Integrating ECG Monitoring and Classification Via Iot and Deep
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Press Release
PRESS RELEASE DATE: November 2013 EMBARGO: Immediate Release Local government leaders from more than 60 communities gather in Xiamen, China, for LivCom finals Representatives of more than 60 communities from around the world will gather in Xiamen, China this week (28 November–2 December) for the finals of the International Awards for Liveable Communities (LivCom). Communities travelling to the coastal garden city of Xiamen on the south east coast of China will share experiences and expertise as well as learning more about the environmental achievements of the host city. The three-days of presentations will conclude on Monday 2nd December with a prestigious United Nations Environment Programme (UNEP) seminar. The results of the judges deliberations on the world’s most liveable communities of 2013 will be announced on Monday evening at an awards ceremony in the city. Delegates will make the case for their towns and cities before a panel of world renowned experts in the field of municipal and environmental management. A continued growth in community focus on sustainablity is seeing a rising number of entries for the awards. Finalists this year reflect a wider geographic spread than ever before with entries from across the globe. Mayor of Xiamen, Mr Liu Keqing, said: “For many years, Xiamen has been seeking harmony between society, economy and nature. The people of Xiamen are encouraged and empowered to actively participate in urban and community development. “Through its own efforts and international collaboration, Xiamen has grown into a friendly community with healthy ecological system, a livable environment, high living standards and a strong public awareness of the environment. -

Solar Radiation Estimation Algorithm and Field Verification in Taiwan
energies Article Solar Radiation Estimation Algorithm and Field Verification in Taiwan Ping-Huan Kuo 1 ID , Hsin-Chuan Chen 2 and Chiou-Jye Huang 3,* ID 1 Computer and Intelligent Robot Program for Bachelor Degree, National Pingtung University, Pingtung 90004, Taiwan; [email protected] 2 School of Computer Engineering, University of Electronic Science and Technology of China Zhongshan Institute, Zhongshan 528402, China; [email protected] 3 School of Electrical Engineering and Automation, Jiangxi University of Science and Technology, Ganzhou 341000, China * Correspondence: [email protected] Received: 5 May 2018; Accepted: 22 May 2018; Published: 29 May 2018 Abstract: The power generation potential of a solar photovoltaic (PV) power generation system is closely related to the on-site solar radiation, and sunshine conditions are an important reference index for evaluating the installation of a solar PV system. Meanwhile, the long-term operation and maintenance of a PV system needs solar radiation information as a reference for system performance evaluation. Obtaining solar radiation information through the installation of irradiation monitoring stations is often very costly, and the cost of sustaining the reliability of the monitoring system, Internet stability and subsequent operation and maintenance can often be alarming. Therefore, the establishment of a solar radiation estimation model can reduce the installation of monitoring stations and decrease the cost of obtaining solar radiation information. In this study, we use an inverse distance weighting algorithm to establish the solar radiation estimation model. The model was built by obtaining information from 20 solar radiation monitoring stations in central and southern Taiwan, and field verification was implemented at Yuan Chang Township town hall and the Tainan Liujia campus. -

List of Insured Financial Institutions (PDF)
401 INSURED FINANCIAL INSTITUTIONS 2021/5/31 39 Insured Domestic Banks 5 Sanchong City Farmers' Association of New Taipei City 62 Hengshan District Farmers' Association of Hsinchu County 1 Bank of Taiwan 13 BNP Paribas 6 Banciao City Farmers' Association of New Taipei City 63 Sinfong Township Farmers' Association of Hsinchu County 2 Land Bank of Taiwan 14 Standard Chartered Bank 7 Danshuei Township Farmers' Association of New Taipei City 64 Miaoli City Farmers' Association of Miaoli County 3 Taiwan Cooperative Bank 15 Oversea-Chinese Banking Corporation 8 Shulin City Farmers' Association of New Taipei City 65 Jhunan Township Farmers' Association of Miaoli County 4 First Commercial Bank 16 Credit Agricole Corporate and Investment Bank 9 Yingge Township Farmers' Association of New Taipei City 66 Tongsiao Township Farmers' Association of Miaoli County 5 Hua Nan Commercial Bank 17 UBS AG 10 Sansia Township Farmers' Association of New Taipei City 67 Yuanli Township Farmers' Association of Miaoli County 6 Chang Hwa Commercial Bank 18 ING BANK, N. V. 11 Sinjhuang City Farmers' Association of New Taipei City 68 Houlong Township Farmers' Association of Miaoli County 7 Citibank Taiwan 19 Australia and New Zealand Bank 12 Sijhih City Farmers' Association of New Taipei City 69 Jhuolan Township Farmers' Association of Miaoli County 8 The Shanghai Commercial & Savings Bank 20 Wells Fargo Bank 13 Tucheng City Farmers' Association of New Taipei City 70 Sihu Township Farmers' Association of Miaoli County 9 Taipei Fubon Commercial Bank 21 MUFG Bank 14 -

A New Fuzzy DEA/AHP Methodology for the Facility Layout Problem in a Fuzzy Environment
Proceedings of the 4th World Congress on Mechanical, Chemical, and Material Engineering (MCM'18) Madrid, Spain – August 16 – 18, 2018 Paper No. ICMIE 115 DOI: 10.11159/icmie18.115 A New Fuzzy DEA/AHP Methodology for the Facility Layout Problem in a Fuzzy Environment C.-K. Hu1, F.-B. Liu2, C.-F. Hu3 1Department of International Business, Kao Yuan University No. 1821, Jhongshan Rd., Lujhu, Kaohsiung, Taiwan [email protected] 2Department of Mechanical and Automation Engineering, I-Shou University No.1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung, Taiwan [email protected] 3Department of Applied Mathematics, National Chiayi University No. 300 Syuefu Rd., Chiayi, Taiwan [email protected] Extended Abstract The facility layout problem has been a subject of tremendous interest in manufacturing system. It is concerned with the allocation of activities to space such that a set of criteria is met and/or some objectives are optimized. A number of formulations have been developed for the facility layout problem. Most of them involve over simplifying assumptions and request overwhelming computational efforts such that they cannot be manipulated with ease in practice [1]. To cope with the difficulties being the cause of this complexity and the vagueness involved in the real-world decision-making problem, this work develops a novel approach combining the Tchebycheff model in fuzzy data envelopment analysis (DEA) and the analytical hierarchical process (AHP) for evaluating the facility layout problem with multiple fuzzy criteria. The hybrid fuzzy DEA/AHP approach takes the best of both fuzzy DEA and AHP methods by avoiding the pitfalls of each. -

The Study of China Student's Life Stress, Happiness And
2018-0907 IJOI http://www.ijoi-online.org/ THE STUDY OF CHINA STUDENT’S LIFE STRESS, HAPPINESS AND STUDY PERFORMANCE IN TAIWAN Doctoral Student Wen-Hao Wu Department of Business Management, National Sun-Yat sen University 70 Lienhai Rd., Kaohsiung 80424, Taiwan, R.O.C. Assistant Professor Dr. Chih-Yu Yang Department of International Business, I-Shou University No.1, Sec.1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan, R.O.C Assistant Professor Dr. Wu-Hua Chang Department of International Business, I-Shou University No.1, Sec.1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan, R.O.C Adjunct Assistant Professor Dr. Ming-Feng Wu* Department of International Business, I-Shou University No.1, Sec.1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan, R.O.C Assistant Professor Dr. Yang-Yu Ou Department of Tourism and Management, Chia Nan University of Pharmacy & Science No.60, Sec. 1, Erren Rd., Rende Dist., Tainan City 71710, Taiwan, R.O.C Assistant Professor Dr. Lu-Feng Huang Department of Leisure Management, National Pingtung University No.1 Lisen Rd., Pingtung City, Pingtung County 90003, Taiwan, R.O.C. Abstract The number of foreign student increase constantly in recently year due to Taiwan government policy and college abroad student recruitment. The major foreign stu- dents come from China. It is necessary to investigate the life stress and study per- formance of foreign student in order to strengthen the administration performance of college and export the advantage to abroad. This study has interviewed 192 china students in Case Study College in southern Taiwan. -

Press Release
PRESS RELEASE DATE: 30th September 2013 EMBARGO: Immediate Release Delegations from more than 60 communities set to gather in Xiamen, China for LivCom finals Representatives of more than 60 communities from around the world will gather in Xiamen, China, 28th November- 2nd December 2013 at the finals of the UN-backed International Awards for Liveable Communities (LivCom). Delegates will make the case for their towns and cities over four days of judging before a panel of world renowned experts in the field of municipal and environmental management. The winning communities in the global awards scheme for civic environmental achievement will be announced on Monday 2nd December. Organisers of the event, which has the support of UNEP, say a continued growth in community focus on sustainablity has sparked not only growing entries but increasing innovation in projects designed to resolve challenging issues in the spheres of socio-economic, built and natural environments. Finalists this year reflect a wide geographic spread with a growth in new communities making their debut at the finals. After a special award was made two years ago to Medillin in Colombia, for its efforts to tackle socio-economic and environmental issues linked to an historically strong drugs culture, the awards have increasingly seen the rise of progressive solutions to tackle global community problems. Founder and chief executive Alan Smith said: “We are looking forward to a highly competitive, educational and informative finals event with some of the leading innovators in the world going before the judges. “As well as sharing knowledge, these awards are a unique way of recognising the outstanding efforts being made by individuals committed to finding innovative answers to their communities problems.” A total of 42 towns and cities, 52 Sustainable Projects and six Bursary Award applications have reached the finals. -

National Level Public Officials Election-Taiwan, 2020)
Election Result By Party Votes For The 7th Direct Presidential Election (National Level Public Officials Election-Taiwan, 2020) James C.Y.Soong、Yu Xiang (PFP) Daniel K.Y.Han、Chang Shan-Zheng (KMT) TSAI,ING-WEN、Lai Qing-De (DPP) Locality Valid Votes Votes % Votes % Votes % Grand Total 14300940 608590 4.26 5522119 38.61 8170231 57.13 Taiwan Province 4207385 179061 4.26 1709221 40.62 2319103 55.12 Ilan County 274406 10739 3.91 90010 32.80 173657 63.28 Hsinchu County 325039 18435 5.67 154224 47.45 152380 46.88 Miaoli County 326601 15222 4.66 164345 50.32 147034 45.02 Changhua County 763231 35060 4.59 291835 38.24 436336 57.17 Nantou County 299152 13315 4.45 133791 44.72 152046 50.83 Yunlin County 399788 15331 3.83 138341 34.60 246116 61.56 Chia-I County 307290 11138 3.62 98810 32.16 197342 64.22 Pingtung County 511050 14021 2.74 179353 35.10 317676 62.16 Taitung County 115668 4163 3.60 67413 58.28 44092 38.12 Hualien County 185212 6869 3.71 111834 60.38 66509 35.91 Penghu County 50904 2583 5.07 20911 41.08 27410 53.85 Keelung City 226204 11878 5.25 99360 43.93 114966 50.82 Hsinchu City 261102 14103 5.40 102725 39.34 144274 55.26 Chia-I City 161738 6204 3.84 56269 34.79 99265 61.37 Taipei City 1632453 70769 4.34 685830 42.01 875854 53.65 Kaohsiung City 1763826 55309 3.14 610896 34.63 1097621 62.23 New Taipei City 2466187 112620 4.57 959631 38.91 1393936 56.52 Taichung City 1698470 84800 4.99 646366 38.06 967304 56.95 Tainan City 1167248 41075 3.52 339702 29.10 786471 67.38 Taoyuan City 1311141 63132 4.82 529749 40.40 718260 54.78 Fuchien Province -

Wearable Device for Evaluating the Effect of Training on the Performance of College Baseball Players and Indicator Construction
Sensors and Materials, Vol. 33, No. 2 (2021) 645–655 645 MYU Tokyo S & M 2484 Wearable Device for Evaluating the Effect of Training on the Performance of College Baseball Players and Indicator Construction Shih-Fu Sung,1 Yue-Yang Chen, 2* Yung-Ching Chou,3 Tsai-Pei Liu,4 and Hsien-Hung Chen5 1Department of Information Management, I-Shou University, No. 1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan 2Department of Business Administration, I-Shou University, No. 1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan 3Department of Information Engineering, I-Shou University, No. 1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan 4Department of Distribution Management, National Taichung University of Science and Technology No. 129, Sec. 3, Sanmin Rd, North District, Taichung City 404, Taiwan 5General Education Center, CTBC Business School, No. 600, Sec. 3, Taijiang Blvd., Annan District, Tainan city 709, Taiwan (Received May 29, 2019; accepted December 14, 2020) Keywords: wearable device, physical fitness, psychological state, training environment, performance indicator, competition event performance Baseball has gained popularity at Taiwanese colleges over the last twenty years. The quality of coaching and training is the key factor in the performance of young players during competition. Wireless sensor network (WSN) technology has been developed to index, navigate, store, and analyze data in sports. We investigated the correlations between the performance of college baseball players during a competition game and the following three factors: (1) athletes’ physical fitness, (2) athletes’ psychological state, and (3) the training environment. Wireless wearable devices were applied in this research to construct the indicators for monitoring the development of players in terms of the three aforementioned factors during routine training. -

The Study of Country Woman's Intention to Adopt
2020-1143 IJOI https://www.ijoi-online.org/ THE STUDY OF COUNTRY WOMAN’S INTENTION TO ADOPT AGRICULTURE IN MIDDLE TAIWAN Associate Prof. Dr. Yi-Yu Shih The Department of International Business, I-Shou University, No.1, Sec. 1, Syuecheng Rd., Dashu District., Kaohsiung County 84001, Taiwan, R.O.C. Prof. Dr. Ting-Yang Liu Graduate Institute of Human Resource and Knowledge Management, National Kaohsiung Normal University, No.116, Heping 1st Rd., Lingya District., Kaohsiung City 80201, Taiwan, R.O.C. Doctoral Student Wen-Hao Wu Department of Business Management, National Sun-Yat sen University, 70 Lienhai Rd., Kaohsiung 80424, Taiwan, R.O.C. Adjunct Assistant Professor Dr. Ming-Feng Wu* Department of International Business, I-Shou University, No.1, Sec.1, Syuecheng Rd., Dashu District., Kaohsiung City 84001, Taiwan, R.O.C *Corresponding author: [email protected] Prof. Dr. Yung-Hsiang Lu Department of Bio-Business Management, National Chiayi University, No. 580, Sinmin Rd., West Dist., Chiayi City 600, Taiwan, R.O.C. Abstract Women are an important force input in the labor market. Especially in rural areas, country women not only bear both the household and economic burden, but are also a core force significant for community development. Their presence can be seen in rural 320 The International Journal of Organizational Innovation Volume 13 Number 3, January 2021 2020-1143 IJOI https://www.ijoi-online.org/ education, children's welfare, care for the elderly, medical care, community develop- ment and other public affairs. Therefore, it is an important topic for Taiwan's agricul- tural economy and community development to understand the factors that will affect the country women's input in agricultural production, and to empower ad assist the country women. -

Welcome to the Central Bank of China
399 INSURED FINANCIAL INSTITUTIONS 2020/3/31 37 Insured Domestic Banks 5 Sanchong City Farmers' Association of New Taipei City 62 Hengshan District Farmers' Association of Hsinchu County 1 Bank of Taiwan 13 BNP Paribas 6 Banciao City Farmers' Association of New Taipei City 63 Sinfong Township Farmers' Association of Hsinchu County 2 Land Bank of Taiwan 14 Standard Chartered Bank 7 Danshuei Township Farmers' Association of New Taipei City 64 Miaoli City Farmers' Association of Miaoli County 3 Taiwan Cooperative Bank 15 Oversea-Chinese Banking Corporation 8 Shulin City Farmers' Association of New Taipei City 65 Jhunan Township Farmers' Association of Miaoli County 4 First Commercial Bank 16 Credit Agricole Corporate and Investment Bank 9 Yingge Township Farmers' Association of New Taipei City 66 Tongsiao Township Farmers' Association of Miaoli County 5 Hua Nan Commercial Bank 17 UBS AG 10 Sansia Township Farmers' Association of New Taipei City 67 Yuanli Township Farmers' Association of Miaoli County 6 Chang Hwa Commercial Bank 18 ING BANK, N. V. 11 Sinjhuang City Farmers' Association of New Taipei City 68 Houlong Township Farmers' Association of Miaoli County 7 Citibank Taiwan 19 Australia and New Zealand Bank 12 Sijhih City Farmers' Association of New Taipei City 69 Jhuolan Township Farmers' Association of Miaoli County 8 The Shanghai Commercial & Savings Bank 20 Wells Fargo Bank 13 Tucheng City Farmers' Association of New Taipei City 70 Sihu Township Farmers' Association of Miaoli County 9 Taipei Fubon Commercial Bank 21 MUFG Bank 14 -
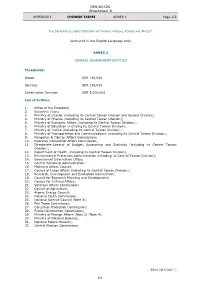
GPA/W/326 Attachment K K1
GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 1/2 THE SEPARATE CUSTOMS TERRITORY OF TAIWAN, PENGHU, KINMEN AND MATSU* (Authentic in the English Language only) ANNEX 1 CENTRAL GOVERNMENT ENTITIES Thresholds: Goods SDR 130,000 Services SDR 130,000 Construction Services SDR 5,000,000 List of Entities: 1. Office of the President; 2. Executive Yuan; 3. Ministry of Interior (including its Central Taiwan Division and Second Division); 4. Ministry of Finance (including its Central Taiwan Division); 5. Ministry of Economic Affairs (including its Central Taiwan Division); 6. Ministry of Education (including its Central Taiwan Division); 7. Ministry of Justice (including its Central Taiwan Division); 8. Ministry of Transportation and Communications (including its Central Taiwan Division); 9. Mongolian & Tibetan Affairs Commission; 10. Overseas Compatriot Affairs Commission; 11. Directorate-General of Budget, Accounting and Statistics (including its Central Taiwan Division); 12. Department of Health (including its Central Taiwan Division); 13. Environmental Protection Administration (including its Central Taiwan Division); 14. Government Information Office; 15. Central Personnel Administration; 16. Mainland Affairs Council; 17. Council of Labor Affairs (including its Central Taiwan Division); 18. Research, Development and Evaluation Commission; 19. Council for Economic Planning and Development; 20. Council for Cultural Affairs; 21. Veterans Affairs Commission; 22. Council of Agriculture; 23. Atomic Energy Council; 24. National Youth Commission; 25. National Science Council (Note 3); 26. Fair Trade Commission; 27. Consumer Protection Commission; 28. Public Construction Commission; 29. Ministry of Foreign Affairs (Note 2) (Note 4); 30. Ministry of National Defense; 31. National Palace Museum; 32. Central Election Commission. … 2014 (WT/Let/…) K1 GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 2/2 * In English only. -

High-Performance DC-AC Power Converter Using Adaptive Control Technique for Advanced Material Machining
Journal of Automation and Control Engineering Vol. 5, No. 1, June 2017 High-Performance DC-AC Power Converter Using Adaptive Control Technique for Advanced Material Machining En-Chih Chang Department of Electrical Engineering, I-Shou University, No.1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan, R.O.C. Email: [email protected] Wei Liu and Hongshu Huang Electrical Engineering and Automation, Guangzhou University, Guangzhou 510006, P.R.C. Email: [email protected], [email protected] Rong-Ching Wu Department of Electrical Engineering, I-Shou University, No.1, Sec. 1, Syuecheng Rd., Dashu District, Kaohsiung City 84001, Taiwan, R.O.C. Email: [email protected] Abstract—A high-performance DC-AC power converter possible. To obtain these requirements, proportional- using adaptive control technique for advanced material integral (PI) controller is one of the useful ways to machining (AMM) is developed in this paper. The presented achieve suitable characteristics. But, PI is difficult for technique combines the merits of hyperbolic tangential converter control to gain good steady-state and dynamic sliding surface (HTSS) and adaptive neuro-fuzzy inference response under nonlinear loads [5-8]. Many control system (ANFIS). The HTSS not only has the robustness of classic SMC but increases the system trajectory convergence techniques are also used in literature, such as mu- speed. However, once a highly nonlinear load occurs, the synthesis, H-infinity control, wavelet control, and so on chattering still exists. The chattering causes high total [9-14]. However, these techniques are complex, and harmonic distortion (THD) in DC-AC power converter difficult to realize.