D-Deprenyl PET
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Review Officer Manual
Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Substance Abuse Prevention Medical Review Officer Manual for Federal Agency Workplace Drug Testing Programs EFFECTIVE OCTOBER 1, 2010 Note: This manual applies to Federal agency drug testing programs that come under Executive Order 12564 dated September 15, 1986, section 503 of Public Law 100-71, 5 U.S.C. section 7301 note dated July 11, 1987, and the Department of Health and Human Services Mandatory Guidelines for Federal Workplace Drug Testing Programs (73 FR 71858) dated November 25, 2008 (effective October 1, 2010). This manual does not apply to specimens submitted for testing under U.S. Department of Transportation (DOT) Procedures for Transportation Workplace Drug and Alcohol Testing Programs (49 CFR Part 40). The current version of this manual and other information including MRO Case Studies are available on the Drug Testing page under Medical Review Officer (MRO) Resources on the SAMHSA website: http://www.workplace.samhsa.gov Previous Versions of this Manual are Obsolete 3 Table of Contents Chapter 1. The Medical Review Officer (MRO)........................................................................... 6 Chapter 2. The Federal Drug Testing Custody and Control Form ................................................ 7 Chapter 3. Urine Drug Testing ...................................................................................................... 9 A. Federal Workplace Drug Testing Overview.................................................................. -

Dexmethylphenidate Hydrochloride Extended-Release Capsules These
DEXMETHYLPHENIDATE HYDROCHLORIDE- dexmethylphenidate hydrochloride capsule, extended release Granules Pharmaceuticals Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION Dexmethylphenidate hydrochloride extended-release capsules These highlights do not include all the information needed to use DEXMETHYLPHENIDATE HYDROCHLORIDE EXTENDED-RELEASE CAPSULES safely and effectively. See full prescribing information for DEXMETHYLPHENIDATE HYDROCHLORIDE EXTENDED RELEASE CAPSULES. DEXMETHYLPHENIDATE HYDROCHLORIDE extended-release capsules, for oral use, CII Initial U.S. Approval: 2005 WARNING: ABUSE AND DEPENDENCE See full prescribing information for complete boxed warning. • CNS stimulants, including dexmethylphenidate hydrochloride extended-release, other methylphenidate-containing products, and amphetamines, have a high potential for abuse and dependence( 5.1, 9.2, 9.3). • Assess the risk of abuse prior to prescribing and monitor for signs of abuse and dependence while on therapy ( 5.1, 9.2). INDICATIONS AND USAGE Dexmethylphenidate hydrochloride extended-release capsules are a central nervous system (CNS) stimulant indicated for the treatment of Attention Deficit Hyperactivity Disorder (ADHD) ( 1) DOSAGE AND ADMINISTRATION • Patients new to methylphenidate: Recommended starting dose is 5 mg once daily for pediatric patients and 10 mg once daily for adults with or without food in the morning ( 2.2) • Patients currently on methylphenidate: Dexmethylphenidate hydrochloride extended-release dosage is half the current total daily dosage of methylphenidate -

'Gating' Residues Ile199 and Tyr326 in Human Monoamine Oxidase B
The ‘gating’ residues Ile199 and Tyr326 in human monoamine oxidase B function in substrate and inhibitor recognition Erika M. Milczek1,*, Claudia Binda2, Stefano Rovida2, Andrea Mattevi2 and Dale E. Edmondson1 1 Departments of Chemistry and Biochemistry, Emory University, Atlanta, Georgia, USA 2 Department of Genetics and Microbiology, University of Pavia, Italy Keywords The major structural difference between human monoamine oxidases A dipartite to monopartite cavity conversion; (MAO A) and B (MAO B) is that MAO A has a monopartite substrate inhibitor specificity; monoamine oxidase B; cavity of 550 A˚3 volume and MAO B contains a dipartite cavity struc- mutations of gating residues; structure of ture with volumes of 290 A˚3 (entrance cavity) and 400 A˚3 (substrate methylene blue complex cavity). Ile199 and Tyr326 side chains separate these two cavities in MAO Correspondence B. To probe the function of these gating residues, Ile199Ala and Ile199Ala- D. E. Edmondson, Department of Tyr326Ala mutant forms of MAO B were investigated. Structural data on Biochemistry, Emory University, 1510 the Ile199Ala MAO B mutant show no alterations in active site geometries Clifton Road, Atlanta, GA 30322, USA compared with wild-type enzyme while the Ile199Ala-Tyr326Ala MAO B Fax: +1 404 727 2738 mutant exhibits alterations in residues 100–103 which are part of the loop Tel: +1 404 727 5972 gating the entrance to the active site. Both mutant enzymes exhibit catalytic E-mail: [email protected] properties with increased amine KM but unaltered kcat values. The altered *Present address KM values on mutation are attributed to the influence of the cavity struc- Department of Chemistry, Princeton ture in the binding and subsequent deprotonation of the amine substrate. -

Selegiline) in Monkeys*
Intravenous self-administration studies with /-deprenyl (selegiline) in monkeys* /-Deprenyl and its stereoisomer d-deprenyl did not maintain intravenous self-administration behavior in rhesus monkeys. In contrast, /-methamphetamine, the major metabolite of /-deprenyl, as well as the baseline drug, cocaine, maintained high rates of intravenous self-administration behavior. Treatment with /-deprenyl doses up to 1.0 mg/kg before self-administration sessions failed to alter self-administra- tion of either cocaine or /-methamphetamine. Thus /-deprenyl did not appear to have cocaine- or meth- amphetamine-like reinforcing properties in monkeys and was ineffective in altering established patterns of psychomotor-stimulant self-administration behavior. These results support clinical findings that de- spite long-term use of /-deprenyl for the treatment of Parkinson's disease by large numbers of patients, no instances of abuse have been documented. /-Deprenyl has recently been suggested as a potential med- ication for the treatment of various types of drug abuse, including cocaine abuse, but its failure to pro- duce selective effects in decreasing cocaine or methamphetamine self-administration behavior in the present experiments makes such an application seem unlikely. (CLIN PHARMACOL THER 1994;56:774-80.) Gail D. Winger, PhD,a Sevil Yasar, MD,b'd'e S. Steven Negus, PhD,a and Steven R. Goldberg, pIli/i d'e Ann Arbor, Mich., and Baltimore, Md. From the 'Department of Pharmacology, University of Michigan /-Deprenyl (selegiline) has been known for several -

Recommended Methods for the Identification and Analysis Of
Vienna International Centre, P.O. Box 500, 1400 Vienna, Austria Tel: (+43-1) 26060-0, Fax: (+43-1) 26060-5866, www.unodc.org RECOMMENDED METHODS FOR THE IDENTIFICATION AND ANALYSIS OF AMPHETAMINE, METHAMPHETAMINE AND THEIR RING-SUBSTITUTED ANALOGUES IN SEIZED MATERIALS (revised and updated) MANUAL FOR USE BY NATIONAL DRUG TESTING LABORATORIES Laboratory and Scientific Section United Nations Office on Drugs and Crime Vienna RECOMMENDED METHODS FOR THE IDENTIFICATION AND ANALYSIS OF AMPHETAMINE, METHAMPHETAMINE AND THEIR RING-SUBSTITUTED ANALOGUES IN SEIZED MATERIALS (revised and updated) MANUAL FOR USE BY NATIONAL DRUG TESTING LABORATORIES UNITED NATIONS New York, 2006 Note Mention of company names and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. ST/NAR/34 UNITED NATIONS PUBLICATION Sales No. E.06.XI.1 ISBN 92-1-148208-9 Acknowledgements UNODC’s Laboratory and Scientific Section wishes to express its thanks to the experts who participated in the Consultative Meeting on “The Review of Methods for the Identification and Analysis of Amphetamine-type Stimulants (ATS) and Their Ring-substituted Analogues in Seized Material” for their contribution to the contents of this manual. Ms. Rosa Alis Rodríguez, Laboratorio de Drogas y Sanidad de Baleares, Palma de Mallorca, Spain Dr. Hans Bergkvist, SKL—National Laboratory of Forensic Science, Linköping, Sweden Ms. Warank Boonchuay, Division of Narcotics Analysis, Department of Medical Sciences, Ministry of Public Health, Nonthaburi, Thailand Dr. Rainer Dahlenburg, Bundeskriminalamt/KT34, Wiesbaden, Germany Mr. Adrian V. Kemmenoe, The Forensic Science Service, Birmingham Laboratory, Birmingham, United Kingdom Dr. Tohru Kishi, National Research Institute of Police Science, Chiba, Japan Dr. -
Serotonin Syndrome How to Avoid, Identify, &
Serotonin syndrome How to avoid, identify, & As the list of serotonergic agents grows, recognizing hyperthermic states and potentially dangerous drug combinations is critical to our patients’ safety. 14 Current VOL. 2, NO. 5 / MAY 2003 p SYCHIATRY Current p SYCHIATRY treat dangerous drug interactions Harvey Sternbach, MD Clinical professor of psychiatry UCLA Neuropsychiatric Institute Los Angeles, CA romptly identifying serotonin syn- drome and acting decisively can keep side effects at the mild end of the spec- Ptrum. Symptoms of this potentially dangerous syndrome range from minimal in patients starting selective serotonin reuptake inhibitors (SSRIs) to fatal in those combining monoamine oxidase inhibitors (MAOIs) with serotonergic agents. This article presents the latest evidence on how to: • reduce the risk of serotonin syndrome • recognize its symptoms • and treat patients with mild to life- threatening symptoms. WHAT IS SEROTONIN SYNDROME? Serotonin syndrome is characterized by changes in autonomic, neuromotor, and cognitive-behav- ioral function (Table 1) triggered by increased serotonergic stimulation. It typically results from pharmacodynamic and/or pharmacokinetic in- teractions between drugs that increase serotonin activity.1,2 continued VOL. 2, NO. 5 / MAY 2003 15 Serotonin Table 1 activity or reduced ability to How to recognize serotonin syndrome secrete endothelium-derived nitric oxide may diminish the System Clinical signs and symptoms ability to metabolize serotonin.2 Autonomic Diaphoresis, hyperthermia, hypertension, tachycardia, pupillary dilatation, nausea, POTENTIALLY DANGEROUS diarrhea, shivering COMBINATIONS Neuromotor Hyperreflexia, myoclonus, restlessness, MAOIs. Serotonin syndrome tremor, incoordination, rigidity, clonus, has been reported as a result of teeth chattering, trismus, seizures interactions between MAOIs— Cognitive-behavioral Confusion, agitation, anxiety, hypomania, including selegiline and insomnia, hallucinations, headache reversible MAO-A inhibitors (RIMAs)—and various sero- tonergic compounds. -

Evidence That Formulations of the Selective MAO-B Inhibitor, Selegiline, Which Bypass First-Pass Metabolism, Also Inhibit MAO-A in the Human Brain
BNL-107759-2015-JA Evidence that formulations of the selective MAO-B inhibitor, selegiline, which bypass first-pass metabolism, also inhibit MAO-A in the human brain Joanna S. Fowler1, Jean Logan2, Nora D. Volkow3,4, Elena Shumay4, Fred McCall-Perez5, Michelle Gilmor7, Millard Jayne4, Gene-Jack Wang4, David L. Alexoff1, Karen Apelskog-Torres4, Barbara Hubbard1, Pauline Carter1, Payton King1, Stanley Fahn6, Frank Telang4, Colleen Shea1, Youwen Xu1, Lisa Muench4 1Biosciences Department, Brookhaven National Laboratory, Upton, NY 11973, USA 2New York University Langone Medical Center, New York, NY 10016, USA 3National Institute on Drug Abuse, Bethesda, MD, USA 4National Institute on Alcohol Abuse and Alcoholism, Bethesda MD, USA 5Targeted Medical Pharma Inc, Los Angeles, CA 90077, USA 6Novartis Pharmaceuticals, East Hanover, NJ 07936, USA 7Neurological Institute, Columbia University, New York, NY, USA Submitted to Neuropsychopharmacology July 2014 Biological, Environmental and Climate Sciences Department Brookhaven National Laboratory U.S. Department of Energy Office of Science Office of Biological and Environmental Research Notice: This manuscript has been authored by employees of Brookhaven Science Associates, LLC under Contract No. DE-AC02-98CH10886 with the U.S. Department of Energy. The publisher by accepting the manuscript for publication acknowledges that the United States Government retains a non-exclusive, paid-up, irrevocable, world-wide license to publish or reproduce the published form of this manuscript, or allow others to do -
(12) Patent Application Publication (10) Pub. No.: US 2015/0011643 A1 Dilisa Et Al
US 2015 0011643A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0011643 A1 DiLisa et al. (43) Pub. Date: Jan. 8, 2015 (54) TREATMENT OF HEART FAILURE AND (60) Provisional application No. 61/038,230, filed on Mar. ASSOCATED CONDITIONS BY 20, 2008, provisional application No. 61/155,704, ADMINISTRATION OF MONOAMINE filed on Feb. 26, 2009. OXIDASE INHIBITORS (71) Applicants:Nazareno Paolocci, Baltimore, MD Publication Classification (US); Univeristy of Padua, Padova (IT) (51) Int. Cl. (72) Inventors: Fabio DiLisa, Padova (IT): Ning Feng, A63L/38 (2006.01) Baltimore, MD (US); Nina Kaludercic, (52) U.S. Cl. Baltimore, MD (US); Nazareno CPC ..... ... A61 K31/138 (2013.01) Paolocci, Baltimore, MD (US) USPC .......................................................... S14/651 (21) Appl. No.: 14/332,234 (22) Filed: Jul. 15, 2014 (57) ABSTRACT Related U.S. Application Data Administration of monoamine oxidase inhibitors is useful in (63) Continuation of application No. 12/407,739, filed on the prevention and treatment of heart failure and incipient Mar. 19, 2009, now abandoned. heart failure. Patent Application Publication Jan. 8, 2015 Sheet 1 of 2 US 201S/0011643 A1 Figure 1 Sial 8. Sws-L) Cleaved Š Caspase-3 ) Figure . Prevention of caspase-3 productief) fron cardiomyocytes Lapoi) reatment with clorgyi Be. Patent Application Publication Jan. 8, 2015 Sheet 2 of 2 US 201S/0011643 A1 Figure 2 8:38:8 ::::::::8: US 2015/0011643 A1 Jan. 8, 2015 TREATMENT OF HEART FAILURE AND in the art is a variety of MAO inhibitors and their pharmaceu ASSOCATED CONDITIONS BY tically acceptable compositions for administration, in accor ADMINISTRATION OF MONOAMINE dance with the present invention, to mammals including, but OXIDASE INHIBITORS not limited to, humans. -

Anticonvulsants Antipsychotics Benzodiazepines/Anxiolytics ADHD
Anticonvulsants Antidepressants Generic Name Brand Name Generic Name Brand Name Carbamazepine Tegretol SSRI Divalproex Depakote Citalopram Celexa Lamotrigine Lamictal Escitalopram Lexapro Topirimate Topamax Fluoxetine Prozac Fluvoxamine Luvox Paroxetine Paxil Antipsychotics Sertraline Zoloft Generic Name Brand Name SNRI Typical Desvenlafaxine Pristiq Chlorpromazine Thorazine Duloextine Cymbalta Fluphenazine Prolixin Milnacipran Savella Haloperidol Haldol Venlafaxine Effexor Perphenazine Trilafon SARI Atypical Nefazodone Serzone Aripiprazole Abilify Trazodone Desyrel Clozapine Clozaril TCA Lurasidone Latuda Clomimpramine Enafranil Olanzapine Zyprexa Despiramine Norpramin Quetiapine Seroquel Nortriptyline Pamelor Risperidone Risperal MAOI Ziprasidone Geodon Phenylzine Nardil Selegiline Emsam Tranylcypromine Parnate Benzodiazepines/Anxiolytics DNRI Generic Name Brand Name Bupropion Wellbutrin Alprazolam Xanax Clonazepam Klonopin Sedative‐Hypnotics Lorazepam Ativan Generic Name Brand Name Diazepam Valium Clonidine Kapvay Buspirone Buspar Eszopiclone Lunesta Pentobarbital Nembutal Phenobarbital Luminal ADHD Medicines Zaleplon Sonata Generic Name Brand Name Zolpidem Ambien Stimulant Amphetamine Adderall Others Dexmethylphenidate Focalin Generic Name Brand Name Dextroamphetamine Dexedrine Antihistamine Methylphenidate Ritalin Non‐stimulant Diphenhydramine Bendryl Atomoxetine Strattera Anti‐tremor Guanfacine Intuniv Benztropine Cogentin Mood stabilizer (bipolar treatment) Lithium Lithane Never Mix, Never Worry: What Clinicians Need to Know about -
Attendee Guidelines
(Temple of Eternal Sound) Attendee Guidelines 1. Introduction 2. Practical Guidelines -Preparation -Contraindications -Food -Clothing -Cleansing -During the Session -Suggested Best Practices -Temple Practices & Ritual Norms -Single Sacrament Sanctuary 3. Code of Ethics 4. Dietary Guidelines 5. Medical Information 6. Attendee Waiver Céu do Som Welcome, Thank you for your interest in our Forest Family Circles, Realisation Retreats and Wisdom Works at the Temple of Céu do Som & Abuelatree Sanctuary. You are endeavouring to participate in what, for us, is one of the most profound and meaningful doorways into the mysteries of the Sacred & Profound. The following pages are practical suggestions outlining our expectations, guidelines and safety measures to ensure harmony for you, for our work and for our community. We seek to uphold a high standard in regards to the safe space of transformation and realisation that may create a positive impact through healing and integration of our participants. The guidelines in this booklet all serve a direct purpose. We ask that each one be approached with due respect. It is not necessary to subscribe to our points of view in order to receive the sacrament. We do not discriminate and find that ultimately it is up to the individual to discover what is true for them. Así Céu do Som PRACTICAL GUIDELINES Preparation for the spiritual study Contraindications (refer to Medical Information section for more details) 1. If you are uncertain about any contraindications or factors please ask. 2. If you have any personal concerns a meeting can be arranged prior in order to discuss. 3. If you are taking any prescription medication, namely antidepressants, antipsychotics or SSRI's please speak to us (Refer to Medical Information section). -
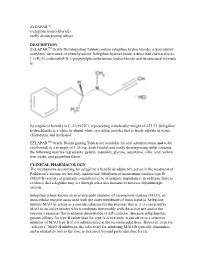
ZELAPAR™ (Selegiline Hydrochloride) Orally Disintegrating Tablets
ZELAPAR™ (selegiline hydrochloride) orally disintegrating tablets DESCRIPTION ZELAPARTM Orally Disintegrating Tablets contain selegiline hydrochloride, a levorotatory acetylenic derivative of phenthylamine. Selegiline hydrochloride is described chemically as: (-)-(R)-N, α-dimethyl-N-2-propynylphenethylamine hydrochloride and its structural formula is: Its empirical formula is C13H17N·HCl, representing a molecular weight of 223.75. Selegiline hydrochloride is a white to almost white crystalline powder that is freely soluble in water, chloroform, and methanol. ZELAPARTM Orally Disintegrating Tablets are available for oral administration (not to be swallowed) in a strength of 1.25 mg. Each lyophilized orally disintegrating tablet contains the following inactive ingredients: gelatin, mannitol, glycine, aspartame, citric acid, yellow iron oxide, and grapefruit flavor. CLINICAL PHARMACOLOGY The mechanisms accounting for selegiline’s beneficial adjunctive action in the treatment of Parkinson’s disease are not fully understood. Inhibition of monoamine oxidase type B (MAO-B) activity is generally considered to be of primary importance; in addition, there is evidence that selegiline may act through other mechanisms to increase dopaminergic activity. Selegiline is best known as an irreversible inhibitor of monoamine oxidase (MAO), an intracellular enzyme associated with the outer membrane of mitochondria. Selegiline inhibits MAO by acting as a suicide substrate for the enzyme; that is, it is converted by MAO to an active moiety which combines irreversibly with the active site and/or the enzyme’s essential flavin adenine dinucleotide (FAD) cofactor. Because selegiline has greater affinity for type B rather than for type A active sites, it can serve as a selective inhibitor of MAO type B if it is administered at the recommended dose. -

Review: Synthetic Methods for Amphetamine
Review: Synthetic Methods for Amphetamine A. Allen1 and R. Ely2 1Array BioPharma Inc., Boulder, Colorado 80503 2Drug Enforcement Administration, San Francisco, CA Abstract: This review focuses on synthesis of amphetamine. The chemistry of these methods will be discussed, referenced and precursors highlighted. This review covers the period 1985 to 2009 with emphasis on stereoselective synthesis, classical non-chiral synthesis and bio-enzymatic reactions. The review is directed to the Forensic Community and thus highlights precursors, reagents, stereochemistry, type and name reactions. The article attempts to present, as best as possible, a list of references covering amphetamine synthesis from 1900 -2009. Although this is the same fundamental ground as the recent publication by K. Norman; “Clandestine Laboratory Investigating Chemist Association” 19, 3(2009)2-39, this current review offers another perspective. Keywords: Review, Stereoselective, Amphetamine, Syntheses, references, Introduction: It has been 20 years since our last review of the synthetic literature for the manufacture of amphetamine and methamphetamine. Much has changed in the world of organic transformation in this time period. Chiral (stereoselective) synthetic reactions have moved to the forefront of organic transformations and these stereoselective reactions, as well as regio-reactions and biotransformations will be the focus of this review. Within the synthesis of amphetamine, these stereoselective transformations have taken the form of organometallic reactions, enzymatic reactions, ring openings, - aminooxylations, alkylations and amination reactions. The earlier review (J. Forensic Sci. Int. 42(1989)183-189) addressed for the most part, the ―reductive‖ synthetic methods leading to this drug of abuse. It could be said that the earlier review dealt with ―classical organic transformations,‖ roughly covering the period from 1900-1985.