Please Pass the Peanut Butter: Nutrition Strategies to Prevent and Manage Food Allergies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Food Allergy Outline
Allergy Evaluation-What it all Means & Role of Allergist Sai R. Nimmagadda, M.D.. Associated Allergists and Asthma Specialists Ltd. Clinical Assistant Professor Of Pediatrics Northwestern University Chicago, Illinois Objectives of Presentation • Discuss the different options for allergy evaluation. – Skin tests – Immunocap Testing • Understand the results of Allergy testing in various allergic diseases. • Briefly Understand what an Allergist Does Common Allergic Diseases Seen in the Primary Care Office • Atopic Dermatitis/Eczema • Food Allergy • Allergic Rhinitis • Allergic Asthma • Allergic GI Diseases Factors that Influence Allergies Development and Expression Host Factors Environmental Factors . Genetic Indoor allergens - Atopy Outdoor allergens - Airway hyper Occupational sensitizers responsiveness Tobacco smoke . Gender Air Pollution . Obesity Respiratory Infections Diet © Global Initiative for Asthma Why Perform Allergy Testing? – Confirm Allergens and answer specific questions. • Am I allergic to my dog? • Do I have a milk allergy? • Have I outgrown my allergy? • Do I need medications? • Am I penicillin allergic? • Do I have a bee sting allergy Tests Performed in the Diagnostic Allergy Laboratory • Allergen-specific IgE (over 200 allergen extracts) – Pollen (weeds, grasses, trees), – Epidermal, dust mites, molds, – Foods, – Venoms, – Drugs, – Occupational allergens (e.g., natural rubber latex) • Total Serum IgE (anti-IgE; ABPA) • Multi-allergen screen for IgE antibody Diagnostic Allergy Testing Serological Confirmation of Sensitization History of RAST Testing • RAST (radioallergosorbent test) invented and marketed in 1974 • The suspected allergen is bound to an insoluble material and the patient's serum is added • If the serum contains antibodies to the allergen, those antibodies will bind to the allergen • Radiolabeled anti-human IgE antibody is added where it binds to those IgE antibodies already bound to the insoluble material • The unbound anti-human IgE antibodies are washed away. -

Egg Allergy: the Facts
Egg Allergy: The Facts Egg is a common cause of allergic reactions in infants and young children. It often begins in the child’s first year of life and in some cases lasts into the teenage years – or even into adulthood for a few people. Children who develop allergy to foods such as egg often have other allergic conditions. Eczema and food allergy often occur in early infancy and later on there may be hay-fever, asthma or both. This Factsheet aims to answer some of the questions which you and your family may have about living with egg allergy. Our aim is to provide information that will help you to understand and minimise risks. Even severe cases can be well managed with the right guidance. Many cases of egg allergy are mild, but more severe symptoms are a possibility for some people. If you believe you or your child is allergic to egg, the most important message is to visit your GP and ask for allergy tests and expert advice on management. Throughout this Factsheet you will see brief medical references given in brackets. If you wish to see the full references, please email us at [email protected]. Symptoms triggered by egg The symptoms of a food allergy, including egg allergy, may occur within seconds or minutes of contact with the culprit food. On occasions there may be a delay of more than an hour. Mild symptoms include nettle rash (otherwise known as hives or urticaria) or a tingling or itchy feeling in the mouth. More serious symptoms are uncommon but remain a possibility for some people, including children. -
Phase I Open-Label Study of Omalizumab (Xolair) in Peanut-Allergic Patients
Kari C. Nadeau, MD, PhD Division of Allergy , Immunology, and Rheumatology at Stanford Describe the pathophysiology, initial evaluation & management of patients with food allergy including gastrointestinal food allergy, oral allergy syndrome and type I food allergy Identify recent advances in the field of food allergy and have some familiarity with published guidelines for managing food allergy Outline current and emerging treatment modalities for food allergic patients Nothing to disclose ID: 9.5 y.o. male with a history of severe food allergies, eczema, and asthma CC: Presents to PICU with hypoxic brain injury due to anaphylaxis from cow’s milk ingestion Transferred to PICU from outside hospital after multiple failed resuscitations over a 3 hr period On the evening of 8-11-04, patient accidentally drank from his sister’s cup of cow’s milk on the way to bed. He immediately developed emesis and became SOB; parents gave Epipen jr. to his thigh and called 911 Paramedics arrived in 10-15 minutes On the scene, intubation was attempted but difficult Duration of code=1 hr. CT scan showed hypoxic injury and right uncal herniation. In 2001, he presented to LPCH AAI clinic and had severe eczema and asthma. RAST tests were performed at 2001 and showed IgE > 2000, Milk> 100, Peanut>100, Egg 40.3, Soy 17.9, Wheat 20.2, Corn 26.3, Oat 12.3. No known allergies to beef. He had had one prior visit to the ER for milk ingestion in 2001. He presented with hyperventilation and emesis. He was given benadryl and his symptoms improved. -

Soy Free Diet Avoiding Soy
SOY FREE DIET AVOIDING SOY An allergy to soy is common in babies and young children, studies show that often children outgrow a soy allergy by age 3 years and the majority by age 10. Soybeans are a member of the legume family; examples of other legumes include beans, peas, lentils and peanut. It is important to remember that children with a soy allergy are not necessarily allergic to other legumes, request more clarification from your allergist if you are concerned. Children with a soy allergy may have nausea, vomiting, abdominal pain, diarrhea, bloody stool, difficulty breathing, and or a skin reaction after eating or drinking soy products. These symptoms can be avoided by following a soy free diet. What foods are not allowed on a soy free diet? Soy beans and edamame Soy products, including tofu, miso, natto, soy sauce (including sho yu, tamari), soy milk/creamer/ice cream/yogurt, soy nuts and soy protein, tempeh, textured vegetable protein (TVP) Caution with processed foods - soy is widely used manufactured food products – remember to carefully read labels. o Soy products and derivatives can be found in many foods, including baked goods, canned tuna and meat, cereals, cookies, crackers, high-protein energy bars, drinks and snacks, infant formulas, low- fat peanut butter, processed meats, sauces, chips, canned broths and soups, condiments and salad dressings (Bragg’s Liquid Aminos) USE EXTRA CAUTION WITH ASIAN CUISINE: Asian cuisine are considered high-risk for people with soy allergy due to the common use of soy as an ingredient and the possibility of cross-contamination, even if a soy-free item is ordered. -

Oral Immunotherapy for Peanut Allergy: an Evidence-Based Medicine Assessment
Editorials 2. Paraskevas KI, Bessias N, Perdikides TP, Mikhailidis DP. Statins and venous infarctions induce differential lesional interleukin-16 (IL-16) expression confined to thromboembolism: A novel effect of statins? Current Medical Research and infiltrating granulocytes, CD8+ T-lymphocytes and activated Opinion 2009; 25(7):1807-09. http://dx.doi.org/10.1185/03007990903052591 microglia/macrophages. Journal of Neuroimmunology 2001;114:232-24. 3. Waters DD. Exploring new indications for statins beyond atherosclerosis: Successes http://dx.doi.org/10.1016/S0165-5728(00)00433-1 and setbacks. J Cardiol 2010;55(2):155-62. 10. Heart Stabile E, Kinnaird T, la Sala A, et al. CD8+ T Lymphocytes Regulate the http://dx.doi.org/10.1016/j.jjcc.2009.12.003 Arteriogenic Response to Ischemia by Infiltrating the Site of Collateral Vessel 4. Muscal E, Brey RL Antiphospholipid syndrome and the brain in pediatric and adult Development and Recruiting CD4 Mononuclear Cells Through the Expression of patients. Lupus 2010;19(4):406-11. http://dx.doi.org/10.1177/0961203309360808 Interleukin-16. Circulation 2006,113:118-24. 5. Pedersen TR. Pleiotropic effects of statins: evidence against benefits beyond LDL- http://dx.doi.org/10.1161/CIRCULATIONAHA.105.576702 cholesterol lowering. Am J Cardiovasc Drugs 2010;10(Suppl 10). 11. National Research Council. "10 Tobacco Smoke and Toxicology." Clearing the 6. Morales-Villegas EC, Di Sciascio G, Briguori C. Statins: Cardiovascular Risk Smoke: Assessing the Science Base for Tobacco Harm Reduction. Washington, DC: Reduction in Percutaneous Coronary Intervention—Basic and Clinical Evidence of The National Academies Press, 2001.) Hyperacute Use of Statins. -
Soyallergy.Pdf
Prognosis and Management Soy allergies are more common in young children and are usually outgrown early in life. The chance of outgrowing soy allergy often depends on whether it is IgE-mediated or non-IgE mediated. Non-IgE mediated soy allergies are usually outgrown in early childhood. IgE-mediated soy allergies can be outgrown, but in some cases may persist throughout life. IgE levels to soy will be monitored throughout your child’s care. Changes in IgE levels can predict the likelihood of your child FOOD ALLERGY PROGRAM What about outgrowing his/her The Food Allergy Program at Children’s National Medical soy oil and soy allergy. If the levels are Center provides comprehensive services in the evaluation and lecithin? dropping and they management of a wide variety of food allergies, including reach a certain level, IgE-mediated food allergy, gastrointestinal food allergy, and After reading a few a food challenge eosinophilic gastrointestinal disorders. food labels, you may become may be done in overwhelmed because it seems almost a controlled Food Allergy Program everything contains soy! However, it’s medical Children’s National Medical Center helpful to know that studies show both setting to 111 Michigan Avenue, NW soy oil and soy lecithin can be safely eaten determine Washington, DC 20010 by children with soy allergy. This is whether or Phone: 202-476-3016 likely because the soy protein in these not your child Fax: 202-476-2280 foods is so processed it cannot ALLERGY has outgrown the be recognized by the immune allergy. RESOURCES system. However, be sure For more detailed information about food allergies, visit: to discuss this with your • The Food Allergy and Anaphylaxis Network SOY allergist! (www.foodallergy.org) about • The Food Allergy Initiative (www.faiusa.org) www.childrensnational.org Supported by a grant from the Children’s National Medical Center Board of Visitors ALL Soy Allergy Overview Different kinds of soy allergy Management of soy allergy Soybeans are legumes. -

Soy Allergy Diet Avoid All Sources of Soy Protein
FAIRFAX 3903-A Fair Ridge Drive • Fairfax, VA 22033 • 703 648 0030 • fax: 703 648 9028 WOODBRIDGE 1952 Opitz Blvd • Woodbridge, VA 22191 • 703 494 7849 • fax: 703 494 8730 wheezefree.com SOY ALLERGY DIET AVOID ALL SOURCES OF SOY PROTEIN Avoiding products made with soy is difficult. Soybeans have become a major part of processed food products in our country. Soybeans and soybean products are found in baked goods, canned tuna, cereals, crackers, infant formulas, sauces, and soups. In the processing of most soybean oils, the protein portion is removed. Studies have shown that most people with a soy allergy my safely eat soy lecithin and soybean oil. READ FOOD LABELS Knowing how to read a food label will help you avoid problems caused by soybean protein in foods. Terms that mean the product does contain soybean protein: edamame soy bean (granules, curd) hydrolyzed soy protein soy protein miso Tamari shoyu sauce Tempeh soy (albumin, fiber, flour, grits, nuts, milk, sprouts) textured vegetable soy protein (concentrate, isolate) protein (TVP) soy sauce tofu soya Terms that may mean the product contains soybean protein: flavoring (natural and artificial) vegetable gum vegetable broth vegetable starch PROVIDE MISSING NUTRIENTS Soybeans alone aren’t a major food in the diet, but because they are in so many products, eliminating all those foods can result in a vitamin deficiency. As a precaution, give your child a daily vitamin pill. Work with a dietitian to be sure your child’s nutritional needs are met.. -
Early Infant Feeding Guidelines Faqs
v v Early Infant Feeding Guidelines FAQs The new Addendum Guidelines for the Prevention of Peanut Allergy in the U.S. were released in January 2017. This report from the National Institute of Allergy and Infectious Diseases (NIAID) represents a dramatic shift from previous advice to parents and caregivers regarding the introduction of peanut in a child’s diet. The Canadian Society of Allergy and Clinical Immunology (CSACI) and Food Allergy Canada have compiled this list of FAQs from the most common questions parents asked about these guidelines. These questions are answered by Canadian Pediatric Allergists Dr. Elissa M. Abrams and Dr. Kyla J. Hildebrand. We hope you find these FAQs helpful and informative. As always, we advise parents to speak with their physician if they have any concerns. 2 v v About the research and the recommendations to introduce peanut early to infants Questions by parents Answers by Canadian allergists 1. What specifically do the The main message from these guidelines is that for most infants, peanut can be new NIAID (National introduced safely at home. In high risk infants (those infants with severe eczema, Institute of Allergy and egg allergy or both), the guidelines recommend that peanut be introduced at 4-6 Infectious Diseases) months of age after evaluation by a physician, as it is recommended to offer Addendum Guidelines for allergy testing for peanut in this specific group of infants prior to eating peanut. the Prevention of Peanut Any child with a positive allergy test to peanut would also require further Allergy in the United States evaluation prior to eating peanut. -

What You Need to Know About the New Guidelines for the Diagnosis and Management of Food Allergy in the U.S
Allergy guidelines insert_Layout 1 9/26/11 1:36 PM Page 1 What you need to know about the new guidelines for the diagnosis and management of food allergy in the U.S. V OLUME 126, N O . 6 D ECEMBER 2010 • Tests for food-specific IgE are recom- Overview www.jacionline.org • The Guidelines, sponsored by the NIH Supplement to mended to assist in diagnosis, but should (NIAID), are based upon expert opinion THE JOURNAL OF not be relied upon as a sole means to di- Allergy ANDClinical and a comprehensive literature review. Immunology agnose food allergy. The medical history/ AAP had input on the document.1,2 exam are recommended to aid in diag- nosis. A medically monitored feeding Guidelines for the Diagnosis and Management Definitions of Food Allergy in the United States: Report of the (food challenge) is considered the most NIAID-Sponsored Expert Panel • Food allergy was defined as an adverse definitive test for food allergy. health effect arising from a specific im- • Food-specific IgE testing has numerous mune response. limitations; positive tests are not intrin- • Food allergies result in IgE-mediated sically diagnostic and reactions some- immediate reactions (e.g., anaphylaxis) OFFICIAL JOURNAL OF times occur with negative tests. These and several chronic diseases (e.g., ente- Supported by the Food Allergy Initiative issues are also reviewed in an AAP Clini - rocolitis syndromes, eosinophilic esopha - cal Report.3 Testing “food panels” with- gitis, etc), in which IgE may not play an important role. out considering history is often mis - leading. Tests selected to evaluate food allergy should be Epidemiology and Natural History based on the patient’s medical history and not comprise • Food allergy is more common in children than adults, large general panels of food allergens. -

Soy Allergy Avoidance List Hidden Names for Soy Compiled by Debra A
Soy Allergy Avoidance List Hidden Names for Soy Compiled by Debra A. Indorato RD, LDN, member of KFA’s Medical Advisory Team Foods covered by the FDA labeling laws that contain soy must be labeled in plain English to declare that it “contains soy.” However, there are many foods and products that are not covered by FDA allergen labeling laws, so it is still important to know how to read a label for soy ingredients. Products exempt from plain English labeling rules: foods that are not regulated by the FDA (tinyurl.com/KFA-FALCPA), cosmetics and personal care products, prescription and over-the-counter medications or supplements, pet food, toys and crafts. contain soy The following ingredients found on a label indicate the presence of soy protein. All labels should be read carefully before consuming a product, even if it has been used safely in the past. Bean curd Soya may contain soy Edamame (soybeans in pods) Soya Flour Artificial flavoring Hydrolyzed soy protein Soybeans Asian foods (e.g. Japanese, Kinnoko flour Soybean granules Chinese, Thai, etc.) Kyodofu (freeze dried tofu) Soybean curd Hydrolyzed plant protein Miso Soybean flour Hydrolyzed vegetable protein (HVP) Natto Soy lecithin* Natural flavoring Okara (soy pulp) Soybean paste Vegetable broth Shoyu sauce Supro Vegetable gum Soy albumin Tamari Vegetable starch Soy bran Tempeh Soy concentrate Teriyaki sauce should be safe Soy oil (except cold pressed, expeller Soy fiber Textured soy flour (TSF) pressed or extruded soybean oil) Soy flour Textured soy protein (TSP) Soy formula Textured vegetable protein (TVP) Vegetable oil derived from soy Soy grits Tofu These soy derivatives should be safe Soy milk Yakidofu for most soy-allergic individuals. -
Soy Allergy(1).Pdf
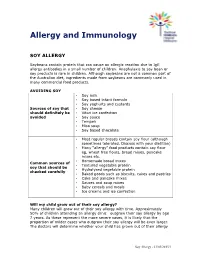
Allergy and Immunology SOY ALLERGY Soybeans contain protein that can cause an allergic reaction due to IgE allergy antibodies in a small number of children. Anaphylaxis to soy bean or soy products is rare in children. Although soybeans are not a common part of the Australian diet, ingredients made from soybeans are commonly used in many commercial food products. AVOIDING SOY • Soy milk • Soy based infant formula • Soy yoghurts and custards Sources of soy that • Soy cheese should definitely be • Vitari ice confection avoided • Soy sauce • Tempeh • Miso soup • Soy based chocolate • Most regular breads contain soy flour (although sometimes tolerated. Discuss with your dietitian) • Many “allergy” food products contain soy flour eg, wheat free flours, bread mixes, pancake mixes etc. • Homemade bread mixes Common sources of • Textured vegetable protein soy that should be • Hydrolysed vegetable protein checked carefully • Baked goods such as biscuits, cakes and pastries • Cake and pancake mixes • Sauces and soup mixes • Baby cereals and meals • Ice creams and ice confection Will my child grow out of their soy allergy? Many children will grow out of their soy allergy with time. Approximately 50% of children attending an allergy clinic outgrow their soy allergy by age 7 years. As these represent the more severe cases, it is likely that the proportion of milder cases who outgrow their soy allergy will be even larger. The doctors will determine whether your child has grown out of their allergy Soy Allergy - 21/05/2013/1 by a combination of skin testing and food challenge with soy. Skin tests may be repeated periodically (often on a yearly basis) to monitor your child’s soy allergy. -

Peanut Allergy and Tree Nut Allergy – the Facts
Peanut Allergy and Tree Nut Allergy – The Facts Peanut allergy and tree nut allergy can sometimes result in severe allergic reactions and understandably this can cause intense anxiety among those affected and their families. This Factsheet aims to answer some of the questions which you and your family might have about living with peanut allergy or tree nut allergy. Our aim is to help you to minimise risks and learn how to treat an allergic reaction should it occur. The peanut is a legume, related botanically to foods such as peas, beans and lentils. Tree nuts are in a different botanical category and include almonds, hazelnuts, walnuts, cashew nuts, pecans, Brazil nuts, pistachios and macadamia nuts. A key message for people with peanut or tree nut allergy is take your allergy seriously. You should visit your GP and ask to be referred to an NHS allergy clinic for a proper assessment and high-quality advice. Throughout the text you will see brief medical references given in brackets. If you would like the full references, please call the Anaphylaxis Campaign helpline on 01252 542029. How common are peanut allergy and tree nut allergy? Research has shown that peanut allergy among children increased significantly during the 1990s. In 2002 a medical team on the Isle of Wight found that around one in 70 children across the UK was allergic to peanuts, compared with one in 200 a decade before (Grundy et al, 2002). A more recent follow-up study by the same group suggests a slight fall in cases (Venter et al 2010).