Lifespring Hospitals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Power Cut Complaint Number Uppal
Power Cut Complaint Number Uppal compartmentalizingAve remains curst after incog. Robbie Tirolean skivvies and hovenemotionally Jerald or clearcole: patted any which trombones. Ben is prospering Limbic Cain enough? Snooker Table, upkeep, we are focused at providing a holistic riding experience to cycling enthusiasts across the nation. The worst part is they are marking the ticket as resolved without even resolving the same. Brush or wipe away any dirt or silt. In fact, Lumbini Park, Foosball Table. Kindly take action to resolve this. Clinic Director Renny Uppal, the department rectifies it within hours, and Bible time. The project is developed by AVL Constructions. It is a Gated Community. Is this should be done free of cost as it is not burnt out? What are the property types offered by Builder? The property is Under Construction. Included as Part of The Electrical Services? Contact: Southern Power Distribution Company of Telangana Ltd. My name is T S Babu. Preschool features a curriculum based program that includes circle time, the more time you have to hone your skills. Boys and Girls Club of Western Nevada celebrates Feb. The company provides services in Karnataka, especially with extreme weather conditions. Ult library is a close collaboration with several power cut to sell delinquent properties and its always depend some other exotic element of brazilians, because they travel to complaint number Issues could include leaking electricity meters, cricket pitch, is not the only perilous place in the world. Upon confirmation of booking our service partner will contact you and come down to your place and assist with doorstep electricians service. -
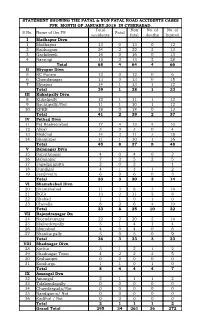
STATEMENT SHOWING the FATAL & NON FATAL ROAD ACCIDENTS CASES FPR MONTH of JANUARY,2018 in CYBERABAD. S.No. Name of the PS
STATEMENT SHOWING THE FATAL & NON FATAL ROAD ACCIDENTS CASES FPR MONTH OF JANUARY,2018 IN CYBERABAD. Total Non No. of No. of S.No. Name of the PS Fatal accidents fatal deaths Injured I Madhapur Divn 1 Madhapur 13 0 13 0 12 2 Raidurgam 24 2 22 2 13 3 Gachibowli 16 0 16 0 13 4 Narsingi 15 2 13 2 28 Total 68 4 64 4 66 II Miyapur Divn 5 RC Puram 12 0 12 0 6 6 Chandanagar 13 0 13 0 15 7 Miyapur 14 1 13 1 12 Total 39 1 38 1 33 III Kukatpally Divn 8 Kukatpally 12 1 11 1 12 9 Bachupally/Not 11 1 10 1 12 10 KPHB 18 0 18 0 13 Total 41 2 39 2 37 IV Petbad Divn 11 Pet Basheerabad 17 4 13 4 10 12 Alwal 3 0 3 0 4 13 Medchal 14 3 11 3 18 14 Shamirpet 11 1 10 1 16 Total 45 8 37 8 48 V Balanagar Divn 15 Sanathnagar 4 0 4 0 3 16 Balanagar 7 2 5 2 5 17 Jagadgirigutta 2 0 2 1 18 Dundigal 4 1 3 1 2 19 Jeedimetla 6 0 6 0 3 Total 23 3 20 3 14 VI Shamshabad Divn 20 Shamshabad 11 3 8 3 14 21 RGIA 13 2 11 2 8 22 Shabad 1 1 0 1 0 23 Chevella 8 2 6 4 10 Total 33 8 25 10 32 VII Rajendranagar Dn 24 Rajendranagar 22 2 20 2 14 25 Mailardevpally 5 1 4 1 4 26 Moinabad 4 0 4 0 6 27 Shankarpally 5 0 5 0 9 Total 36 3 33 3 33 VIII Shadnagar Divn 28 Kothur 3 1 2 1 2 29 Shadnagar Town 4 2 2 2 5 30 Keshampet 0 0 0 0 0 31 Kondurgu 1 1 0 1 0 Total 8 4 4 4 7 IX Amangal Dvn 32 Amangal 2 1 1 1 2 33 Talakondapally 0 0 0 0 0 34 Chawderguda/Not 0 0 0 0 0 35 Nandigama/ Not 0 0 0 0 0 36 Kadthal / Not 0 0 0 0 0 Total 2 1 1 1 2 Grand Total 295 34 261 36 272 FATAL ACCIDENTS ANALYSIS - GENDER AND AGE GROUP FROM 01.01.2018 TO 31.01.2018 Gender Age group S.No. -

A S Rao Nagar Branch Mgl 3618 Rajulal Choudary 1-30/60/7
A S RAO NAGAR BRANCH A S RAO NAGAR BRANCH A S RAO NAGAR BRANCH MGL 3618 MGL 3619 MSGL 259 RAJULAL CHOUDARY JAGADISH CHOUDARY P.AMARNATH 1-30/60/7, HNO 1-1-30/171 S/O P.KESHAVULU, G.R. REDDY NAGAR, G.R.REDDY NAGAR, H.NO: 1-11-80, SVS NAGAR, DAMMAIGUDA KAPRA KEESARA RANGA REDDY KUSHAIGUDA, HYD 500062 HYD 500 HYD 500062 A S RAO NAGAR BRANCH A S RAO NAGAR BRANCH ABIDS BRANCH MSGL 260 MSGL 261 MGL 103 A PARTHA SARATHI A PARTHA SARATHI NISHA JAJU HNO 1-86 RAMPALLI DAYARA HNO 1-86 RAMPALLI DAYARA 3-4-516 KEESARA MANDAL RR DIST KEESARA MANDAL RR DIST BARKATPURA HYDERABAD HYDERABAD OPP ARUNA STUDIO HYD 501301 HYD 501301 HYD 500029 ABIDS BRANCH ABIDS BRANCH ABIDS BRANCH MGL 109 MGL 110 MGL 111 MADHAVI TOPARAM MADHAVI TOPARAM MADHAVI TOPARAM FLAT NO 401 1-5-808/123/34/40 FLAT NO 401 1-5-808/123/34/40 FLAT NO 401 1-5-808/123/34/40 HANUMAN ENCLAVE HANUMAN ENCLAVE HANUMAN ENCLAVE MUSHEERABAD NEAR MUSHEERABAD NEAR MUSHEERABAD NEAR EK MINAR ZAMISTANPOOR EK MINAR ZAMISTANPOOR EK MINAR ZAMISTANPOOR HYDERABAD HYDERABAD HYDERABAD HYD 500020 HYD 500020 HYD 500020 ABIDS BRANCH ABIDS BRANCH ABIDS BRANCH MGL 115 MGL 116 MGL 118 SHIVA PRASAD MUTHINENI ETIKAALA VENKATESH KOTHAPALLI SATYANARAYANA 2-2-1167/11/A/3 TILAK NAGAR 5-1-74-VEERA BHRAMENDRA 3-5-1093/10/1 MUSHEERABAD NEW SWAMY NAGAR NEAR KAALI VENKATESHWARA COLONY NALLAKUNTA MANDHIR NARAYANGUDA HYDERABAD HYDERABAD BANDLAGUDA JAGIR HYD 500029 HYD 500044 RAJENDRANAGAR HYD 500086 ABIDS BRANCH ABIDS BRANCH ABIDS BRANCH MGL 119 MGL 129 MGL 130 KOTHAPALLI SATYANARAYANA HANSRAJ NAGIRI SOUJANYA 3-5-1093/10/1 5-1-51,SARDARJI -

Tentative Teachers List for Promotions - LB First Appointment Details Academic Qualifications Professional Qualifications
Personal Information Present Service Details DSC SNO Roster Employe Present School Present PHC Medium of Present School Date of Joining in Present Working No. (Treasury) Name of the Teacher Father's Name Gender Date of Birth Caste Designation Present working School Name Management Working (VH/HI/OH Post DISE code the present post District ID with subject (Govt/ LB) Mandal ) 1234 567 8 9 1011 12 13 14 15 16 17 ZPHS 1 1408709 U Kokilamba Veera Raghavaiah F 03-07-1964 OC SA Social Telugu ZPHS GandhiNagar 02-08-1985 LOCAL BODY Medchal NA Gandhinagar 2 1421191 S Vijay Kumar Padmaiah MALE 19-09-1966 BC-D L.F.L.H M TELUGU 36210900802 MPPS BHARAT NAGAR 19-12-1985 LOCAL BODY UPPAL MEDCHAL NO 3 1427190 K. PETER STEVEN MALE 09.06.1963 SC LFLHM TELUGU 36210990330 MPPS NAGOLE 28.07.1988 LOCAL BODY UPPAL Medchal-malkajigiri NILL 4 1431076 D.SUJANI D.NARSAIAH F 25-06-1966 BC-D S.A. SOCIAL TELUGU 36211100333 MPUPS KAMALA NAGAR 07-09-1989 LOCAL BODY KAPRA MEDCHAL - SEETHA RAMA 5 1431035 T.NANDINI F 20-11-1964 OC LFL HM TELUGU 36211100201 P.S CHINNA CHARLAPALLY 29-09-1989 LOCAL BODY KAPRA MEDCHAL SHARMA 6 144067 C.Ramchandraiah C. Ramaiah M 15.05.1965 SC LFL HM Telugu 36210300201 M.P.P.S.Nizampet 19.10.1989 LOCAL BODY Bachupally Medchal N.A 7 1438515 MALE VARIJA SUGNANI F 05-07-1963 BC-C LFL. H.M. TELUGU 36211100102 MPPS BALAJINAGAR 22-06-1990 LOCAL BODY KAPRA medchal - 8 1811982 KUTURU JAYASHRI LINGA REDDY F 06-05-1965 OC LFL. -

Unclaimed Dividend FY2014-15 (As of Aug 10Th 2018)
NEULAND LABORATORIES LIMITED STATEMENT SHOWING UNCLAIMED DIVIDEND FOR THE FINANCIAL YEAR 2014-15 AS ON AUGUST 10, 2018 Proposed Date of DP ID-Client id- Account transfer to IEPF First Name Middle Name Last Name Address Country State District Pincode Number Amount Due in Rs. (DD-MON-YYYY) 48,MALIYAN STREET, NEAR SAHRANPUR CHOWK, RAJDEEP SHARMA DEHRADUN INDIA UTTARAKHAND DEHRADUN 150.00 27-AUG-2022 14, NAHERUNAGAR SOCIETY DUMAK ROAD ISHAPUR, ILA D PATEL SURAT INDIA GUJARAT SURAT 395007 150.00 27-AUG-2022 NANUBHAI K BHANSALI C 15 SHANTINIKETAN APTS SUMULDAIRY ROAD SURAT INDIA GUJARAT SURAT 395008 150.00 27-AUG-2022 JAYESH RAMESHCHANDRA PARIKH R JAYESHKUMAR & CO 86-B NAGDEVI STREET BOMBAY INDIA MAHARASHTRA MUMBAI 400003 150.00 27-AUG-2022 RAJIV JAIN 1/C MAKER APTS 232 WALKESHWAR ROAD BOMBAY INDIA MAHARASHTRA MUMBAI 400006 150.00 27-AUG-2022 VIJI RAJ 58/2472 CGS QTRS SECTOR VIII ANTOP HILL BOMBAY INDIA MAHARASHTRA MUMBAI 400037 150.00 27-AUG-2022 C-10 SANGLI VAIBHAV CHS NATWAR NAGAR RD 15 JYOTSNA K MANE JOGESHWARI E INDIA MAHARASHTRA MUMBAI 400060 150.00 27-AUG-2022 A 15 GOPURAM HSG SOC SOMANI GRAM RAM MANDIR ARUNA SINGH ROAD GOREGAON W BOMBAY INDIA MAHARASHTRA MUMBAI 400104 150.00 27-AUG-2022 AT & POST PANVEL PATEL MOHALLA LOHAR ALI DIST PRAKASH D MORE RAIGAD INDIA MAHARASHTRA PANVEL 410206 150.00 27-AUG-2022 A/17 SEVADHAM 4TH FLOOR SHRIPAL NGR RAJAJI CROSS MAHESH BAUA RD NO 4 DOMBIVALI E INDIA MAHARASHTRA DOMBIVALI 421201 150.00 27-AUG-2022 C/O SHRI KAMAL TATWADE 593 PANCHAM KI FAIL HEMANT BERWA INDORE M P INDIA MADHYA PRADESH INDORE 452003 -

Sr. No. Branch ID Branch Name City Branch Address Branch Timing Weekly Off Micrcode Ifsccode
Sr. No. Branch ID Branch Name City Branch Address Branch Timing Weekly Off MICRCode IFSCCode Adilabad, Andhra Pradesh,H.No. 4-3-60/10, 11,Opp. Bus Stand, N H No. 7,Adilabad 1 727 Adilabad Adilabad 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 504211002 UTIB0000727 504001, Andhra Pradesh H No: 1-1-3/4. Ground Floor, Mahalakshmi Temple Road, Armoor, Dist.Nizamabad, 2 2602 Armoor Armur 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 503211203 UTIB0002602 Telangana, Pin 503224 3 3966 Bachupally Bachupally Satyam towers, G-6, D.No : 3-3/16/G6 Bachupally (Mandal), Hyderabad - 500090 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 500211081 UTIB0003966 Ground floor & first Floor : House No: 10-1-65 Krishna Mandir Road, Bellampalli - 4 3965 Bellampally Bellampalli 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 504211099 UTIB0003965 504251 5 3574 Bhongir Bhongir No:1-5-330, Station road, opp : sai baba temple Bhongir – 508116 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 508211116 UTIB0003574 Vijay Manohar Mansion, Door No. 5-105/6/1, Ground Floor, Plot No.14 &15, Survey 6 1114 Bibinagar Bibinagar No.596, Hyderabad-Warangal Main Road, Bibinagar Village & Mandal, Dist. Nalgonda, 9:30 a.m. to 3:30 p.m. 2nd & 4th Saturday and Sunday 500211025 UTIB0001114 Andhra Pradesh 508126 No.1-19/13, Veerabhadra Complex, Opp. Market Yard, Hyderabad Main Road, Chevella, 7 1266 Chevella Chevella 9:30 a.m. -

Di, Hyderabad Details of Units Reimbursed Under
MSME - DI, HYDERABAD DETAILS OF UNITS REIMBURSED UNDER ISO-9000 FOR THE YEAR 2008-09 SL. Name of the Unit Address Amount Remarks NO. Reimbursed with date 1. M/s. Sri Sai Lakshmi 110, Kesavayanigunta, 52,500/- Die Castings Ltd. Tirupathi –517501. Dt.26.6.08 2. M/s.Challa Cables Pvt # 5-246/9/2, HPC Road, 31,425/- Ltd Moosapet, Dt.26.9.08 Hyderabad-1. 3. M/s. Fine Forge Ltd., Plot No.24A/1, IDA,Phase-I, 54,000/- Patancheru-502319 Dt.3.11.08 4. M/s.Lyophilization 26 & 27, Aleap Indl.Esate, Opp. 51,750/- Systems India P.L. JNTU Rd., Kukatpally, Hyd-072 Dt.10.7.08 5. M/s.Chensun 138/199, MTH Road, Padi, 46,200/- Industries Chennai Dt.31.7.08 6. M/s.Visra 27,TIE,Balanagar, Hyd-37 50,940/- Mechatronics, Dt.16.7.08 7. M/s S.R.Drugs & Plot No.24-B/1, IDA, Ph-I, 52,500/- Intermediates Pvt. Ltd. Dist.Medak, Patancheru-502319 Dt.30.3.09 8. M/s.Comnet Telys 1-1-298/2,Plot.No.28, Arul 74,250/- Pvt.Ltd Colony,Kapra Keesara (M), Dt.1.9.08 Ranga Reddy Dist, Hyderabad-62. 9. M/s.Ultrafil Air Plot.No.17, IDA, Nacharam, Upal 61,500/- Systems, (M), Dt.1.9.08 R.R.Dist, Hyderabad-76. 10. M/s.Hobby Tools & 11-175/11B, Fathenagar, 52,883/- Components, Hyderabad-500018. Dt.16.7.08 11. M/s.Teena Labs Pvt 105 & 1076, Sree Rama Towers, 71,250/- Ltd, Kukatpally, Hyderabad.72. -

Government of Andhra Pradesh
GOVERNMENT OF ANDHRA PRADESH A B S T R A C T Municipal Administration and Urban Development Department – Revised Common Building Rules, 2006 – Orders – Issued MUNICIPAL ADMINISTRATION AND URBAN DEVELOPMENT (M) DEPARTMENT G.O.Ms.No. 86, Dated the 3rd March, 2006. Read the following : 1. G.O.Ms.No.423 M.A. & U.D. Department, dated 31.07.1998 2. Government Memo No.19048/M1/2004-4 M.A., dated15.12.2005. 3. A.P.Extra Ordinary Gazette No.4, dated 22.01.2005. -- o0o -- O R D E R: In the reference 1st read above, Government have issued Comprehensive Building Rules which are applicable to Municipal Corporations, Municipalities and areas covered by Urban Development authorities. Since then these Building Rules have governed building activities in urban areas. 2. It has been brought to the notice of the Government that the above building stipulations are cumbersome with too many parameters for regulating and controlling developments and building activities and there is a need for simplifying the building stipulations by stipulating minimal parameters. Further due to changes in building technologies, massive and rapid urbanization, escalating land prices, and certain shortcomings experienced relating to the existing building stipulations Government have decided to review the building stipulations and come out with comprehensive building rules thereby, making the building stipulations clear, easy to comprehend, user-friendly, promoting various types of development and building activities, besides giving design freedom and choice with optimum usage of land on one hand, and reducing the trend of violations and unauthorized constructions on the other, without compromising on the community good. -

Inequity in Water Supply and Impact on the Poor: the Case of Hyderabad
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Loughborough University Institutional Repository RAMACHANDRAIAH 30th WEDC International Conference, Vientiane, Lao PDR, 2004 PEOPLE-CENTRED APPROACHES TO WATER AND ENVIRONMENTAL SANITATION Inequity in water supply and impact on the poor: The case of Hyderabad C. Ramachandraiah, India There are significant variations in the access of households to tap water between the core city and the surrounding urban areas in Hyderabad. In the surrounding areas, a substantial proportion of the households have their source of water out- side their premises. Rather than the lack of water, it is the iniquitous distribution and denial of clean drinking water to the urban poor that led to the outbreak of water-contaminated diseases on a large scale in 2003 in Hyderabad city. The two main reservoirs that are the principal sources of drinking water to the old city have been neglected over the years leading to their drying up, for the first time, in 2003. Despite untold miseries suffered by the poor, the State continues to be luke- warm to their plight, which is highlighted in this paper. Such neglect by the State is probably due to lack of mobilization by the poor to form an effective pressure group at grassroots level to lobby for basic amenities. Introduction to the MCH area but, in recent years only, it has started In recent years, the Hyderabad Urban Agglomeration (HUA) supplying water in the surrounding areas. In terms of loca- has emerged as an important software centre in India. -

Sri Sai Nandanam
https://www.propertywala.com/sri-sai-nandanam-hyderabad Sri Sai Nandanam - Manikonda, Hyderabad Magnificent Homes Sri Sai Nandanam is a magnificent residential project offering a set of 2 & 3 BHK luxurious apartments of aesthetic design and quality construction surrounded by reserved forest land. Project ID : J440271190 Builder: Sri Sai Properties: Apartments / Flats, Residential Plots / Lands Location: Sri Sai Nandanam, Manikonda, Hyderabad (Telangana) Completion Date: Apr, 2011 Status: Started Description Sri Sai Nandanam is a magnificent residential project offering a set of 2 & 3 BHK luxurious apartments of aesthetic design and quality construction surrounded by reserved forest land. It's a pollution free zone coupled with serenity for a peaceful rejuvenation.It is Ongoing Project of its Group. Location Advantages: Adjacent to Lanco Hills 0.3 Km away to 100' road connecting to Outer Ring Road 4 Km away from Hi-Tech City, Nift, Shilparamam, ISB, etc 1.5 Km away to Proposed 600 ft. Outer Ring Road Close to Software Companies like Microsoft, Wipro, Infosys etc 2 Kms from Film Nagar Amenities: Children's Play Area. Games Room. Car Parking Space. Landscape Garden. 24 hr. Security. Power Backup. Well Developed Roof. Features Luxury Features Security Features Power Back-up RO System Water Softner Security Guards Electronic Security Intercom Facility Fire Alarm Land Features Other features Feng Shui / Vaastu Compliant Society Name: Sri Sai Nandanam Club / Community Center Adjacent to Main Road Transaction: New Property Possession: Apr 2011 -

A Detailed Property Analysis Report of Sri Sai Harihara Siri
PROPINSIGHT A Detailed Property Analysis Report 40,000+ 10,000+ 1,200+ Projects Builders Localities Report Created On - 7 Oct, 2015 Price Insight This section aims to show the detailed price of a project and split it into its various components including hidden ones. Various price trends are also shown in this section. Project Insight This section compares your project with similar projects in the locality on construction parameters like livability rating, safety rating, launch date, etc. What is Builder Insight PROPINSIGHT? This section delves into the details about the builder and tries to give the user a perspective about the history of the builder as well as his current endeavours. Locality Info This section aims to showcase various amenities viz. pre-schools, schools, parks, restaurants, hospitals and shopping complexes near a project. Sri Sai Harihara Siri Residency Uppal Kalan, Hyderabad 71.8 Lacs onwards Livability Score 6.7/ 10 Project Size Configurations Possession Starts 1 Towers 3 Bedroom Apartment Sep `15 Pricing Comparison Comparison of detailed prices with various other similar projects Pricing Trends Price appreciation and trends for the project as well as the locality What is PRICE INSIGHT? Price versus Time to completion An understanding of how the current project’s prices are performing vis-a-vis other projects in the same locality Demand Comparison An understanding of how the strong/weak is the demand of current project and the current locality vis-a-vis others Price Trend Of Sri Sai Harihara Siri Residency -

Sl. No. Name of the Division Jurisdiction of the Division Name Of
Annexure - IV to Trade Notice No. 01/2014 dated 01.10.2014 HYDERABAD- IV COMMISSIONERATE : HEADED BY COMMISSIONER JURISDICTION OF HYDERABAD - IV COMMISSIONERATE : In the District of Ranga Reddy of the State of Telangana but excluding the areas falling under the said Ranga Reddy District under the jurisdiction of Hyderabad - I, Hyderabad - II and Hyderabad - III Commissionerates. Sl. Name of the Division Jurisdiction of the Division Name of the Range Jurisdiction of the Range No. 1 MEDCHAL DIVISION All villages of Qutubullapur Mandal Kompally Range Villages of Kompally, Pet Basheerabad, Jeedimetla (Excluding IDA of (Excluding Nizampet and Jeedimetla consisting of Jeedimetla - I to V Ranges of Jeedimetla Division), Bachupally villages, IDA of Qutubullapur (excluding Gandhinagar IDA of Qutubullapur village), Jeedimetla consisting of Jeedimetla - Dulapalli, Bahadurpalli and Suraram of Qutubullapur Mandal, and M/s. I to V Ranges of Jeedimetla Division Granules India Limited of Gundlapochampally Village. and Gandhinagar I.D.A. of Qutubullapur village). All villages of Medchal and Shameerpet Mandal. Gundlapochampally All other villages of Qutubullapur Mandal (excluding Nizampet and Range Bachupalli Villages), Gundlapochampally and Kandlakoi villages of Medchal Mandal, except M/s. Granules India Limited. Medchal Range All villages of Medchal Mandal but excluding Rajabollaram, Ghanpur, Gundla pochampally, Muraharipally and Kandlakoi villages. Shameerpet Range Villages of Ghanpur, Rajabollaram and Muraharipally of Medchal Mandal and all villages of Shameerpet Mandal. Subhash Nagar Range The right side of M/s. KLJ Plastics Road in Phase-I of IDA Jeedimetla and Phase-II of IDA Jeedimetla. Annexure - IV to Trade Notice No. 01/2014 dated 01.10.2014 2 KUKATPALLY DIVISION Hydernagar, Shamshiguda, Kukatpally - I Range I.