Bariatric Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
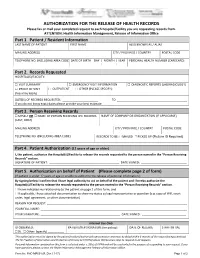
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

Outpatient Laboratory Requisition
Outpatient Laboratory All Physicians MUST include addresses ORDERING PHYSICIAN, ADDRESS, Requisition MSP PRACTITIONER NUMBER Laboratory Medicine (Anatomical Pathology requisitions - see separate form) Grey highlighted fields must be completed to avoid For tests indicated with a grey tick box F, consult provincial delays in specimen collection and patient processing. guidelines and protocols (www.BCGuidelines.ca). LOCUMLOCUM FORFOR PHYSICIAN:PHYSICIAN: Bill to: FMSP FICBC FWorkSafeBC FPATIENT FOTHER: ______________________ MSP PRACTITIONER NUMBERNUMBER:: PPHNHN NUMBENUMBERR ICBC/WorkSafeBC/RCMP NUMBER SURNAME OF PATIENT FIRSTFIRST NAME OF PATIENTPATIENT If this is a STAT order please provide contact telephone number:number: DOBDOB SEXSEX Copy to Physician/Address/MSP Practitioner Number YYYY MM DD FM FF Pregnant? FYES FNO Fasting? _________ h pc TELEPHONE NUMBER OF PATIENT CHART NUMBER ADDRESS OF PATIENT CITY/TOWN PROVINCE DIAGNOSIS CURRENT MEDICATIONS/DATE AND TIME OF LAST DOSE HEMATOLOGY URINE TESTS CHEMISTRY FHematology profile FUrine culture - list current antibiotics: FGlucose - fasting (see reverse for patient instructions) FPT-INR FOn warfarin? FGTT - gestational diabetes screen (50 g load, 1 hour post-load) FFerritin (query iron deficiency) _____________________________________________________ FGTT - gestational diabetes confirmation (75 g load, fasting, FF Macroscopic microscopic if dipstick positive 1 hour & 2 hour test) HFE - Hemochromatosis (check ONE box only) FF Macroscopic urine culture if pyuria or nitrite present FHemoglobin A1c FConfirm diagnosis (ferritin first ± TS, ± DNA testing) FF Macroscopic (dipstick) FF Microscopic FAlbumin/creatinine ratio (ACR) - urine FSibling/parent is C282Y/C282Y homozygote (DNA testing) FSpecial case (if ordered together) LIPIDS FPregnancy test 9 one bboxox ononly.ly. FForor ototherher lilipidpid iinvestigations,nvestigations, ppleaselease ororderder MICROBIOLOGY - label all specimens with patient’s first & last name, DOB and/or PHN & site specispecificfic tests below and provide diadiagnosis.gnosis. -

Vancouver Coastal Health Designated Responder Coordinators
Designated Responder Coordinators COC/Facility Program Name Title/Discipline email Main Phone North Shore Lions Gate Hospital Social Work Macdonald, Catherine Clinical Practice Leader RSW [email protected] 604-984-5905 MH & Addictions Community Psychiatric Service Wood, Karen Team Leader RPN [email protected] 604-984-5000 5145 West CHC Geriatric Outreach Program Lawrie, Richard S. Social Worker RSW [email protected] 604-904-6200 4116 Home & Community Care Chant, Susie Team Leader RN [email protected] 604-983-6700 Powell River MH & Addictions Powell River MH Team Berg, Rhonda Geriatric Community MH Nurse [email protected] 604-485-3300 4408 RPN Powell River Hospital Acute Care Curtis, Corinna Acute Services Manager RN [email protected] 604-485-3201 Thursday, January 21, 2016 Page 1 of 5 Designated Responder Coordinators COC/Facility Program Name Title/Discipline email Main Phone Providence Health Care Brock Fahrni Pavillion Residential Care Whyte, Christopher Registered Social Worker RSW [email protected] 604-806-9711 Mount St. Josephs Hospital Elder Care Robitaille, Teresa Registered Social Worker RSW [email protected] 604-874-1141 78647 St. Paul's Hospital Elder Care McMenamie, Meghan Registered Social Worker RSW [email protected] 604-806-8739 Social Work Bosma, Harvey Registered Social Worker RSW [email protected] 604-682-2344 68068 Lee, Sandra Y. Registered Social Worker RSW [email protected] 604-682-2344 63389 Richmond Home & Community Care Continuing -

Births by Facility 2015/16
Number of Births by Facility British Columbia Maternal Discharges from April 1, 2015 to March 31, 2016 Ü Number of births: Fort Nelson* <10 10 - 49 50 - 249 250 - 499 500 - 999 Fort St. John 1,000 - 1,499 Wrinch Dawson Creek 1,500 - 2,499 Memorial* & District Mills Chetwynd * ≥ 2,500 Memorial Bulkley Valley MacKenzie & 1,500-2,499 Stuart Lake Northern Prince Rupert District * Births at home with a Haida Gwaii* University Hospital Registered Healthcare Provider of Northern BC Kitimat McBride* St. John G.R. Baker Memorial Haida Gwaii Shuswap Lake General 100 Mile District Queen Victoria Lower Mainland Inset: Cariboo Memorial Port Golden & District McNeill Lions Gate Royal Invermere St. Paul's Cormorant Inland & District Port Hardy * Island* Lillooet Ridge Meadows Powell River Vernon VGH* Campbell River Sechelt Kootenay Elk Valley Burnaby Lake Squamish Kelowna St. Joseph's General BC Women's General Surrey Penticton Memorial West Coast East Kootenay Abbotsford Royal General Regional Richmond Columbian Regional Fraser Creston Valley Tofino Canyon * Peace Langley Nicola General* Boundary* Kootenay Boundary Arch Memorial Nanaimo Lady Minto / Chilliwack Valley * Regional Gulf Islands General Cowichan Saanich District Victoria 0 62.5 125 250 375 500 Peninsula* General Kilometers * Hospital does not offer planned obstetrical services. Source: BC Perinatal Data Registry. Data generated on March 24, 2017 (from data as of March 8, 2017). Number of Births by Facility British Columbia, April 1, 2015 - March 31, 2016 Facility Community Births 100 Mile -

Vancouver Coastal Health Schedule of Payments to Suppliers of Goods and Services Fiscal Year Ended March 31, 2011
Vancouver Coastal Health Schedule of Payments to Suppliers of Goods and Services Fiscal Year Ended March 31, 2011 Vendor Name Total Paid 0696277 BC LTD (CHURCHILL HOUSE) 630,612.62 0701743 BC LTD (FERN RIDGE PLACE) 96,337.10 0737912 BC LTD (DAVID HEMERKA) 80,903.66 0840738 BC LTD (SHAMIM KHAN) 45,080.00 0895577 BC LTD (GERRY LATHAM) 74,592.00 1290 HORNBY STREET LTD 1,021,226.50 18TH ST. COMMUNITY CARE SOCIETY 1,138,667.00 1921 HOLDINGS LTD 73,576.87 2450 ONTARIO ST INVESTMENTS LTD 1,202,300.24 3M CANADA COMPANY 426,762.07 4TH UTILITY INC. 256,728.23 540 ENTERPRISES LTD 49,518.00 547727 BC LIMITED (WESTMINSTER HOUSE) 421,434.00 619164 BC LTD. (ROBERT MCMASTER) 60,000.00 650600 BC LIMITED (FRANCIS HOUSE) 355,860.00 650603 BC LTD (GRANVILLE HOUSE) 242,897.00 93 LEASING LTD 286,221.22 A CRAIG & SON LTD 117,141.78 A.W. FIREGUARD SUPPLIES LTD. 64,912.31 ABBOTT DIAGNOSTICS 92,897.34 ABBOTT LABORATORIES LIMITED 506,053.81 ABBOTT VASCULAR 1,089,156.64 ABI OUTREACH SERVICES 54,218.51 ABIOMED, INC 33,372.95 ACART EQUIPMENT LIMITED 28,703.69 ACCENTUS INC 1,389,192.86 ACCESS COMMUNITY THERAPISTS LIMITED 633,714.51 ACCOUNTING ADVANTAGE 37,122.73 ACCREDITATION CANADA 270,467.70 ACCURATE POWER GROUP LTD 168,680.19 ACKLANDS - GRAINGER INC. 124,267.05 ACME VISIBLE FILING SYSTEMS LTD. 253,145.52 ADELMISH INVESTMENTS LTD 204,804.44 ADILMAN, DR STEPHEN 120,258.33 ADL CONSULTING LTD 157,191.37 ADT SECURITY SERVICES CANADA INC. -

Tier 1 (General Health Care Services) Tier 2 (Basic Stroke Services) Tier
Vancouver Coastal/ Colour Legend: Interior Health Sites Northern Health Sites Fraser Health Sites Vancouver Island Sites Providence Health Sites Chemainus Health Urgent Care Fraser Canyon Cormorant Island HCC Mission Memorial 100 Mile House District General Hospital Lady Minto Hospital Alexis Creek Health Centre Tier 1 Ladysmith Urgent Care Bella Coola Hospital Arrow Lakes Hospital CT Scanner? NO (General Health Port Alice Health Centre Pemberton Health Centre Ashcroft Hospital & CHC Care Services) Port Hardy Hospital R.W. Large Hospital Barriere Health Centre Port McNeill & District Hospital Squamish Hospital Boundary Hospital Tofino General Hospital UBC Hospital Castlegar & District CHC Chase Health Centre Clinton Health & Wellness Centre Atlin Health Centre YES Creston Valley Hospital Bulkley Valley Hospital Dr. Helmcken Memorial Hospital Chetwynd General Hospital Elkford Health Care Centre Fort Nelson Hospital Elk Valley Hospital Fraser Lake CHC Golden & District Hospital Granisle CHC Invermere & District Hospital Houston Health Centre Kaslo Primary Health Services Hudson’s Hope Health Centre Kimberley Health Centre Kitimat General Hospital Lillooett Hospital Lakes District Hospital Logan Lake Health Centre Mackenzie & District Hospital & Health Centre Nicola Valley Hospital McBride and District Hospital Princeton General Hospital Northern Haida Gwaii Hospital & Health Centre Queen Victoria Hospital Queen Charlotte City Health Centre Rock Creek Health Centre St. John Hospital Slocan CHC Stewart Health Centre South Okanagan General -

HSA HSPBA Tentative Agreement Information Meetings
HSA HSPBA Tentative Agreement Information Meetings The following information meetings are being held to help HSA members covered by the Health Science Professionals Bargaining Association collective agreement make an informed vote on the tentative agreement reached between HSPBA and HEABC. More meetings are being planned; check this site for updates. All members covered by the agreement will receive an information package, ballot, and instructions for how to vote by mail in the coming days. CHILLIWACK AREA Thursday, December 5 12:00 p.m. Chilliwack General Hospital Respiratory Rehab Office (Off elevators on 5th Floor) KAMLOOPS AREA Thursday, November 28 5:30-7:00p.m. Hotel 540 THE PEAKES ROOM 540 Victoria Street, Kamloops KELOWNA AREA Wednesday, November 27 5:30-7:00 p.m. Coast Capri Hotel VINYARD - SECTION 1 & 2 1171 Harvey Avenue, Kelowna NANAIMO AREA Tuesday, November 26 5:30-7p.m. Best Western Plus Dorchester Hotel Opera Room 70 Church Street, Nanaimo RICHMOND AREA Wednesday, December 11 12:00-2:00p.m. Richmond Hospital RALPH FISHER AUDITORIUM 7000 Westminster Highway, Richmond SURREY / LANGLEY AREA Tuesday, December 3 5:30-7:00p.m. Days Inn KING GEORGE ROOM 13373 King George Boulevard, Surrey TERRACE AREA Friday, December 6 12:00-1:00p.m. Mills Memorial Hospital - Education Room 4720 Haughland Avenue, Terrace VANCOUVER AREA Thursday, November 28 Vancouver General Hospital 12 noon - 1 p.m. Heather Pavilion Conference Room 101 Monday, December 2 5:30-7:00 p.m. Park Inn OAK ROOM 898 W. Broadway, Vancouver Wednesday, December 4 5:30pm-7:00 p.m. UBC Robson Square 800 Robson Street, Vancouver Thursday, December 5 12:00 p.m. -

What Is Palliative Care?
Supportive Palliative Care Unit Information Booklet What this Booklet is About Table of Contents This booklet is intended to be a resource to support you and your loved ones in your Hospice Palliative Care journey. This booklet About Richmond Hospital ............................. 4 will provide information about what palliative care is; Values and Principles .................................. 5 who your supportive palliative team members are, what Your Supportive Palliative Team Members ........ 6 is available to you at Richmond Hospital’s Supportive What is Palliative Care? ............................... 11 Palliative Care Unit (SPCU), what a typical day on the unit SPCU Goals ................................................ 11 would look like, personal safety, what financial expenses Palliative Care can be Delivered in you can expect, and other helpful resources. Different Settings ....................................... 12 The Layout of the SPCU ............................... 17 A Typical Day on the SPCU ........................... 20 Keeping You Safe During Your Stay on the SPCU............................................... 24 Additional Information ................................ 26 Finances .................................................... 28 What is Advance Care Planning (ACP)? ........... 29 Code Status ............................................... 30 What Happens Immediately After the Death in the Hospital? ................... 31 Funeral Services (Burial vs. Cremation) ........... 32 Organ Donation ......................................... -

Breast Biopsy Limit Any Arm Strain on the Side You Had Jim Pattison Outpatient Care 604-533-3308 the Biopsy
Care at home Locations Abbotsford-Regional Hospital 604-851-4868 Your breast will be tender and a little Medical Imaging 2nd Floor, Fraser Wing, 32900 Marshall Road, Abbotsford swollen. You might get a bruise at the BC Cancer Agency 604-877-6000 needle site. This is normal and should go Medical Imaging, 3rd Floor, 600 West 10th Ave, Vancouver Chilliwack General Hospital 604-795-4122 away within a few days. Medical Imaging, Main Floor, 45600 Menholm Rd, Chilliwack Return to your regular daily activities. Delta Hospital 604-946-1121 Medical Imaging, 5800 Mountain View Boulevard, Delta Breast Biopsy Limit any arm strain on the side you had Jim Pattison Outpatient Care 604-533-3308 the biopsy. and Surgery Centre ext. 63926 Medical Imaging, 2nd Floor, 9750 140th Street, Surrey Langley Memorial Hospital 604-533-6405 For the next 24 hours: Medical Imaging, Main Floor, 22051 Fraser Highway, Langley Wear a supportive bra. Lions Gate Hospital 604-984-5775 Place an ice pack over your bra on the Medical Imaging, Lower Level, 231 East 15th Street, North Vancouver needle site for 10 to 15 minutes at a Mount Saint Joseph Hospital 604-877-8323 Medical Imaging, Level one, 3080 Prince Edward Street, Vancouver time. Peace Arch Hospital 604-531-5512 If needed, take plain acetaminophen Medical Imaging, Main Floor, 15521 Russell Ave, White Rock (Tylenol) for pain. Powell River General Hospital 604-485-3282 Medical Imaging, 5000 Joyce Avenue, Powell River Richmond Hospital 604-278-9711 Medical Imaging, Main Floor, 7000 Westminster Hwy, Richmond When to get help Ridge Meadows Hospital 604-463-1800 Call your doctor if you have: Medical Imaging, Main Floor, 11666 Laity St., Maple Ridge Fever above 38.5°C (101°F), aches and Royal Columbian Hospital 604-520-4640 Medical Imaging, Columbia Tower, 330 E. -

Agenda General Purposes Committee MINUTES COUNCILLOR CAROL
Agenda General Purposes Committee Anderson Room, City Hall 6911 No. 3 Road Monday, March 2, 2020 4:00 p.m. Pg. # ITEM MINUTES GP-5 Motion to adopt the minutes of the meeting of the General Purposes Committee held on February 18, 2020. COUNCILLOR CAROL DAY 1. HOSPITAL PARKING (File Ref. No.) GP-14 See Page GP-14 for materials That Richmond City Council write to the Provincial Government and the Vancouver Coast Health Authority to ask the Province and Vancouver Coastal Health to provide one hour free parking for patients and family of patients at BC hospitals. GP – 1 General Purposes Committee Agenda – Monday, March 2, 2020 Pg. # ITEM COUNCILLOR MICHAEL WOLFE 2. DECLARATION OF SOLIDARITY WITH WET’SUWET’EN PEOPLE (File Ref. No.) GP-20 See Page GP-20 for materials That Council endorse the following resolution and request that Mayor and Council send a copy of to the Prime Minister of Canada, Premier of BC, Solicitor General of BC, Richmond MPs, Richmond MLAs, and member local governments of the UBCM: The City of Richmond calls on the Government of British Columbia and Canada to end any attempt at forced removal of non-violent Wet’suwet’en People from their traditional territories, suspend permits authorizing construction of the Coastal GasLink pipeline and commence good-faith consultation with the Wet’suwet’en People. ENGINEERING AND PUBLIC WORKS DIVISION 3. AWARD OF CONTRACT 6715P – TRAFFIC CONTROL SERVICES (File Ref. No. 10-6000-01) (REDMS No. 6346166 v. 5) GP-21 See Page GP-21 for full report Designated Speakers: Ben Dias & David Aarons STAFF RECOMMENDATION That Contract 6715P – Traffic Control Services be awarded for a three-year term commencing April 1, 2020, to three bidders, with the intent of assigning the majority of the work to Ansan Traffic Group as the primary service provider, and with Lane Safe Traffic Control and Traffic Pro Services serving as secondary and tertiary backup service providers. -

Inflammatory Arthritis Clinic
Other Arthritis Rehab Services CONTACT US in the Lower Mainland Inflammatory Arthritis Clinic Surrey Memorial Hospital Publicly funded arthritis clinics with Rehabilitation Department Inflammatory physiotherapy and occupational B building basement level 13750 96 Avenue Surrey B.C. V3V 1Z2 therapy include: Arthritis Clinic Mary Pack Arthritis Program Ph. 604 585 5666 ext 778778 (Vancouver) Richmond Hospital Arthritis Clinic Lions Gate Hospital Arthritis Surrey Memorial Clinic (North Vancouver) Hospital OASIS clinics for osteoarthritis (Richmond, Vancouver, North Vancouver) Burnaby Hospital Arthritis Program A doctor referral is required. Arthritis Resources The Arthritis Society: www.arthritis.ca Mary Pack Arthritis Centre: www.mpap.vch.ca www.fraserhealth.ca www.rheuminfo.com © August 2017 Rehabilitation Subtitle Subtitle Sed tellus lorem, semper id felis non, Mauris condimentum pharetra tempor dolor. Aliquam condimentum ligula, a maximus feugiat venenatis leo, at hendrerit mauris fringilla eget. Mauris nec Title of massa posuere sed. posuere nulla. In hac habitasse Sed ut sollicitudin ex. Donec fringilla platea dictumst. ante nec lectus laoreet facilisis. Ut Brochure eleifend gravida nulla, viverra laoreet Curabitur feugiat justo eget leo lectus eleifend ac. hendrerit tristique. Maecenas venenatis sollicitudin ornare. Nam Proin ut faucibus urna. at nisi a quam ornare mollis eu Subtitle nec eros. Ut ac enim vel odio Fusce at leo vulputate, finibus leo tristique pulvinar vel sed sem. quis, eleifend urna. Additional info Morbi ac purus a libero ornare Etiam magna nulla, rhoncus sed facilisis. posuere ut, tempus sed libero. Nullam id leo aliquet, tristique Nunc sit amet fringilla odio. nibh vel, sodales mi. Quisque luctus facilisis dolor, id aliquam ligula posuere quis. Quisque eu arcu rutrum, semper dui ut, egestas tellus. -

Thoracentesis
Are there any risks or complications? Locations Any time the skin is pierced or cut, there is Abbotsford-Regional Hospital 604-851-4866 Medical Imaging 2nd Floor, Fraser Wing, 32900 Marshall Road, Abbotsford a chance of infection. Other possible BC Cancer Agency 604-877-6000 complications include: Medical Imaging, 3rd Floor, 600 West 10th Ave, Vancouver - bleeding at the site Burnaby Hospital 604-434-4211 Medical Imaging, 3rd Floor, 3935 Kincaid St., Burnaby - an air leak into the chest cavity (called a Chilliwack General Hospital 604-795-4122 pneumothorax) Medical Imaging, Main Floor, 45600 Menholm Rd, Chilliwack Thoracentesis Jim Pattison Outpatient Care 604-533-3308 - bleeding into the chest cavity (called a and Surgery Centre Ext 63926 hemothorax) Medical Imaging, 2nd Floor, 9750 140th Street, Surrey - fluid in the lungs (called pulmonary Langley Memorial Hospital 604-533-6405 Medical Imaging, Main Floor, 22051 Fraser Highway, Langley edema) – a rare reaction to a large Lions Gate Hospital 604-984-5775 amount of fluid removed Medical Imaging, Lower Level, 231 East 15th Street, North Vancouver Peace Arch Hospital 604-531-5512 - trouble breathing Medical Imaging, Main Floor, 15521 Russell Ave, White Rock Powell River General Hospital 604-485-3282 When to get help Medical Imaging, 5000 Joyce Avenue, Powell River Call your doctor if you have: Richmond Hospital 604-278-9711 Medical Imaging, Main Floor, 7000 Westminster Hwy, Richmond Fever above 38.5°C (101°F), aches and Ridge Meadows Hospital 604-463-1800 chills Medical Imaging, Main Floor, 11666 Laity Street, Maple Ridge Fluid starts or continues to leak out from Royal Columbian Hospital 604-520-4640 Medical Imaging, Columbia Tower the needle site 330 East Columbia Street, New Westminster Go to the nearest Emergency Department St.