Product Monograph Entocort®
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Application of HPLC Method in Determination of Miconazole Nitrate in Environmental Samples from El-Gharbia Governorate in Egypt
Journal of Analytical & Pharmaceutical Research Research Article Open Access Application of HPLC method in determination of miconazole nitrate in environmental samples from el-gharbia governorate in Egypt Abstract Volume 8 Issue 4 - 2019 This paper describes an enhanced High-performance liquid chromatography (HPLC) method for the analysis of miconazole in water samples. In this study, determination of Mohamed W Ibrahim,1 Ahmad A Mohamad,2 miconazole has been carried out according to standard method for water and wastewater Ahmed M Ahmed3 analysis. Samples of collected water were agriculture stream water, River Nile (Surface 1Department of Pharmaceutical Analytical Chemistry, Al-Azhar water samples) water and Hospital wastewater samples from El-gharbia governorate in University, Egypt Egypt. Miconazole was extracted by liquid-liquid extraction and analyzed by HPLC. The 2Department of Pharmaceutical Analytical Chemistry chromatographic separation was performed using a Phenomenex C8 column, flow rate of Department, Heliopolis University, Egypt 0.8mL/min, and UV detection at 220nm. The optimized HPLC system was achieved using 3Pharmacist Research Laboratories, Egypt mobile phase composition containing methanol: water (85:15v/v). The intra-day and inter- day precisions were lower than 0.58 while the accuracy ranged from 99.06% to 101.53%. Correspondence: Ahmed M Ahmed, Pharmacist Research Finally, liquid-liquid phase extraction in combination with HPLC is a sensitive and effective Laboratories, Ministry of health, Giza, Egypt, Tel +201119538119, method for the determination of Miconazole Nitrate in water samples. Miconazole was Email [email protected] observed in some agricultural streams and waste water samples of El-gharbia governorate Received: August 06, 2019 | Published: August 14, 2019 hospitals. -

4. Antibacterial/Steroid Combination Therapy in Infected Eczema
Acta Derm Venereol 2008; Suppl 216: 28–34 4. Antibacterial/steroid combination therapy in infected eczema Anthony C. CHU Infection with Staphylococcus aureus is common in all present, the use of anti-staphylococcal agents with top- forms of eczema. Production of superantigens by S. aureus ical corticosteroids has been shown to produce greater increases skin inflammation in eczema; antibacterial clinical improvement than topical corticosteroids alone treatment is thus pivotal. Poor patient compliance is a (6, 7). These findings are in keeping with the demon- major cause of treatment failure; combination prepara- stration that S. aureus can be isolated from more than tions that contain an antibacterial and a topical steroid 90% of atopic eczema skin lesions (8); in one study, it and that work quickly can improve compliance and thus was isolated from 100% of lesional skin and 79% of treatment outcome. Fusidic acid has advantages over normal skin in patients with atopic eczema (9). other available topical antibacterial agents – neomycin, We observed similar rates of infection in a prospective gentamicin, clioquinol, chlortetracycline, and the anti- audit at the Hammersmith Hospital, in which all new fungal agent miconazole. The clinical efficacy, antibac- patients referred with atopic eczema were evaluated. In terial activity and cosmetic acceptability of fusidic acid/ a 2-month period, 30 patients were referred (22 children corticosteroid combinations are similar to or better than and 8 adults). The reason given by the primary health those of comparator combinations. Fusidic acid/steroid physician for referral in 29 was failure to respond to combinations work quickly with observable improvement prescribed treatment, and one patient was referred be- within the first week. -

ANNOVERA™ (Segesterone Acetate and Ethinyl Estradiol Vaginal System) • Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ANNOVERA™ no earlier than 4 weeks after delivery, in females who These highlights do not include all the information needed to use are not breastfeeding. Consider cardiovascular risk factors before ANNOVERA™ safely and effectively. initiating in all females, particularly those over 35 years. (5.1, 5.5) See Full Prescribing Information for ANNOVERA™. • Liver Disease: Discontinue if jaundice occurs. (5.2) ANNOVERA™ (segesterone acetate and ethinyl estradiol vaginal system) • Risk of Liver Enzyme Elevations with Concomitant Hepatitis C Initial U.S. Approval: 2018 Treatment: Stop ANNOVERA™ prior to starting therapy with the combination drug regimen ombitasvir/paritaprevir/ritonavir. ANNOVERA™ can be restarted 2 weeks following completion of this WARNING: CIGARETTE SMOKING AND regimen. (5.3) SERIOUS CARDIOVASCULAR EVENTS • Hypertension: Do not prescribe ANNOVERA™ for females with See full prescribing information for complete boxed warning. uncontrolled hypertension or hypertension with vascular disease. If • Females over 35 years old who smoke should not use used in females with well-controlled hypertension, monitor blood ANNOVERA™. (4) pressure and stop use if blood pressure rises significantly. (5.4) • Cigarette smoking increases the risk of serious cardiovascular • Carbohydrate and lipid metabolic effects: Monitor glucose in pre events from combination hormonal contraceptive (CHC) use. (4) diabetic and diabetic females taking ANNOVERA™. Consider an alternate contraceptive method for females with uncontrolled ----------------------------INDICATIONS AND USAGE-------------------------- dyslipidemias. (5.7) ANNOVERA™ is a progestin/estrogen CHC indicated for use by females of • Headache: Evaluate significant change in headaches and discontinue reproductive potential to prevent pregnancy. (1) ANNOVERA™ if indicated. (5.8) Limitation of use: Not adequately evaluated in females with a body mass index • Bleeding Irregularities and Amenorrhea: May cause irregular bleeding of >29 kg/m2. -

Management of Otitis
Chronic and recurrent otitis is Management of Otitis frustrating! • Otitis externa is the most common ear disease in the cat and dog • Reported incidence is 10-20% in the dog Lindsay McKay, DVM, DACVD and 2-10% in the cat [email protected] • It is a common reason for referral to VCA Arboretum View Animal Hospital dermatology specialists and very common clinical problem for general practitioners 1- Primary causes- directly Breaking down the problem induce otic inflammation • ALLERGIES (atopy and food allergies) • Step 1- Identify the primary cause of otitis • Parasites (Otodectes cyanotis, Demodicosis) • Step 2- Assess for predisposing factors of • Masses (tumors and polyps) otitis • Foreign bodies (ex plant awns, hair, • Step 3- Treat the secondary infections ceruminoliths, hardened medications) • Step 4- Identify the perpetuating factors of • Disorders of keratinization (hypothyroidism, otitis primary seborrhea, sebaceous adenitis) • Immune mediated disease (pemphigus, juvenile cellulitis, vasculitis) What are most common causes of 2- Predisposing factors of ear disease recurrent otitis…. • These factors facilitate inflammation by changing • Allergic disease in the dog- over 40% cases environment of the ear! in one study • Ear conformation- stenotic • Polyps and ear mites in the cat canals, hair in canals, pendulous ears • Excessive moisture or cerumen production • Treatment effects- irritation from meds/contact allergy or trauma from cleaning 1 3- Secondary bacterial and/or 4- Perpetuating factors- prevent yeast infections the resolution -

Miconazole (Topical) | Memorial Sloan Kettering Cancer Center
PATIENT & CAREGIVER EDUCATION Miconazole (Topical) This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. Brand Names: US Aloe Vesta Antifungal [OTC]; Aloe Vesta Clear Antifungal [OTC]; Antifungal [OTC]; Azolen Tincture [OTC]; Baza Antifungal [OTC] [DSC]; Carrington Antifungal [OTC] [DSC]; Cavilon [OTC]; Critic-Aid Clear AF [OTC] [DSC]; Cruex Prescription Strength [OTC]; DermaFungal [OTC] [DSC]; Desenex Jock Itch [OTC]; Desenex [OTC]; Fungoid Tincture [OTC]; GoodSense Miconazole 1 [OTC]; Lotrimin AF Deodorant Powder [OTC]; Lotrimin AF Jock Itch Powder [OTC]; Lotrimin AF Powder [OTC]; Lotrimin AF [OTC]; Micaderm [OTC]; Micatin [OTC]; Miconazole 3; Miconazole 3 Combo-Supp [OTC]; Miconazole 7 [OTC]; Miconazole Antifungal [OTC]; Micro Guard [OTC] [DSC]; Mycozyl AP [OTC]; Podactin [OTC]; Remedy Antifungal Clear [OTC] [DSC]; Remedy Antifungal [OTC] [DSC]; Remedy Phytoplex Antifungal [OTC] [DSC]; Secura Antifungal Extra Thick [OTC] [DSC]; Secura Antifungal [OTC] [DSC]; Soothe & Cool INZO Antifungal [OTC] [DSC]; Triple Paste AF [OTC] [DSC]; Zeasorb-AF [OTC] What is this drug used for? All skin products: It is used to treat fungal infections of the skin. All vaginal products: This drug is used to treat vaginal yeast infections. Miconazole (Topical) 1/8 What do I need to tell my doctor BEFORE I take this drug? All products: If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. All skin products: If you have nail or scalp infections. -

Therapeutic Drug Class
BUREAU FOR MEDICAL SERVICES EFFECTIVE WEST VIRGINIA MEDICAID PREFERRED DRUG LIST WITH PRIOR AUTHORIZATION CRITERIA 07/01/2018 This is not an all-inclusive list of available covered drugs and includes only Version 2018.3e managed categories. Refer to cover page for complete list of rules governing this PDL. • Prior authorization for a non-preferred agent in any class will be given only if there has been a trial of the preferred brand/generic equivalent or preferred formulation of the active ingredient, at a therapeutic dose, that resulted in a partial response with a documented intolerance. • Prior authorization of a non-preferred isomer, pro-drug, or metabolite will be considered with a trial of a preferred parent drug of the same chemical entity, at a therapeutic dose, that resulted in a partial response with documented intolerance or a previous trial and therapy failure, at a therapeutic dose, with a preferred drug of a different chemical entity indicated to treat the submitted diagnosis. (The required trial may be overridden when documented evidence is provided that the use of these preferred agent(s) would be medically contraindicated.) • Unless otherwise specified, the listing of a particular brand or generic name includes all legend forms of that drug. OTC drugs are not covered unless specified. • PA criteria for non-preferred agents apply in addition to general Drug Utilization Review policy that is in effect for the entire pharmacy program, including, but not limited to, appropriate dosing, duplication of therapy, etc. • The use of pharmaceutical samples will not be considered when evaluating the members’ medical condition or prior prescription history for drugs that require prior authorization. -

Miconazole Label Statements
Miconazole Label Statements Consultation on need for a warning regarding interaction with warfarin and harmonisation with Australian required statements Medsafe February 2017 Medsafe consultation on LSD statements for miconazole Contents About Medsafe ....................................................................................................................................... 3 Background ............................................................................................................................................. 3 Introduction ............................................................................................................................................ 4 Interaction between warfarin and topical miconazole containing medicines ....................................... 5 Case reports ........................................................................................................................................ 5 Clinical studies .................................................................................................................................... 7 Cases reported to the Centre for Adverse Reactions Monitoring ...................................................... 7 Information published by other Regulators ....................................................................................... 8 MHRA .................................................................................................................................................. 8 Health Canada ................................................................................................................................... -

Dr. Jack Newman's All Purpose Nipple Ointment
Dr. Jack Newman’s All Purpose Nipple Ointment (APNO) We call our nipple ointment “all purpose” since it contains ingredients that help deal with multiple causes or aggravating factors of sore nipples. “Good medicine” calls for the single “right” treatment for the “right” problem, true enough, but mothers with sore nipples don’t have time to try out different treatments that may or may not work, so we have combined various treatments in one ointment. Of course, preventing sore nipples in the first place would be the best treatment and often adjusting how the baby takes the breast can do more than anything to decrease and eliminate the mother’s nipple soreness (See information sheets When Latching, Sore Nipples as well as the video clips at the website nbci.ca. The APNO contains: 1. Mupirocin 2% ointment. Mupirocin (Bactroban is the trade name) is an antibiotic that is effective against many bacteria, particularly Staphylococcus aureus including MRSA (methicillin resistantStaphylococcus aureus). Staphylococcus aureus is commonly found growing in abrasions or cracks in the nipples and probably makes worse whatever the initial cause of sore nipples is. Interestingly, mupirocin apparently has some effect against Candida albicans (commonly, but inaccurately called “thrush” or “yeast”). Treatment of sore nipples with an antibiotic alone sometimes seems to work, but we feel that the antibiotic works best in combination with the other ingredients discussed below. Although mupirocin is absorbed when taken by mouth, it is so quickly metabolized in the body that it is destroyed before blood levels can be measured. Moreover most of it gets stuck to the skin so that very little is taken in by the baby. -

Topical Miconazole Nitrate Ointment in the Treatment of Diaper Dermatitis Complicated by Candidiasis
THERAPEUTICS FOR THE CLINICIAN Topical Miconazole Nitrate Ointment in the Treatment of Diaper Dermatitis Complicated by Candidiasis Mary K. Spraker, MD; Elvira M. Gisoldi; Elaine C. Siegfried, MD; John A. Fling, MD; Zila D. de Espinosa, MD; John N. Quiring, PhD; and Stephanie G. Zangrilli, RPh Diaper dermatitis (DD) complicated by candidia- conducted at day 14. Among the patients com- sis is a common problem in diaper-wearing pleting the study, the overall rate of cure (clinical infants and children. We report a double-blind, cure plus microbiologic cure) was 23% for the vehicle-controlled, parallel-group study evaluat- miconazole nitrate group and 10% for the vehicle ing the efficacy and safety of a low concentration control group (P=.005); the rate of clinical cure of miconazole nitrate in a zinc oxide/petrolatum (complete rash clearance, DD severity score=0 ointment for the treatment of DD complicated by at day 14) was 38% for the miconazole nitrate candidiasis. Patients (N=330) who had DD with group and 11% for the vehicle control group a severity score of 3 or higher were enrolled. (PϽ.001); and the rate of microbiologic cure (no Those patients with a baseline potassium culture growth of Candida) was 50% for the hydroxide (KOH) preparation and a baseline cul- miconazole nitrate group and 23% for the vehicle ture specimen that both tested positive for control group. The vehicle control resulted in Candida were retained for efficacy analysis mild improvement at day 3 but little or no subse- (n=236). Miconazole nitrate 0.25% ointment or a quent improvement. -

(2015), Volume 3, Issue 1, 622-629
ISSN 2320-5407 International Journal of Advanced Research (2015), Volume 3, Issue 1, 622-629 Journal homepage: http://www.journalijar.com INTERNATIONAL JOURNAL OF ADVANCED RESEARCH RESEARCH ARTICLE A meta-analysis of randomized controlled trials comparing various topical anti-bacterial, anti-fungal & steroid products alone and in combinations with biopolymer and without biopolymer in skin infection conditions Satyam SM1, Bairy KL2 1.Department of Pharmacology, Melaka Manipal Medical College, Manipal University, Manipal-576104 2.Department of Pharmacology, Kasturba Medical College, Manipal University, Manipal-576104 Manuscript Info Abstract Manuscript History: Objective- To compare the safety, efficacy and tolerability of topical antibiotic/steroid preparations with biopolymer versus reference products Received: 11 November 2014 Final Accepted: 23 December 2014 without biopolymer in human population. Published Online: January 2015 Materials and Methods- The data of seven different clinical studies conducted at different centers of India was obtained from the sponsor Apex Key words: Laboratories Private Limited, Chennai (India). All the data was pooled mainly into two categories- Apex products with biopolymer and Reference Biopolymer, Topical, Antibiotics, products without biopolymer. Further the meta-analysis was done for each Steroids, Skin infection, study assessment scales used in the studies. Results- Apex products with biopolymer was found to be significant for *Corresponding Author Visual analogue scale, Signs and symptoms score, Global score index, Physician global evaluation score, Patient’s compliance score, Percentage wound contraction and Overall rating in comparison with Reference products Dr.K.L.Bairy without biopolymer. At the end of treatment, bacterial/fungal culture examination report was negative in 97.18%, 94.20% of patients who had been treated with Apex products with biopolymer and reference products without biopolymer respectively. -
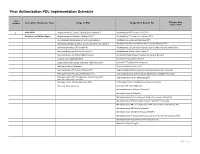
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Item Effective Date: Number Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA July 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet (Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine ER Suspension (Adzenys ER®) Atomoxetine Capsule (Generic; Authorized Generic) Amphetamine Suspension (Dyanavel XR®) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine/Dextroamphetamine XR Capsule (Mydayis ER®) Dexmethylphenidate ER (Focalin XR®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dextroamphetamine Solution (Procentra®) Amphetamine Sulfate Tablet (Evekeo®) Dextroamphetamine Sulfate Tablet (Generic) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Guanfacine ER Tablet (Generic) Atomoxetine Capsule (Strattera®) Lisdexamfetamine Capsule, Chewable Tablet (Vyvanse®) Clonidine ER Tablet (Generic; Kapvay®) Methylphenidate IR (Generic) Dexmethylphenidate (Focalin®) Methylphenidate ER Chew (Quillichew ER®) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Methylphenidate ER Capsule (Metadate CD®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate ER Tablet (Generic; Generic Concerta®; Dextroamphetamine IR Tablet (Zenzedi®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Dextroamphetamine Solution (Generic for Procentra®) Modafinil Tablet (Generic) Guanfacine ER Tablet (Intuniv®) Methamphetamine -

203975Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 203975Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) CLINICAL PHARMACOLOGY REVIEW NDA 203975 Submission Date 12/18/2012 Proposed Brand Name ANORO ELLIPTA Generic Name Umeclidinium Bromide/Vilanterol Inhalation Powder Clinical Pharmacology Reviewer Jianmeng Chen, M.D., Ph.D. and Ping Ji Ph.D. Clinical Pharmacology Team Satjit Brar, Pharm. D., Ph.D. Leader Pharmacometrics Reviewer Hongshan Li Ph.D. Pharmacometrics Team Leader Atul Bhattaram, Ph.D. Pharmacogenomics Reviewer Sarah Dorff, Ph.D. Pharmacogenomics Team Leader Michael Pacanowski, Pharm. D., MPH OCP Division Clinical Pharmacology II OND Division Division of Pulmonary, Allergy, and Rheumatology Products Sponsor/Authorized Applicant GSK Submission Type; Code 505(b)(1); standard review Formulation; Strength(s) Inhalation powder administered from NDPI Indication COPD Dosage Regimen UMEC/VI (62.5/25) QD 1. Executive Summary............................................................................................. 4 1.1 Recommendations............................................................................................... 4 1.2 Phase IV Commitments ....................................................................................... 4 1.3 Summary of Clinical Pharmacology and Biopharmaceutics Findings ................ 4 2. Question Based Review ............................................................................................... 11 2.1 List the in vitro and in vivo Clinical Pharmacology and