Gujarat 3Rd Crm Report.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

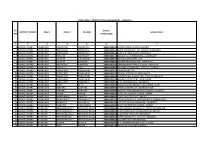
Rainfall in Mm) Sr
State Emergency Operation Centre,Revenue Department, Gandhinagar Rainfall Report 31/10/2018 (Rainfall in mm) Sr. District/ Avg Rain Rains till Rain During Total % Against Avg Rain Rains till Rain During Total % Against No Sr.No. District/ Taluka Taluka (1988-2017) Yesterday last 24 Hrs. Rainfall Avg Rain (1988-2017) Yesterday last 24 Hrs. Rainfall Avg Rain . 1 2 3 4 5 6 7 1 2 3 4 5 6 7 KUTCH NORTH GUJARAT 1 Kutch 4 Mahesana 1 Abdasa 390 53 0 53 13.61 1 Becharaji 659 294 0 294 44.64 2 Anjar 434 231 0 231 53.28 2 Jotana 753 139 0 139 18.45 3 Bhachau 441 103 0 103 23.36 3 Kadi 814 258 0 258 31.71 4 Bhuj 376 83 0 83 22.08 4 Kheralu 727 207 0 207 28.47 5 Gandhidham 403 264 0 264 65.54 5 Mahesana 760 288 0 288 37.90 6 Lakhpat 349 12 0 12 3.44 6 Satlasana 769 504 0 504 65.55 7 Mandvi(K) 434 118 0 118 27.22 7 Unjha 743 239 0 239 32.18 8 Mundra 477 145 0 145 30.40 8 Vadnagar 694 307 0 307 44.21 9 Nakhatrana 406 70 0 70 17.22 9 Vijapur 826 370 0 370 44.80 10 Rapar 460 26 0 26 5.65 10 Visnagar 689 195 0 195 28.32 Dist. Avg. 417 111 0 111 26.51 Dist. Avg. 743 280 0 280 37.70 KUTCH REGION 417 111 0 111 26.51 5 Sabarkantha 1 Himatanagar 838 902 0 902 107.60 NORTH GUJARAT 2 Idar 960 763 0 763 79.45 2 Patan 3 Khedbrahma 843 502 0 502 59.56 1 Chanasma 525 103 0 103 19.60 4 Posina 833 503 0 503 60.38 2 Harij 577 173 0 173 29.97 5 Prantij 832 415 0 415 49.86 3 Patan 685 164 0 164 23.93 6 Talod 804 418 0 418 51.97 4 Radhanpur 626 190 0 190 30.36 7 Vadali 877 556 0 556 63.38 5 Sami 537 168 0 168 31.26 8 Vijaynagar 835 673 0 673 80.58 6 Santalpur 478 154 0 154 32.22 Dist. -
Banaskantha INDEX
Banaskantha INDEX 1 Banaskantha: A Snapshot 2 Economy and Industry Profile 3 Industrial Locations / Infrastructure 4 Support Infrastructure 5 Social Infrastructure 6 Tourism 7 Investment Opportunities 8 Annexure 2 1 Banaskantha: A Snapshot 3 Introduction: Banaskantha Map 1: District Map of Banaskantha with § Banaskantha is the third largest district of Gujarat and is Talukas located in North eastern region of the State § The region is presumably named after the West Banas River and shares its border with the neighbouring State of Rajasthan § There are 11 talukas in the district with Palanpur (District Headquarter), Deesa, Dantaand Amirgarhbeing the important and developed talukas of the district § Banaskantha contributes significantly to Agricultural production of the State and ranks No. 1 in the production of potatoes in India § The district is also known for its diamond and ceramic industry § The proposed Palanpur-Mehsana Investment Region along Amirgadh the Delhi-Mumbai Industrial Corridor (DMIC) is expected to Dhanera drive the economic growth of the district Dantiwada Tharad § Focus Industry Sectors Vav Deesa Danta § Food Processing Deoder Palanpur Bhabhar Sikori Vadgam § Tourism § Mineral Based Industries (Ceramic Industry) Taluka § Tourist Places: Ambaji, Kumbharia, Balaram-Ambaji District Headquarter Sanctuary and JessoreSloth Bear Sanctuary 4 Fact File Longitude: 71.03O to 73.02O East Geographical Location Latitude: 23.33Oto 24.25O North 45 O Centigrade (Maximum) Temperature 5 O Centigrade (Minimum) Average Rainfall 1550 mm Rivers -
DRAFT DETAILED PROJECT REPORT Volume II (Environmental Management Plan)
Roads and Buildings Department Government of Gujarat Second Gujarat State Highway Project Radhanpur-Chanasma (SH-55) DRAFT DETAILED PROJECT REPORT Volume II (Environmental Management Plan) December, 2018 LEA Associates South Asia Pvt. Ltd., India Consultancy Services for Project Management of Roads & Buildings Department, Second Gujarat State Highway Project Government of Gujarat R o a ds in Gujarat TABLE OF CONTENTS 1 INTRODUCTION ........................................................................................................................4 1.1 CONTEXT FOR THE EMP ........................................................................................................... 4 1.2 PROJECT ROAD ......................................................................................................................... 4 2 CORRIDOR CHARACTERISTICS ....................................................................................................5 2.1 CORRIDOR PROFILE .................................................................................................................. 5 2.2 PROPOSED IMPROVEMENTS FOR MAINTENANCE ................................................................... 6 3 PROJECT CORRIDOR - BASELINE .................................................................................................7 3.1 ENVIRONMENTAL AND SOCIAL INVENTORY ............................................................................ 7 3.2 STAKEHOLDER CONSULTATIONS ............................................................................................. -

List of Kaushalya Vardhan Kendra with Attach ITI
List of Kaushalya Vardhan Kendra with attach ITI No. District Taluka Name of KVK Attached ITI 1 Ahmedabad Ahmedabad City Ghatlodiya (P.H) Kubernagar 2 Ahmedabad Ahmedabad City Vastrapur (P.H) Saraspur 3 Ahmedabad Bavala Bagodara Bavala 4 Ahmedabad Bavala Durgi Bavala 5 Ahmedabad Bavala Kavitha Bavala 6 Ahmedabad Bavala Shiyal Bavala 7 Ahmedabad Daskroi Bareja Saraspur 8 Ahmedabad Daskroi Bopal (Godhavi) Sarkhej 9 Ahmedabad Daskroi Kuha Maninagr 10 Ahmedabad Detroj DetrojRampura Rampura Detroj DetrojRampura 11 Ahmedabad Dhandhuka Rojka Dhandhuka 12 Ahmedabad Dholka Badarkha Dholka 13 Ahmedabad Dholka Koth Thaltej (Women) 14 Ahmedabad Mandal Trent Mandal 15 Ahmedabad Sanad Mankol Sanad 16 Ahmedabad Sanad Virochannagar Sanad 17 Ahmedabad Viramgam Shahpur Viramgam 18 Aravali Bayad Ambaliyara Bayad 19 Aravali Bayad Demai Bayad 20 Aravali Bhiloda Kishan gadh Bhiloda 21 Aravali Bhiloda Torada Bhiloda 22 Aravali Dhansura Akrund vadagam 23 Aravali Malpur Aniyor Malpur 24 Aravali Malpur Ubharan Malpur 25 Aravali Meghraj Panchal Meghraj 1 No. District Taluka Name of KVK Attached ITI 26 Aravali Modasa Limbhoi Modasa 27 Aravali Modasa Sardoi Modasa 28 Banaskantha Amirgadh Iqbalgadh Amirgadh 29 Banaskantha Amirgadh virampur Amirgadh 30 Banaskantha Bhabhar Kuvala Bhabhar 31 Banaskantha Bhabhar Mitha Bhabhar 32 Banaskantha Danta Danta Kumbhariya 33 Banaskantha Danta Hadad Kumbhariya 34 Banaskantha Danta Navavas Kumbhariya 35 Banaskantha Dantiwada Panthawada Dantiwada 36 Banaskantha Deesa Agthala Deesa 37 Banaskantha Deesa Bhadath Deesa 38 Banaskantha -

India Floods 2017
REDUCING RISK India Floods 2017 loods have been a recurrent human casualties in hundreds, Surendranagar, Ahmedabad, Morbi, F phenomenon in India that lead extensive damage to infrastructure Gandhinagar, Kutch, Mehsana and to huge losses to lives, properties, and also severely affected the Valsad are hit by the large-scale livelihood systems, infrastructure animals. The Inter-Ministerial flooding. Banaskantha and Patan are and public utilities. As a matter of Central Team visited Assam to take among the worst-hit districts in the fact, 12% of the total landmass of the stock of situation, and Prime state due to heavy rains and flooding country (40 million hectare) is flood Minister Mr. Modi himself visited of the Banas and Sipu rivers. prone1. Gujarat flood affected areas. It shows Dhanera block Banaskatha district seriousness at the apex level. was worst affected and was Furthermore, as on August 18, 2017, inaccessible therefore the damages 25 states2 in the country are The cumulative rainfall was are estimated to be higher in the susceptible to floods, the most recorded in excess, in June and July block as reported by IAG members5. vulnerable States are Assam, Bihar, 2017, in most States of India. In India, Uttar Pradesh, Gujarat, West Bengal, Central Water Commission is Nodal The floods have impacted lives and Madhya Pradesh, Odisha, Andhra Agency for flood forecasting. They livelihoods, including education and Pradesh, Maharashtra, Punjab and have at present 221 Flood public transportation by damaging Jammu & Kashmir. Similarly as Forecasting Stations4 spread across roads, highways, rail lines and many as 137 districts3 are vulnerable 24 States & UTs. -

India Floods 2017" and River Basin Or National Flood Plans Are in Colombo, Partnership for Faith and a First Step but Not Enough Any More
August 2017 southasiadisasters.net 1 INTRODUCTION ABOUT THIS ISSUE Floods as an Opportunity n 2017, South Asia was n 2017 South Asia was ravaged by to look ahead to even greater systemic Iravaged by devastating Iunprecedented flooding that affected challenges — poor connectivity, limited floods that caused close to 41 million people across India, role of private sector, and knowledge management — and start evolving widespread death and Bangladesh and Nepal. While the death and destruction unleashed by these suitable solutions for them till 2030. destruction. It has been floods is tragic, it also represents an estimated that these floods opportunity to learn the necessary Floods do not spare the hotspots of have led to 1,200 casualties lessons to set South Asia firmly onto a terrorism or conflict and as a result pose and affected 40 million safer and greener development trajectory. a threat to people and prosperity in people across India, Nepal recovery. Estimates suggest over 100 and Bangladesh. India is By highlighting the existing gaps in the districts in India alone suffer from such perhaps one of the most response, preparedness and relief a double threat. Almost each country flood prone countries in the activities undertaken by various state in South Asia has similar conflict and non-state actors the key problems affected areas. Thus, floods impact local world. The 2017 floods have have been identified. This present issue security, governance, and human rights raised some very serious and of Southasiadisasters.net aims to just that. protection. inconvenient questions about the country's Local flood studies that explore and Local faith based organisation can be preparedness to such floods. -

VG-2017 MSME - Approved Investment Intentions District : Banaskantha Sr.No
VG-2017 MSME - Approved Investment Intentions District : Banaskantha Sr.No. Name of Company Registered Office Address 1 A R Udhyog Plot No.233 & 234,Chandisar GIDC,Chandisar-Palanpur,Banaskantha 2 AARTI COLD STORAGE R.S.NO. 268P AT KOTADA ,DEODAR JETDA ROAD,,Kotda Deodar-385535,Deodar,Banaskantha 3 Acme Micronised Minerals Plot No.235-2,GIDC Chandisar,Chandisar-Palanpur,Banaskantha 4 Akhani Mahendrakumar Ratilal Plot No-18,GIDC Industrial Estate Deodar,Deodar-Deodar,Banaskantha 5 Akhanii Mahendrakumar Ratilal Plot No.124, GIDC Deodar,Banaskantha,-,Banaskantha 6 AKSHAR STONE HEBATPURA PATIYA, ABU HIGHWAY, PALANPUR,,Palanpur-385001,Palanpur,Banaskantha 7 ALFA MICRONCE NEAR B.K PETROL PUMP, HIGHWAY CROSS ROAD, SHERPURA, MAJADAR,,Sherpura (Majadar)-385210,Vadgam,Banaskantha 8 ALPESHKUMAR.A PANCHAL PALANPUR HIGHWAY, JAYANTINAGAR, DEESA,,Deesa-385535,Deesa,Banaskantha 9 Ambica Electricals Plot No.118, GIDC Deodar,,-,Banaskantha 10 Amrit Oil Industries Plot No.106,GIDC Chandisar,Chandisar-Palanpur,Banaskantha 11 Amrut Eingineering Plot No.174,GIDC Chandisar,Chandisar-Palanpur,Banaskantha 12 AMRUTBHAI PATEL 84, SANTOMINAGAR, OLD LAXMIPURA,,Palanpur-385001,Palanpur,Banaskantha 13 ANIL PANCHAL ANTIYA AREA, RAMCHOWK, GADH,,Gadh-385001,Palanpur,Banaskantha 14 ANILKUMAR VORA AT.RAIYA,,Raiya-385565,Deodar,Banaskantha 15 ANILKUMAR.N PARMAR AT.NAVADEESA,,Nesda Nava-385535,Deesa,Banaskantha 16 ANKITKUMAR JOSHI AT.PEDAGARA,,Pedagara-385001,Palanpur,Banaska ntha 17 APPLE GRANITE INDUSTRIES PLOT NO 645,SECTOR 8,Gandhinagar-38207,Gandhinagar,Gandhinagar 18 Arasuri Engineers Plot No.46,Chandisar GIDC,Chandisar-Palanpur,Banaskantha 19 ASAGARALI VAKALIYA HUSAINI AREA, NEAR NEW MASZID, KANODAR,,Kanodar-385001,Palanpur,Banaskantha 20 Ashapura Cleaning Plot No,Chandisar GIDC,Chandisar-Palanpur,Banaskantha 21 ASHISH PATEL NEAR JAIN DERASAR, JASLENI,,Jasleni-385001,Palanpur,Banaskantha 22 Ashokkumar S Dhariwal Plot No-190,GIDC Ind Estate Chandisar,Chandisar-Palanpur,Banaskantha Page 1 of 11 VG-2017 MSME - Approved Investment Intentions District : Banaskantha Sr.No. -

Palanpur Circle Office Sr
Palanpur Circle Office Sr. No. Name of Office Name of Officer Designation Office No. Contact No. E-mail 1 Palanpur Circle Office Shri L A Gadhavi Addl. Chief Engineer 2742255451 9925212210 [email protected] 2 Palanpur Circle Office (Tech) Shri K.L.Jani Executive Engineer 9909940117 [email protected] 3 Palanpur Circle Office (Tech) Shri S B Patel Deputy Engineer 9925212111 [email protected] 4 Palanpur Circle Office (Tech) Shri K R Joshi Deputy Engineer 9925212225 [email protected] 5 Palanpur Circle Office (RSO) Shri S.D. Chaudhary Deputy Engineer 9925212211 [email protected] 6 Palanpur Circle Office (I/C.) Shri M. G. Patel Deputy Engineer(I/C) 6357196545 [email protected] 7 Palanpur Circle Office (Tech) Shri A. B. Trivedi Junior Engineer 9879615732 [email protected] 8 Palanpur Circle Office (Tech) Shri P.P.Prajapati Junior Engineer 9925212118 [email protected] 9 Palanpur Circle Office (Tech) Ms D. J. Modh Junior Engineer 9925212113 [email protected] 10 Palanpur Circle Office (Tech) Shri Y.G. Khant Junior Engineer 7434852101 [email protected] 11 Palanpur Circle Office (I/C) Shri P. R. Raval Junior Engineer (I/C) 9925212928 [email protected] 12 Palanpur Circle Office (I/C) Shri G. S. Singh Junior Engineer (I/C) 7069029636 [email protected] 13 Palanpur Circle Office (RSO) Shri K C Kumar Junior Engineer 7434852102 [email protected] 14 Palanpur Circle Office (Civil) Shri K. M. Jadav Junior Engineer(Civil) 9925212109 [email protected] 15 Palanpur Circle Office (Civil) Shri N. R. Amin Junior Engineer(Civil) 7573972163 [email protected] 16 Palanpur Circle Office (Civil) Smt. -

Distance from Village • to Village Banaskantha District
®umtltllmttnf uf »omba!l jlublie lVutltll ~wartmttnf Distance from Village •to Village IN Banaskantha District .IIOMBAY 11163 BANASKANTHA DISTRICT. From To 0~ Abu Road Station Achnlg~rh · .•• :til Do. · Ambnji 14 Do. Amirgadh Railway Station. 11 Do. Delwara 20 Do. Kiwarli... Railway . Stationo. .. 6 Do. Ma dl O]t . .~ ..... ~ ••• 7 Do. • ~ 0 Maval Railway $tation• ... 6 Do. Mount Abu·, .. IT! Do. Palanpur • S5 Do.· RUBhikesh ... -~ ' Danta AmbaMata ... 16! Do. ...... Chitroda c . '18 Do. Gbodial.· .......• ... 14 Do. Go Ia ... 17 Do. • Hathidara ·.•.• 17 .,Hirad · ..•• Do. ·, .... 29 Do. Jitpur : . ...... ., ·u .• . Do. .; ... Kodram ... ~261 Do. ... ·.· '- Mahomodpur .. ,... 20 Do. ·. .. ~ .:1 -,l ••• Memanvas~ ·- ... ·l. ~- ..... ;. S! Do. .. _ ... Navava.s ~ .. .. 5f Do ... Pachada ... 19! Do. .... - ' Pepal · ... · 23 Do. , ... · Pilucha 25! Do. • t ••• _. ·". ~.. _Ranpur ... 22f Do. •... ·. , · · ...., .. Rupa l 22i ·Do. .. , .:·;'; Shri Jaswant Gadh • 6l Do. ••• ~-->:--' •• ~· Sudasana .... .... 15 Do. ', J; Vadgam .... 21 Do. · Vansal ••• r_ Do. ··: .... Vesa ·.- ~il Do. Vijlasana .·24 Deesa Railway Station Agthal~ · •. ......... 19 Do. ~······...,., Akhal ·, 3! Do. ... · Asarda .. ·7 '. .21 Do. Atroli L' i>o. Bhaker •. 10 Do. Bharat ...... S! Do. Bhilari • .'\ .... 12! Do.· Bhoyan ..... 17 Do. ... · Bhuta.di . -17 Do. .., Chadotai:''. .. , .12! Do. ... Chhatrala · • · 151 Do.. · ... _•. ... Chandaar Rly. Station 9 IIO·WBk ~ 13 2 Miles. Deesa.:aallway Station •. ·;,•;• Dalwara :·-~· ·: 13! Do~ · #;. ... Dama ... 8 Dw ...... .. -

Tender Docume Hand Operated Ch at Main Dairy Pl
Tender Document For Supply of 5000 Units of Hand Operated Chaff Cutters At Main Dairy Plant and Chilling Centers at Tharad,Radhanpur and Khimana Ref: BNS/PUR/HANDCHAFF CUTTER/2021 Page 1 of 22 Notice Inviting Tender Bid BANASKANTHA DISTRICT CO-OP. MILK PRODUCERS’ UNION LTD., BANAS DAIRY, PB NO: 20, PALANPUR: 385 001 Phone: (02742) 253881 to 253885 TENDER NOTICE Sealed Bids are invited for supply of 5000 Units Hand Operated Chaff Cutter from experienced and eligible bidders. Tender document containing specification of items, general terms and conditions and the eligibility criteria is available at our website: www.banasdairy.coop. Completed bid, in sealed envelope super-scribed with the ‘Tender for Hand Operated Chaff Cutter by due date 27.03.2021, can be submitted latest by 27.03.2021 up to 01.30 PM. All bids shall be opened on 03.00 PM. on 27.03.2021, in presence of all present bidders. Incharge Managing Director reserves the right to accept or reject any or all tenders without assigning any reason there of and there shall be no dispute on that decision. Incharge Managing Director Page 2 of 22 Index Table of Contents Notice Inviting Tender Bid ....................................................................................................................... 1 Index ....................................................................................................................................................... 3 Preface ................................................................................................................................................... -

E-Auction Sale Notice
SALE NOTICE FOR SALE OF IMMOVEABLE/MOVABLES PROPERTIES Mehsana Regional Office : Shriram Complex, 2nd Floor, Radhanpur Rd., Mehsana - 384002. [Under Rule 6(2) and 8(6) of Security Interest (Enforcement) Rules, 2002] Phone No. : 02762-254080, 251003, 7567883435, Fax : 02762- 250874, Email ID : [email protected] E-auction sale notice for sale of movable/immovable assets under the Securitisation and Reconstruction of Financial Assets and Enforcement of Security Interest Act, 2002 read with proviso to rule 6(2) and 8(6) of the Security Interest (Enforcement) Rules, 2002. Notice is hereby given to the public in general and in particular to the Borrower (s) Guarantor (s) that the below described movable/ immovable properties hypothecated/mortgaged/charged to the Bank of Baroda [Erstwhile Dena Bank amalgamated into Bank of Baroda with effect from 1st April 2019 in term of Gazette of India No. GSR No. 2E dated 2nd January 2019 issued by Ministry of Finance, Government of India] a body corporate constituted under the Banking Companies (Acquisition and Transfer of Undertaking) Act 1970 and having its Head office at Mandvi, Baroda, Gujarat State and one of the Branch mentioned as below as the secured creditor, the constructive / physical possession of which has been taken by the Authorised officer of Secured Creditor under section 13(4) of the Act, will be sold on “As is where is”, As is what is” and “Whatever there is” on 30.05.2019 for recovery of Rs. (as mentioned below) due to the Bank Of Baroda secured creditor from (Name of Borrower & Guarantor mentioned below). -
SR NO DISTRICT NAME Block Cluster VILLAGE School U-DISE
U-DISE CODE / SCHOOL CODE ( Banaskantha - Palanpur ) SR School DISTRICT_NAME Block Cluster VILLAGE School Name NO U-DISE CODE 12 3 4 5 6 7 1 BANAS KANTHA AMIRGADH AMIRGADH AMIRGADH 24020100108 SHREE SARSWATI VIDYAMANDIR 2 BANAS KANTHA AMIRGADH AMIRGADH AMIRGADH 24020100111 GOVT. HIGHER SEC. SCI. SCHOOL, AMIRGADH 3 BANAS KANTHA AMIRGADH AMIRGADH AMIRGADH 24020100112 SHRI R. R. VIDHYALAY, AMIRGADH 4 BANAS KANTHA AMIRGADH KIDOTAR AMIRGADH 24020100113 ADIJATI U.B. ASHRAMSHALA, AMIRGADH 5 BANAS KANTHA AMIRGADH KIDOTAR UPLOBANDH 24020100202 ADIVASI ASRAM PRI. SCH 6 BANAS KANTHA AMIRGADH KIDOTAR JORAPUR 24020100402 ADARSH NIVASI SCHOOL, JORAPURA 7 BANAS KANTHA AMIRGADH BALUNDRA KAPASIYA 24020101903 SARKARI MADHYAMIK SCHOOL, KAPASIYA 8 BANAS KANTHA AMIRGADH DABHELA AVAL 24020102402 SURYABA BHAMADIRA HIGH. SEC. SCHOOL 9 BANAS KANTHA AMIRGADH IQBALGATH IQBALGADH 24020103103 SWASTIK PRI. SCH. 10 BANAS KANTHA AMIRGADH IQBALGATH IQBALGADH 24020103107 ADIVASI VIDHYALAY, IQBALGADH 11 BANAS KANTHA AMIRGADH IQBALGATH IQBALGADH 24020103108 AGRASEN SEC. & HIGH. SEC. KANYA VIDHYALAY 12 BANAS KANTHA AMIRGADH IQBALGATH IQBALGADH 24020103109 AGRASEN VIDHYALAY, IQBALGADH 13 BANAS KANTHA AMIRGADH IQBALGATH ZANZARVA 24020103403 U. B. ASHRAMSHALA, ZANZARVA 14 BANAS KANTHA AMIRGADH JETHI JETHI 24020104302 EKLAVYA GIRLS RESIDENTIAL SCHOOL, JETHI 15 BANAS KANTHA AMIRGADH SAROTRA SAROTRA 24020104903 SHIVAM VIDHYALAY, SAROTRA ROAD 16 BANAS KANTHA AMIRGADH SAROTRA SAROTRA 24020104904 EKLAVYA GIRLS RESIDENTIAL SCHOOL, SAROTRA 17 BANAS KANTHA AMIRGADH KHARA KHARA 24020105602 GOVT. SECONDARY SCHOOL, KHARA 18 BANAS KANTHA AMIRGADH RAMPURA(V) DABHELI 24020106602 GOVT. HIGH SCHOOL, DABHELI 19 BANAS KANTHA AMIRGADH RAMPURA(V) KHEMRAJIYA 24020107202 ADIJATI KANYA U.B. ASHRAMSHALA, KHEMRAJIYA 20 BANAS KANTHA AMIRGADH VIRAMPUR VIRAMPUR 24020107305 LOK NIKETAN VINAYMANDIR, VIRAMPUR 21 BANAS KANTHA AMIRGADH KANPURA UPLAGHODA 24020107602 GOVT.