Presentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
Emergency Nursing Program Foreword
RESOURCE MANUAL NSW HEALTH 2011 Transition to Practice Emergency Nursing Program Foreword The role of emergency nurses requires a broad level of skill and ability to meet the care needs of patients and their families. The Transition to Emergency Nursing Program is designed to support registered nurses new to the practice of emergency nursing. The Emergency Department is a fast-moving environment within which nurses can find themselves faced with a variety of challenges across a day. This program will assist them as they develop their knowledge and skills to meet these often changing care needs within the emergency setting. The program also supports a more consistent approach to transition to emergency nursing and it is anticipated will become the standard for initial entry to practice as an emergency nurse across NSW. This Resource Manual is the core document for the program and is complemented by both the Participant Workbook and the Facilitator’s Manual. Within the Emergency Department participants will be supported by staff to meet the relevant learning objectives during the 3-6 months over which this program extends. The development of the Transition to Emergency Nursing Program has been a lengthy process which reflects the commitment of emergency nurses to their area of practice and I acknowledge and thank them for their enthusiasm and work in enabling the Program to be developed. I am sure that it will have a positive impact for those nurses new to emergency nursing and to the care of patients. 1 Adjunct Professor Debra Thoms Chief Nursing and Midwifery Officer NSW Health NSW Department of Health 73 Miller Street NORTH SYDNEY NSW 2060 Tel. -

Bronson Healthcare Midwest Epic Review of Systems 10.3
Bronson HealthCare Midwest Epic Review of Systems 10.3 Constitution Endocrine Activity Change Y N Cold intolerance Y N Appetite Change Y N Heat intolerance Y N Chills Y N Polydipsia Y N Diaphoresis Y N Polyuria Y N Fatigue Y N GU Fever Y N Difficulty urinating Y N Unexpctd wt chnge Y N Dyspareunia Y N HENT Dysuria Y N Facial Swelling Y N Enuresis Y N Neck pain Y N Flank pain Y N Neck stiffness Y N Frequency Y N Ear Discharge Y N Genital Sore Y N Hearing loss Y N Hematuria Y N Ear pain Y N Menstrual problem Y N Tinnitus Y N Pelvic pain Y N Nosebleeds Y N Urgency Y N Congestion Y N Urine decreased Y N Rhinorrhea Y N Vaginal bleeding Y N Postnasal drip Y N Vaginal discharge Y N Sneezing Y N Vaginal pain Y N Sinus Pressure Y N Musc Dental problem Y N Arthralgias Y N Drooling Y N Back pain Y N Mouth sores Y N Gait problem Y N Sore throat Y N Joint swelling Y N Trouble swallowing Y N Myalgias Y N Voice Change Y N Skin Eyes Color change Y N Eye Discharge Y N Pallor Y N Eye itching Y N Rash Y N Eye pain Y N Wound Y N Last Name: ___________________________________ First Name: ______________________________________ Date of Birth: _____________________________ Today’s Date: __________________________________________ Bronson HealthCare Midwest Epic Review of Systems 10.3 Eye redness Y N Allergy/Immuno Photophobia Y N Env allergies Y N Visual disturbance Y N Food Allergies Y N Respiratory Immunocompromised Y N Apnea Y N Neurological Chest tightness Y N Dizziness Y N Choking Y N Facial asymmetry Y N Cough Y N Headaches Y N Shortness of breath Y N Light-headedness -

W10: Causes and Co-Morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30
W10: Causes and Co-morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30 Start End Topic Speakers 09:00 09:20 Phenotyping Nocturia – Judge a Book by its Cover? An-Sofie Goessaert 09:20 09:40 Sleep and Nocturia – Central Mechanisms into Business? Karlien Dhondt 09:40 10:00 Bladder and Kidney – Making the Bladder Gladder or Lowering Philip Van Kerrebroeck the Water Levels? 10:00 10:20 Questionnaire on Nocturia – to TANGO or Not to TANGO? Wendy Bower 10:20 10:30 Questions All Speaker Powerpoint Slides Please note that where authorised by the speaker all PowerPoint slides presented at the workshop will be made available after the meeting via the ICS website www.ics.org/2017/programme Please do not film or photograph the slides during the workshop as this is distracting for the speakers. Aims of Workshop Nocturia is a highly prevalent condition affecting both men and women of all ages. It is no longer a problem merely attributed to overactive bladder or benign prostate hyperplasia. There can be an impairment in one or more factors of the triad brain-kidney- bladder but also other factors such as obesity, hypertension, peripheral edema, sleep disturbance, depression, medication, etc can play a role. The objective of this workshop is to provide an overview on causes and co-morbidities of nocturia and how to identify them. Learning Objectives This workshop should allow the attendant to know the answers to following questions: 1. What physical features can help you to identify possible causes or co-morbidities of nocturia? 2. -

A 27-Month-Old Boy with Polyuria and Polydipsia
UC Davis UC Davis Previously Published Works Title A 27-Month-Old Boy with Polyuria and Polydipsia. Permalink https://escholarship.org/uc/item/8x24x4p2 Authors Lee, Yvonne Winnicki, Erica Butani, Lavjay et al. Publication Date 2018 DOI 10.1155/2018/4281217 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Hindawi Case Reports in Pediatrics Volume 2018, Article ID 4281217, 4 pages https://doi.org/10.1155/2018/4281217 Case Report A 27-Month-Old Boy with Polyuria and Polydipsia Yvonne Lee,1 Erica Winnicki,2 Lavjay Butani ,3 and Stephanie Nguyen 3 1Department of Pediatrics, Section of Endocrinology, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA 2Department of Pediatrics, Section of Nephrology, University of California, San Francisco, San Francisco, CA, USA 3Department of Pediatrics, Section of Nephrology, University of California, Davis, Sacramento, CA, USA Correspondence should be addressed to Stephanie Nguyen; [email protected] Received 16 May 2018; Accepted 1 August 2018; Published 23 August 2018 Academic Editor: Anselm Chi-wai Lee Copyright © 2018 Yvonne Lee et al. )is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Psychogenic polydipsia is a well-described phenomenon in those with a diagnosed psychiatric disorder such as schizophrenia and anxiety disorders. Primary polydipsia is differentiated from psychogenic polydipsia by the lack of a clear psychotic disturbance. We present a case of a 27-month-old boy who presented with polyuria and polydipsia. Laboratory studies, imaging, and an observed water deprivation test were consistent with primary polydipsia. -
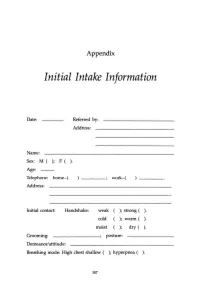
Initial Intake Information
Appendix Initial Intake Information Date: Referred by: Address: Name: Sex: M ( ); F ( ). Age: Telephone: home-( work-( Address: Initial contact: Handshake: weak ); strong ( ). cold ); warm ( ). moist ); dry ( ). Grooming: ________; posture: Demeanor/attitude: Breathing mode: High chest shallow ( ); hyperpnea ( ). 307 308 APPENDIX Sighing: frequent ( ); occasional ( ); absent ( ). Occupation: Contact with: dust ( ); fibers (); paints ( ); solvents ( ); sprays ( ); detergents ( ). Other chemicals or airborne particles: Status: Married ( ); single ( ); divorced ( ); other: children: No. Boys ( ); No. Girls ( ). Physician(s) of record: Last medical examination: _________,199__ Diagnos(e)s: 'Ireatmentts): Medication(s): Do you now have, have you ever had, or has any family member related to you by blood (mother, father, sister, brother, familial grandparents or uncles and aunts) had: ( ) High blood pressure () Heart disease APPENDIX 309 ) Low blood pressure ) Angina ) Diabetes (insulin-dependent) ) Anemia ) Diabetes (non-insulin- ) Allergies dependent) ) Dermatitis ) Colitis ) Muscle spasms ) Gastritis ) Tingling in hands and/or feet ) Ulcer ) Fainting (syncope) ) Shortness of breath ) Dizziness (vertigo) ) Asthma ) Stroke ) Emphysema ) Headache ) Hyperventilation ) TMJlbruxism ) Mitral valve prolapse ) Chronic low backache ) Other heart murmur ) EB virus (mononucl.) ) Heart arrhythmia ) PMS ) Chronic vaginal yeast ) Chronic tiredness ) Cystitis ) Menstrual irregul. ) Raynaud's disease ) Tinnitus ) Chronic pain ) Hyperthyroid ) Eating disorder -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
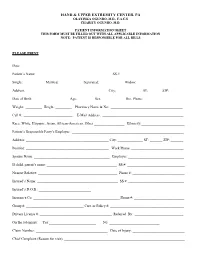
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Vitals & Assessment Bingo
Vitals & Assessment Bingo myfreebingocards.com Safety First! Before you print all your bingo cards, please print a test page to check they come out the right size and color. Your bingo cards start on Page 3 of this PDF. If your bingo cards have words then please check the spelling carefully. If you need to make any changes go to mfbc.us/e/dtfgtk Play Once you've checked they are printing correctly, print off your bingo cards and start playing! On the next page you will find the "Bingo Caller's Card" - this is used to call the bingo and keep track of which words have been called. Your bingo cards start on Page 3. Virtual Bingo Please do not try to split this PDF into individual bingo cards to send out to players. We have tools on our site to send out links to individual bingo cards. For help go to myfreebingocards.com/virtual-bingo. Help If you're having trouble printing your bingo cards or using the bingo card generator then please go to https://myfreebingocards.com/faq where you will find solutions to most common problems. Share Pin these bingo cards on Pinterest, share on Facebook, or post this link: mfbc.us/s/dtfgtk Edit and Create To add more words or make changes to this set of bingo cards go to mfbc.us/e/dtfgtk Go to myfreebingocards.com/bingo-card-generator to create a new set of bingo cards. Legal The terms of use for these printable bingo cards can be found at myfreebingocards.com/terms. -

Respiratory Failure
Respiratory Failure Phuong Vo, MD,* Virginia S. Kharasch, MD† *Division of Pediatric Pulmonary and Allergy, Boston Medical Center, Boston, MA †Division of Respiratory Diseases, Boston Children’s Hospital, Boston, MA Practice Gap The primary cause of cardiopulmonary arrest in children is unrecognized respiratory failure. Clinicians must recognize respiratory failure in its early stage of presentation and know the appropriate clinical interventions. Objectives After completing this article, readers should be able to: 1. Recognize the clinical parameters of respiratory failure. 2. Describe the respiratory developmental differences between children and adults. 3. List the clinical causes of respiratory failure. 4. Review the pathophysiologic mechanisms of respiratory failure. 5. Evaluate and diagnose respiratory failure. 6. Discuss the various clinical interventions for respiratory failure. WHAT IS RESPIRATORY FAILURE? Respiratory failure is a condition in which the respiratory system fails in oxy- genation or carbon dioxide elimination or both. There are 2 types of impaired gas exchange: (1) hypoxemic respiratory failure, which is a result of lung failure, and (2) hypercapnic respiratory failure, which is a result of respiratory pump failure (Figure 1). (1)(2) In hypoxemic respiratory failure, ventilation-perfusion (V_ =Q)_ mismatch results in the decrease of PaO2) to below 60 mm Hg with normal or low PaCO2. _ = _ (1) In hypercapnic respiratory failure, V Q mismatch results in the increase of AUTHOR DISCLOSURE Drs Vo and Kharasch fi PaCO2 to above 50 mm Hg. Either hypoxemic or hypercapnic respiratory failure have disclosed no nancial relationships can be acute or chronic. Acute respiratory failure develops in minutes to hours, relevant to this article. -

Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation
Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation. ФЕДЕРАЛЬНОЕ ГОСУДАРСТВЕННОЕ БЮДЖЕТНОЕ ОБРАЗОВАТЕЛЬНОЕ УЧРЕЖДЕНИЕ ВЫСШЕГО ОБРАЗОВАНИЯ «КУБАНСКИЙ ГОСУДАРСТВЕННЫЙ МЕДИЦИНСКИЙ УНИВЕРСИТЕТ» МИНИСТЕРСТВА ЗДРАВООХРАНЕНИЯ РОССИЙСКОЙ ФЕДЕРАЦИИ (ФГБОУ ВО КубГМУ Минздрава России) Кафедра пропедевтики внутренних болезней Department of Propaedeutics of Internal Diseases BASIC CLINICAL SYNDROMES Guidelines for students of foreign (English) students of the 3rd year of medical university Krasnodar 2020 2 УДК 616-07:616-072 ББК 53.4 Compiled by the staff of the department of propaedeutics of internal diseases Federal State Budgetary Educational Institution of Higher Education «Kuban State Medical University" of the Ministry of Healthcare of the Russian Federation: assistant, candidate of medical sciences M.I. Bocharnikova; docent, c.m.s. I.V. Kryuchkova; assistent E.A. Kuznetsova; assistent, c.m.s. A.T. Nepso; assistent YU.A. Solodova; assistent D.I. Panchenko; docent, c.m.s. O.A. Shevchenko. Edited by the head of the department of propaedeutics of internal diseases FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation docent A.Yu. Ionov. Guidelines "The main clinical syndromes." - Krasnodar, FSBEI HE KubSMU of the Ministry of Healthcare of the Russian Federation, 2019. – 120 p. Reviewers: Head of the Department of Faculty Therapy, FSBEI HE KubSMU of the Ministry of Health of Russia Professor L.N. Eliseeva Head of the Department