surgeons performing lenticules for epikeratophakia involve rapid the technique.4 However, no comprehensive freezing, cryolathing, and slow warming of the account of its long term outcome has yet been donor cornea. We have found that this pro- published. cedure causes structural damage to the Several complications resulting in the failure epithelial basement membrane in the donor of epikeratophakia have been reported, includ- cornea which may subsequently contribute to ing infection, graft dehiscence, persistent inter- poor postoperative re-epithelialisation of the face haze or opacity, ulceration, and imperfect implant, leading to graft failure. Endeavouring re-epithelialisation. Among these, the failure of to overcome these problems, the effects of host epithelial cells to migrate over and re- cryoprotection of donor cornea were investi- surface the anterior face of the grafted tissue gated, using dimethyl sulphoxide, in conjunc- continues to be the major reason for the removal tion with different cooling and warming rates ofepikeratophakia lenticules.'-'0 as part of the protocol for cryolathing. The Epithelial healing is itselfa complex phenome- structural integrity of the epithelial basement non involving mitosis of host cells at the graft membrane zone (BMZ) was then assessed by periphery, centripetal migration, and attach- electron microscopy and by immunofluores- ment. -

Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission
Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission The use of oral doxycycline and vitamin C in the management of acute corneal hydrops: a case comparison Abstract- We compare two patients presenting to clinic with an uncommon complication of keratoconus, acute corneal hydrops. Management of the patients differs. One heals quickly, while the other has a delayed course to resolution. I. Case A a. Demographics: 40 yo AAM b. Case History i. CC: red eye, tearing, decreased VA x 1 day OS ii. POHx: (+) keratoconus OU iii. PMHx: depression, anxiety, asthma iv. Meds: Albuterol, Ziprasidone v. Scleral CL wearer for approximately 6 months OU vi. Denies any pain OS, denies previous occurrence OU, no complaints OD c. Pertinent Findings i. VA cc (CL’s)- 20/25 OD, 20/200 PH 20/60+2 OS ii. Slit Lamp 1. Inferior corneal thinning and Fleisher ring OD, central scarring OD, 2+ diffuse microcystic edema OS, Descemet’s break OS (photos and anterior segment OCT) 2. 2+ diffuse injection OS 3. D&Q A/C OU iii. Intraocular Pressures: deferred OD due to CL, 9mmHg OS (tonopen) iv. Fundus Exam- unremarkable OU II. Case B a. Demographics: 39 yo AAM b. Case History i. CC: painful, red eye, tearing, decreased VA x 1 day OS ii. POHx: unremarkable iii. PMHx: hypertension iv. Meds: unknown HTN medication v. Wears Soflens toric CL’s OU; reports previous doctor had difficulty achieving proper fit OU; denies diagnosis of keratoconus OU vi. Denies any injury OS, denies previous occurrence OU, no complaints OD c. -

Photorefractive Keratectomy for Correction of Epikeratophakia
CASE REPORTS AND SMALL CASE SERIES high myopia resulting from poste- results might be related to the pre- Photorefractive Keratectomy rior lenticonus. Postsurgical refrac- existing corneal stromal abnormali- for Correction of tion was stable for 8 years, then a ties in their patients, which were not Epikeratophakia Regression rapid myopic regression of the epi- observed in our group. Thus, PRK keratophakic lenses was observed can effectively be used to treat epi- Excimer laser photorefractive kera- the following year (Table). In- keratophakic regressed lenses in a se- tectomy (PRK) is widely used for the stead of removing the failed epikera- lected group of patients in whom correction of myopia, astigmatism, tophakic lenses, we performed PRK both the epikeratograft and the sur- and hyperopia.1,2 It has also been on the eyes. rounding cornea are clear. This used for correction of astigmatism method eliminates the need for re- after penetrating keratoplasty.3 Results. Two and a half years after moval of the epikeratograft and ex- Epikeratophakia has been used PRK, the refraction in all 4 eyes is posing the patient to the risks of suc- in the treatment of nontolerant con- stable and the epigrafts are clear. The cessive penetrating keratoplasty. tact lens keratoconous patients.4,5 Table presents the refraction and vi- The epigrafts were made from ma- sual acuity results for the eyes be- Hirsh Ami, MD chined corneal tissue that was found fore PRK and at 3 months, 1 year, Solberg Yoram, MD, PhD unsuitable for penetrating kerato- and 21⁄2 years after PRK. No haze has Cahana Michael, MD plasty. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -

Download Article (PDF)
Advances in Health Sciences Research, volume 26 2nd Bakti Tunas Husada-Health Science International Conference (BTH-HSIC 2019) Adherent Leukoma Associated with Measles: A Low Vision Case Report Giselle R. Shi1*, Dr. Maria Cecilia L. Yu1 1Centro Escolar University, *[email protected] Abstract— Objective: To assess if the patient has a and eye disorders that may lead to blindness [3-4]. low vision condition and to give proper management to The higher risks of complications are infants under the patient who has adherent leukoma associated with the age of 1, immune-compromised children and measles. Method: The patient was referred back by an adults especially pregnant woman. The common ophthalmologist to the optometrist for low vision effect of the measles virus to the eyes is the corneal assessment and management. The demographic profile damage which becomes cloudy or hazy. Infected was taken along with case history taking. Subjective children can also have measles keratitis which they examinations were performed like the distance visual acuity test, subjective refraction, binocular vision test, have excessive tearing and excessive sensitivity to visual field test, contrast sensitivity test, near vision test, light. It can also affect the retina, blood vessels and and color vision test. After that, objective examinations optic nerve. Due to scarring or swelling of the retina, like fixation, and retinoscopy was performed. Result patients may loss his or her vision. [4] and discussion: In the subjective refraction, the left eye The layers of the cornea should be transparent had -20.00Dsph with a visual acuity of 20/70-1. Near so that the cornea itself would look transparent as a visual acuity in the right eye was all 8M at 9cm without, whole. -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus.