Tobacco Use Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Smoking Cessation Treatment at Substance Abuse Rehabilitation Programs
SMOKING CEssATION TREATMENT AT SUBSTANCE ABUSE REHABILITATION PROGRAMS Malcolm S. Reid, PhD, New York University School of Medicine, Department of Psychiatry; Jeff Sel- zer, MD, North Shore Long Island Jewish Healthcare System; John Rotrosen, MD, New York University School of Medicine, Department of Psychiatry Cigarette smoking is common among persons with drug and alcohol n Nicotine is a highly use disorders, with prevalence rates of 80-90% among patients in sub- addictive substance stance use disorder treatment programs. Such concurrent smoking may that meets all of produce adverse behavioral and medical problems, and is associated the criteria for drug with greater levels of substance use disorder. dependence. CBehavioral studies indicate that the act of cigarette smoking serves as a cue for drug and alcohol craving, and the active ingredient of cigarettes, nicotine, serves as a primer for drug and alcohol abuse (Sees and Clarke, 1993; Reid et al., 1998). More critically, longitudinal studies have found tobacco use to be the number one cause of preventable death in the United States, and also the single highest contributor to mortality in patients treated for alcoholism (Hurt et al., 1996). Nicotine is a highly addictive substance that meets all of the criteria for drug dependence, and cigarette smoking is an especially effective method for the delivery of nicotine, producing peak brain levels within 15-20 seconds. This rapid drug delivery is one of a number of common properties that cigarette smok- ing shares with hazardous drug and alcohol use, such as the ability to activate the dopamine system in the reward circuitry of the brain. -

Alcohol, Tobacco, and Prescription Drugs: the Relationship with Illicit Drugs in the Treatment of Substance Users
Macquarie University ResearchOnline This is the author version of an article published as: Teesson, M., Farrugia, P., Mills, K., Hall, W., & Baillie, A. (2012). Alcohol, tobacco, and prescription drugs: The relationship with illicit drugs in the treatment of substance users. Substance use & misuse, Vol. 47, Issue 8-9, p. 963-971. Access to the published version: http://doi.org/10.3109/10826084.2012.663283 Copyright: Copyright the Publisher 2012. Version archived for private and non- commercial use with the permission of the author/s and according to publisher conditions. For further rights please contact the publisher. Comorbidity 1 Alcohol, tobacco and prescription drugs: The relationship with illicit drugs in the treatment of substance users. Maree Teesson, Philippa Farrugia, Katherine Mills 1 Wayne Hall2, Andrew Baillie3. 1. National Drug and Alcohol Research Centre, University of New South Wales, Sydney, New South Wales 2052 Australia, 2. University of Queensland Centre for Clinical Research, 3. Centre for Emotional Health, Department of Psychology, Macquarie University. * Corresponding author: Maree Teesson National Drug and Alcohol Research Centre University of New South Wales, Sydney New South Wales 2052 Australia Tel: +61 2 9385 0333; fax: +61 2 9385 0222; email: [email protected] Abstract Alcohol, tobacco, prescription drug and illicit drug use frequently co-occur. This paper reviews the extent of this co-occurrence in both general population samples and clinical samples, and its impact on treatment outcome. We argue that the research base for understanding comorbidity between tobacco, alcohol, prescription and illicit drugs needs to be broadened. We specifically advocate for: 1) more epidemiological studies of relationships between alcohol, tobacco and other illicit drug use; and 2) increased research on treatment options that address the problematic use of all of these drugs. -

Concurrent Alcohol and Tobacco Dependence
Concurrent Alcohol and Tobacco Dependence Mechanisms and Treatment David J. Drobes, Ph.D. People who drink alcohol often also smoke and vice versa. Several mechanisms may contribute to concurrent alcohol and tobacco use. These mechanisms include genes that are involved in regulating certain brain chemical systems; neurobiological mechanisms, such as cross-tolerance and cross-sensitization to both drugs; conditioning mechanisms, in which cravings for alcohol or nicotine are elicited by certain environmental cues; and psychosocial factors (e.g., personality characteristics and coexisting psychiatric disorders). Treatment outcomes for patients addicted to both alcohol and nicotine are generally worse than for people addicted to only one drug, and many treatment providers do not promote smoking cessation during alcoholism treatment. Recent findings suggest, however, that concurrent treatment for both addictions may improve treatment outcomes. KEY WORDS: comorbidity; AODD (alcohol and other drug dependence); alcoholic beverage; tobacco in any form; nicotine; smoking; genetic linkage; cross-tolerance; AOD (alcohol and other drug) sensitivity; neurotransmitters; brain reward pathway; cue reactivity; social AODU (AOD use); cessation of AODU; treatment outcome; combined modality therapy; literature review lcohol consumption and tobacco ers who are dependent on nicotine Department of Health and Human use are closely linked behaviors. have a 2.7 times greater risk of becoming Services 1989). The concurrent use of A Thus, not only are people who alcohol dependent than nonsmokers both drugs by pregnant women can drink alcohol more likely to smoke (and (e.g., Breslau 1995). Finally, although also result in more severe prenatal dam- vice versa) but also people who drink the smoking rate in the general popula age and neurocognitive deficits in their larger amounts of alcohol tend to smoke tion has gradually declined over the offspring than use of either drug alone more cigarettes. -

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -

Barriers and Solutions to Addressing Tobacco Dependence in Addiction Treatment Programs
Barriers and Solutions to Addressing Tobacco Dependence in Addiction Treatment Programs Douglas M. Ziedonis, M.D., M.P.H.; Joseph Guydish, Ph.D., M.P.H.; Jill Williams, M.D.; Marc Steinberg, Ph.D.; and Jonathan Foulds, Ph.D. Despite the high prevalence of tobacco use among people with substance use disorders, tobacco dependence is often overlooked in addiction treatment programs. Several studies and a meta-analytic review have concluded that patients who receive tobacco dependence treatment during addiction treatment have better overall substance abuse treatment outcomes compared with those who do not. Barriers that contribute to the lack of attention given to this important problem include staff attitudes about and use of tobacco, lack of adequate staff training to address tobacco use, unfounded fears among treatment staff and administration regarding tobacco policies, and limited tobacco dependence treatment resources. Specific clinical-, program-, and system-level changes are recommended to fully address the problem of tobacco use among alcohol and other drug abuse patients. KEY WORDS: Alcohol and tobacco; alcohol, tobacco, and other drug (ATOD) use, abuse, dependence; addiction care; tobacco dependence; smoking; secondhand smoke; nicotine; nicotine replacement; tobacco dependence screening; tobacco dependence treatment; treatment facility-based prevention; co-treatment; treatment issues; treatment barriers; treatment provider characteristics; treatment staff; staff training; AODD counselor; client counselor interaction; smoking cessation; Tobacco Dependence Program at the University of Medicine and Dentistry of New Jersey obacco dependence is one of to the other. The common genetic vul stance use was considered a potential the most common substance use nerability may be located on chromo trigger for the primary addiction. -

Cocaine Use Disorder
COCAINE USE DISORDER ABSTRACT Cocaine addiction is a serious public health problem. Millions of Americans regularly use cocaine, and some develop a substance use disorder. Cocaine is generally not ingested, but toxicity and death from gastrointestinal absorption has been known to occur. Medications that have been used as substitution therapy for the treatment of a cocaine use disorder include amphetamine, bupropion, methylphenidate, and modafinil. While pharmacological interventions can be effective, a recent review of pharmacological therapy for cocaine use indicates that psycho-social efforts are more consistent over medication as a treatment option. Introduction Cocaine is an illicit, addictive drug that is widely used. Cocaine addiction is a serious public health problem that burdens the healthcare system and that can be destructive to individual lives. It is impossible to know with certainty the extent of use but data from public health surveys, morbidity and mortality reports, and healthcare facilities show that there are millions of Americans who regularly take cocaine. Cocaine intoxication is a common cause for emergency room visits, and it is one drug that is most often involved in fatal overdoses. Some cocaine users take the drug occasionally and sporadically but as with every illicit drug there is a percentage of people who develop a substance use disorder. Treatment of a cocaine use disorder involves psycho-social interventions, pharmacotherapy, or a combination of the two. 1 ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com ce4less.com Pharmacology of Cocaine Cocaine is an alkaloid derived from the Erthroxylum coca plant, a plant that is indigenous to South America and several other parts of the world, and is cultivated elsewhere. -

Alcohol Use Disorder
Section: A B C D E Resources References Alcohol Use Disorder (AUD) Tool This tool is designed to support primary care providers (family physicians and primary care nurse practitioners) in screening, diagnosing and implementing pharmacotherapy treatments for adult patients (>18 years) with Alcohol Use Disorder (AUD). Primary care providers should routinely offer medication for moderate and severe AUD. Pharmacotherapy alone to treat AUD is better than no therapy at all.1 Pharmacotherapy is most effective when combined with non-pharmacotherapy, including behavioural therapy, community reinforcement, motivational enhancement, counselling and/or support groups. 2,3 TABLE OF CONTENTS pg. 1 Section A: Screening for AUD pg. 7 Section D: Non-Pharmacotherapy Options pg. 4 Section B: Diagnosing AUD pg. 8 Section E: Alcohol Withdrawal pg. 5 Section C: Pharmacotherapy Options pg. 9 Resources SECTION A: Screening for AUD All patients should be screened routinely (e.g. annually or when indicators are observed) with a recommended tool like the AUDIT. 2,3 It is important to screen all patients and not just patients eliciting an index of suspicion for AUD, since most persons with AUD are not recognized. 4 Consider screening for AUD when any of the following indicators are observed: • After a recent motor vehicle accident • High blood pressure • Liver disease • Frequent work avoidance (off work slips) • Cardiac arrhythmia • Chronic pain • Rosacea • Insomnia • Social problems • Rhinophyma • Exacerbation of sleep apnea • Legal problems Special Patient Populations A few studies have reviewed AUD in specific patient populations, including youth, older adults and pregnant or breastfeeding patients. The AUDIT screening tool considered these populations in determining the sensitivity of the tool. -
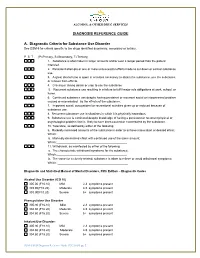
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

Evidence-Based Guidelines for the Pharmacological Management of Substance Abuse, Harmful Use, Addictio
444324 JOP0010.1177/0269881112444324Lingford-Hughes et al.Journal of Psychopharmacology 2012 BAP Guidelines BAP updated guidelines: evidence-based guidelines for the pharmacological management of substance abuse, Journal of Psychopharmacology 0(0) 1 –54 harmful use, addiction and comorbidity: © The Author(s) 2012 Reprints and permission: sagepub.co.uk/journalsPermissions.nav recommendations from BAP DOI: 10.1177/0269881112444324 jop.sagepub.com AR Lingford-Hughes1, S Welch2, L Peters3 and DJ Nutt 1 With expert reviewers (in alphabetical order): Ball D, Buntwal N, Chick J, Crome I, Daly C, Dar K, Day E, Duka T, Finch E, Law F, Marshall EJ, Munafo M, Myles J, Porter S, Raistrick D, Reed LJ, Reid A, Sell L, Sinclair J, Tyrer P, West R, Williams T, Winstock A Abstract The British Association for Psychopharmacology guidelines for the treatment of substance abuse, harmful use, addiction and comorbidity with psychiatric disorders primarily focus on their pharmacological management. They are based explicitly on the available evidence and presented as recommendations to aid clinical decision making for practitioners alongside a detailed review of the evidence. A consensus meeting, involving experts in the treatment of these disorders, reviewed key areas and considered the strength of the evidence and clinical implications. The guidelines were drawn up after feedback from participants. The guidelines primarily cover the pharmacological management of withdrawal, short- and long-term substitution, maintenance of abstinence and prevention of complications, where appropriate, for substance abuse or harmful use or addiction as well management in pregnancy, comorbidity with psychiatric disorders and in younger and older people. Keywords Substance misuse, addiction, guidelines, pharmacotherapy, comorbidity Introduction guidelines (e.g. -
Treatment of Patients with Substance Use Disorders Second Edition
PRACTICE GUIDELINE FOR THE Treatment of Patients With Substance Use Disorders Second Edition WORK GROUP ON SUBSTANCE USE DISORDERS Herbert D. Kleber, M.D., Chair Roger D. Weiss, M.D., Vice-Chair Raymond F. Anton Jr., M.D. To n y P. G e o r ge , M .D . Shelly F. Greenfield, M.D., M.P.H. Thomas R. Kosten, M.D. Charles P. O’Brien, M.D., Ph.D. Bruce J. Rounsaville, M.D. Eric C. Strain, M.D. Douglas M. Ziedonis, M.D. Grace Hennessy, M.D. (Consultant) Hilary Smith Connery, M.D., Ph.D. (Consultant) This practice guideline was approved in December 2005 and published in August 2006. A guideline watch, summarizing significant developments in the scientific literature since publication of this guideline, may be available in the Psychiatric Practice section of the APA web site at www.psych.org. 1 Copyright 2010, American Psychiatric Association. APA makes this practice guideline freely available to promote its dissemination and use; however, copyright protections are enforced in full. No part of this guideline may be reproduced except as permitted under Sections 107 and 108 of U.S. Copyright Act. For permission for reuse, visit APPI Permissions & Licensing Center at http://www.appi.org/CustomerService/Pages/Permissions.aspx. AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES John S. McIntyre, M.D., Chair Sara C. Charles, M.D., Vice-Chair Daniel J. Anzia, M.D. Ian A. Cook, M.D. Molly T. Finnerty, M.D. Bradley R. Johnson, M.D. James E. Nininger, M.D. Paul Summergrad, M.D. Sherwyn M. -

Substance Use Disorder Defined by NIDA and SAMHSA
Substance Use Disorder defined by NIDA and SAMHSA: NIDA (National Institute on Drug Abuse) defines SUD/Addiction as: What is drug addiction? Addiction is defined as a chronic, relapsing disorder characterized by compulsive drug seeking, continued use despite harmful consequences, and long-lasting changes in the brain. It is considered both a complex brain disorder and a mental illness. Addiction is the most severe form of a full spectrum of substance use disorders, and is a medical illness caused by repeated misuse of a substance or substances. Why study drug use and addiction? Use of and addiction to alcohol, nicotine, and illicit drugs cost the Nation more than $740 billion a year related to healthcare, crime, and lost productivity.1,2 In 2016, drug overdoses killed over 63,000 people in America, while 88,000 died from excessive alcohol use.3,4 Tobacco is linked to an estimated 480,000 deaths per year.5 (Hereafter, unless otherwise specified, drugs refers to all of these substances.) How are substance use disorders categorized? NIDA uses the term addiction to describe compulsive drug seeking despite negative consequences. However, addiction is not a specific diagnosis in the fifth edition of The Diagnostic and Statistical Manual of Mental Disorders (DSM-5)—a diagnostic manual for clinicians that contains descriptions and symptoms of all mental disorders classified by the American Psychiatric Association (APA). In 2013, APA updated the DSM, replacing the categories of substance abuse and substance dependence with a single category: substance use disorder, with three subclassifications—mild, moderate, and severe. The symptoms associated with a substance use disorder fall into four major groupings: impaired control, social impairment, risky use, and pharmacological criteria (i.e., tolerance and withdrawal). -

Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender
Opioid and Nicotine: Influences of Sex and Gender Conference Report: Opioid and Nicotine Use, Dependence, and Recovery: Influences of Sex and Gender Authors: Bridget M. Nugent, PhD. Staff Fellow, FDA OWH Emily Ayuso, MS. ORISE Fellow, FDA OWH Rebekah Zinn, PhD. Health Program Coordinator, FDA OWH Erin South, PharmD. Pharmacist, FDA OWH Cora Lee Wetherington, PhD. Women & Sex/Gender Differences Research Coordinator, NIH NIDA Sherry McKee, PhD. Professor, Psychiatry; Director, Yale Behavioral Pharmacology Laboratory Jill Becker, PhD. Biopsychology Area Chair, Patricia Y. Gurin Collegiate Professor of Psychology and Research Professor, Molecular and Behavioral Neuroscience Institute, University of Michigan Hendrée E. Jones, Professor, Department of Obstetrics and Gynecology; Executive Director, Horizons, University of North Carolina at Chapel Hill Marjorie Jenkins, MD, MEdHP, FACP. Director, Medical Initiatives and Scientific Engagement, FDA OWH Acknowledgements: We would like to acknowledge and extend our gratitude to the meeting’s speakers and panel moderators: Mitra Ahadpour, Kelly Barth, Jill Becker, Kathleen Brady, Tony Campbell, Marilyn Carroll, Janine Clayton, Wilson Compton, Terri Cornelison, Teresa Franklin, Maciej Goniewcz, Shelly Greenfield, Gioia Guerrieri, Scott Gottlieb, Marsha Henderson, RADM Denise Hinton, Marjorie Jenkins, Hendrée Jones, Brian King, George Koob, Christine Lee, Sherry McKee, Tamra Meyer, Jeffery Mogil, Ann Murphy, Christine Nguyen, Cheryl Oncken, Kenneth Perkins, Yvonne Prutzman, Mehmet Sofuoglu, Jack Stein, Michelle Tarver, Martin Teicher, Mishka Terplan, RADM Sylvia Trent-Adams, Rita Valentino, Brenna VanFrank, Nora Volkow, Cora Lee Wetherington, Scott Winiecki, Mitch Zeller. We would also like to thank those who helped us plan this program. Our Executive Steering Committee included Ami Bahde, Carolyn Dresler, Celia Winchell, Cora Lee Wetherington, Jessica Tytel, Marjorie Jenkins, Pamela Scott, Rita Valentino, Tamra Meyer, and Terri Cornelison.